-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2017; 6(2): 15-25
doi:10.5923/j.cp.20170602.01

Implications of Nurse's Moral Distress Experience in Clinical Practice and Their Health Status in Obstetrics and Critical Care Settings
Shereen Ahmed Ahmed Qalawa 1, Hanan Elzeblawy Hassan 2
1Department of Medical Surgical Nursing, Faculty of Nursing, Port Said University, Port Said, Egypt
2Department of Maternal & Newborn Health Nursing, Faculty of Nursing, Beni-Suef University, Beni-Suef, Egypt
Correspondence to: Hanan Elzeblawy Hassan , Department of Maternal & Newborn Health Nursing, Faculty of Nursing, Beni-Suef University, Beni-Suef, Egypt.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

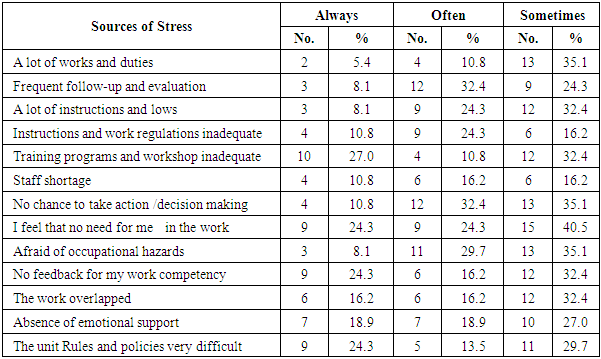
Background: Professional stress or moral distress is a common issue that may has an adverse effect on patients and nurses, moreover, the healthcare system as a whole. There are high levels of human contact with the nursing profession. Aim: assess the implications of nurses' moral distress experience in clinical practice and their health status in maternal and medical-surgical critical care settings. Methods: This is a cross-section descriptive study, including nurses selected from obstetrics and medical-surgical critical care units at all governmental hospital in Beni-Suef City, Egypt. Four tools were used for data collection: a self-administered questionnaire, Moral Distress Experience Scale, health status assessment sheet, and work stress assessment sheet. Results: 24.3% of nurses perceived that they are useless in the work, no feedback for their work competency and difficulty of unit rules and policies are always the sources of work stress while 32.4% of them often seen that no chance to take action/decision making are often work stress for them. 77.2% of nurses usually complaint of insomnia, while 66.6% & 66.5% often complain of a headache and indigestion, respectively, 61.2% often complaint of arthralgia and tachycardia as nurse perceived. Conclusion: A negative correlation was found between the nurse's attitude of moral distress, the source of work stress and their health status, there are significant relations were found between nurses' work stress and their age, and between nurses' health status and their years of experience. Recommendations: Further studies should be undertaken on the effect of preventive measures for moral distress on clinical nursing practice and nurses' health status in non-critical areas and large sample size to generalize the result of study to improve their preventive attitude regarding moral distress, work stressors in numerous geographical zones to explore the confounding that hinder nurse's optimal general health.
Keywords: Implications, Moral Distress, Nurses, Critical Care Settings
Cite this paper: Shereen Ahmed Ahmed Qalawa , Hanan Elzeblawy Hassan , Implications of Nurse's Moral Distress Experience in Clinical Practice and Their Health Status in Obstetrics and Critical Care Settings, Clinical Practice, Vol. 6 No. 2, 2017, pp. 15-25. doi: 10.5923/j.cp.20170602.01.
Article Outline
1. Introduction
- Critical-care nursing is that sub-specialty of nursing sciences that deals, particularly, with human responses to life-threatening issues. Critical-care nurses are the skilled licensed nurses who are in charge of guaranteeing that all critically sick patients & their families receive the best and the optimal care. Within the hospital setting, critical-care nurses are found, in a wide assortment of specialties and environments wherever there are critically sick patients such as trauma intensive care unit, burn unit, surgical serious care unit, cardiothoracic intensive care unit, cardiac care unit, intensive care unit for internal medicine, intensive-care units (ICUs), progressive care units as well as recovery rooms, and emergency departments. [1, 2] No specialty to fame is more immersed with emergencies than obstetrics. Obstetrical emergencies are more common in form of ectopic pregnancy associated with shock, acute abdominal pain through pregnancy period, premature birth associated with hemorrhagic shock, abdominal pregnancy, antepartum hemorrhage, cardiopulmonary resuscitation (CPR) during pregnancy, severe preeclampsia, eclampsia, amniotic fluid embolism, premature rupture of membranes, prolapsed umbilical cord, shoulder dystocia, preterm labor, cesarean section with local or no anesthesia, retained placenta, uterine inversion, trauma, Disseminated Intravascular Coagulation (DIC), postpartum hemorrhage, postmortem cesarean section, and what's more, the transportation of the obstetric patient. [3, 4] Obstetric admission to the emergency and ICU units & maternal mortality continues to be critically affecting maternal medicinal services. Not at all like others, the obstetric patients represent a major management challenge to the ICU team due to the altered physiology during their pregnancy, consideration of fetal wellbeing, & the unique type of disorders to be dealt with. [5] Despite the advances in the obstetrical care, admission rate to the emergency units had multiplied compared with a decade ago. The most causes for admission in intensive care units (ICU) are listed in as the following: (1) postpartum & obstetric problems, postpartum hemorrhage (PPH) were the leading cause followed by preeclamptic toxemia (PET) or eclampsia. (2) Moreover, non-obstetric reasons for admitted to the ICU as seizure, epileptic fits, cardiovascular problems "pulmonary hypertension, heart failure, and cardiomyopathy", acute pulmonary edema, Ethanol toxicity, myasthenia gravis, renal diseases, and anaphylactic shock. [5]Basic care for the patient includes; the ABCs of resuscitation (airway patency, breathing, and circulation). The patient ought to be evaluated quickly, taking history and patient's physical examination should be performed as quickly as possible. If the patient in shock or vital signs are unstable, intravenous access should be obtained, and 2 large bore IVs placed. What laboratory & radiographic studies are needed? if there is active bleeding, does the patient (and baby) need oxygen? What amount of blood does the blood bank have at this institution? [3]Nursing is viewed as an associate inherently stressful occupation, as nurses expect not exclusively the role of caregivers, supervisors for their patients, & administrators, however, additionally they become strong advocates, role models as well as educators for his or her families, work environments, and their communities. These multiple and different work roles expose them to much work-related stress, including the requests of the patients, the experience of long working hours and death. [6-8]The phenomenon of moral distress has been generally investigated in different clinical settings in which nurse's practice. After a broad reviewing literature, there were little researches perceived that concentrated on moral distress among nurses in continuing care settings. [9] Additionally, the event of moral distress may involve different repercussions for nurse, patient, and healthcare organizations. In confronting these conditions, nurses may encounter pity, inconsistency, worthlessness, and tribulation. Prolongation of these conditions may lead to prompt fatigue of their resistance assets and cause disappointment and dissatisfaction with the work environment. Stress is a well-known phenomenon in the nursing profession that may involve negative and positive consequences. Professional stress can be created under various conditions such as moral distress, nursing shortages, and organizational limitations as well as authoritative impediments, and affect nurse directly, followed by the patient and finally the all healthcare system. [10] Additionally, Studies have revealed that the stress among staff attendants is caused by significant workload, role clashes, shift schedule, social issues, inadequate preparation, violent attacks, and uncertainty about treatment outcome. [11] Furthermore, nurse who work in exceedingly unpleasant situations such as critical care unit, is particularly defenseless against the harmful impacts of burnout. Recent advances in technology & changes in medicinal services methods & conveyance in those units have just added new obligations and responsibilities to the attendant's traditional role as a caregiver and the patient’s advocate. It is very common for attendants who work in such units encounter a lot of stress since they are mindful on an everyday basis for the welfare of patients who are dependent on critical life support procedures & technology and for patients frequently in a condition of terminal or useless care. [12]Critical care nurses are repeatedly bombarded with auditory stimulation from alarming monitoring devices, mechanical ventilation equipment, and infusion devices. Endless phone calls from families, physicians, and ancillary departments disrupt care for their patients. Intuitive recognition of acute changes in a patient's status demands vigilance. Life-supporting technological advances require critical care nurses to acquire an extensive knowledge base and maintain the ability to make split-second decisions. [13]Moral distress is present among maternity and medical-surgical critical care attendants related to end of life care and is related to moral atmosphere and strengthening. Profoundly enabled nurse working in a positive moral atmosphere are probably going to encounter less moral distress. The presence of palliative care team does not equate with sufficient usage or all around incorporated palliative care conveyance. Essential palliative care education for ICU nurses may add to less moral distress when consolidated with well-integrated care teams and positive ethical climates. [14]A few main drivers of moral distress have been perceived in the literature. Some main drivers are externally focused. Regular cases incorporate administration of medically inappropriate treatment and concerns about communication between healthcare services providers or between patients and health services providers. The ethical climate in which clinicians work-determined by the institutional system in place to resolve ethical issues may heavily influence moral distress, although the nature of its influence remains uncertain. Internal considerations include feelings of powerlessness or perceptions of power differentials between healthcare providers. [15] On the other hand, for the impact of moral distress on nurses' manners in clinical Practice, Borhani et al, 2014, nested that leaving the profession can have different effects on the healthcare system. [10] Shortage of skilled human resources (HR) can cause a decrease in the quality of care and cause financial and legal challenges for the health service providers, and in an endless loop, increment moral trouble & professional stress in the rest of the nurses. Likewise, moral distress may indirectly affect the quality of the care which provided by nurses & cause nurses to avoid facing the patients in need of quality care and impacts of distress on organizations is associated with work abdications, diminished occupation fulfillment and quality & nature of care. They likewise expressed that the intensity & recurrence of moral troubles are distinctive in various situations.
1.1. Significance of the Study
- Nurses having a vital role in the system of health care as well as play an essential role in collaboration with other different health professions to determine the effectiveness of treatment. They are considered to be members of a stressful job as a profession because of they care for an upsetting group comprising patients or those at health hazard. [16-18]In the case that the nurses working in the critical care unit, many circumstances like crucial and critical decision-making, managing the therapy having a serious aspect of adverse effects, patients’ problems with anger & disobedience with therapy, monitoring patient suffering and has pain &, terminal care, stressful situations experienced in connection with the death of patient, emotional difficulties with patients & conflicts inside the team may cause stress. Burnout syndrome frequently happens because of endless work stress found in these units. [19]Nursing could be a skilled occupation portrayed by higher moral distress than others. Stress might be associated with routine with regards to wellbeing advancing practices; however, no study has explored the moral distress among nurses working in critical care units of obstetrics and medical surgical departments in Egypt. So this study aimed to: (1) Determine sources of stress as recognized by critical care nurses; (2) determine health complaint resulting from moral distress experience as recognized by critical care nurses; and (3) find out relationship between nurses' moral distress experience in clinical practice and their health status in critical care settings.
1.2. Operational Definitions
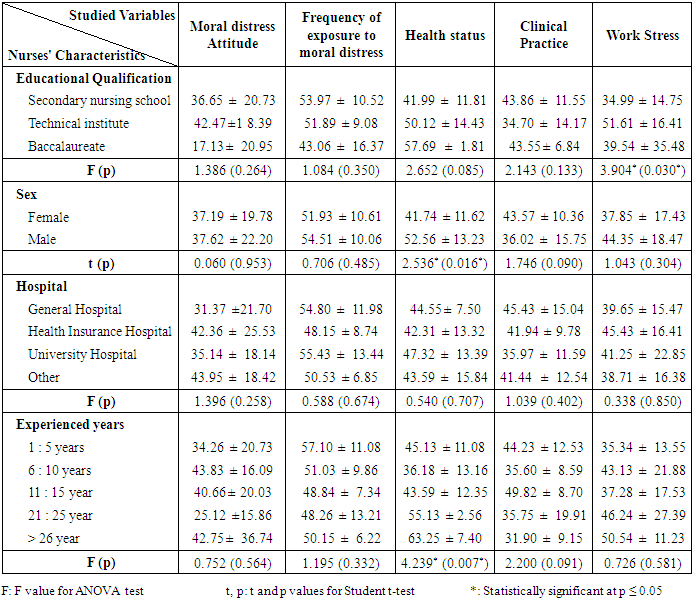
- Critical care nursing is defined as the field of nursing with an attention on the most extreme care of the unstable or critically ill patients following extensive surgery, injury and/or life-threatening diseases. [1] Implications: The consistency in the reactions to moral distress experience among participants is remarkable and informative to those working in critical care units and for decision makers.Moral distress as defined by Leggett, 2013 is a state of the psychological disequilibrium that, ones experienced when they know the right ethical decisions to make but they can't make it because of institutional constraints. [20] Additionally, Weinzimmer, et al, 2014 characterized moral distress as a phenomenon in which a healthcare providers perceive an ethically preferable and / or morally right course of action to take, yet interior or outer requirements make it almost difficult to seek after that course. [15] Health Status: as defined in medical dictionary; A generic term for the wellbeing (good or poor) of an individual, a group or all populace in specific territory, particularly when with different ranges or with national information, which level of health soundness of a distinct person, a group or a population as assessed by that individual or by objective measures. [21] Conceptual Model for Moral distress in Nursing: Corley in 2002 proposed the hypothesis of moral distress & described it as having both internal & external contexts. [22]The external one focused on the work environment while the internal one concentrated on the psychological effect. Nursing has been depicted as an ethical job with nurses as moral agents. This hypothesis proposed 8 moral concepts used to portray moral distress through the literature. How these concepts demonstrated, interact and communicate with each other can lead to moral distress or moral intent to act? Moral distress can affect 3 levels: (1) the patient; (2) the nurse; and (3) the organization (Figure 1). [23]
 | Figure 1. Conceptual Model for Moral distress in Nursing |
1.3. Research Questions
- (1) What are sources of stress among maternal and medical surgical critical care nurses?(2) Are there health complaints resulting from moral distress experience by critical care nurses? What are they?(3) Is there is correlation between nurses' moral distress in clinical practice & their health status in critical care settings?(4) Is there gender difference existing in the moral distress scores?
2. Subjects and Methods
2.1. Research Design
- A descriptive cross-section design was used in the current study.
2.2. Study Setting
- This study was carried out in Beni-Suef city at critical care units, in obstetrics (emergencies, intensive care unit (ICU) and critical care units) and medical surgical departments (emergency, intensive care, Burn, dialysis, oncology), at University Hospital, Health Insurance Hospital and Ministry of Health General Hospital.
2.3. Subjects
- Convenient sample was selected from the available nurses worked in the above mentioned setting. While there are 56 nurse in service at maternity and medical surgical previously mentioned critical settings, 37 consented to take an interest in the study, representing 66.1% of them.
2.3.1. Inclusion Criteria
- Ÿ At least one year of experience in obstetrics or medical surgical emergency and/or critical care units.
2.3.2. Exclusion Criteria
- Ÿ Partnership nursing attendants.Ÿ Administrative nursesŸ Nursing students.
2.4. Tools of Collection the Data
- Data collected by using adopted 4 tools.
2.4.1. Tool I: Self-administered Questionnaire
- It is consisted of two parts as the followings:Part i: Socio-demographic data that include age, educational levels, ………etc.Part ii: critical care units' background variables: It was contained number of working hours in the unit, working preferable shift, total number of patients in charge of, numbers of patients who admitted to the unit, numbers of isolated patients, numbers of daily discharge patient, numbers of assistant nurses; clerk, & work environment.
2.4.2. Tool II: Moral Distress Experience Scale
- It includes 36 question Likert items to measure both the intensity & frequency of experience moral distress and its implications for nursing practice. The instrument adopted, valid & reliable from Corley, et al., 2001 and Aft, 2011. [24, 23] As moral distress experience and its occurrence numbers which ranged from 0 to 6 as 0 no experience and 6 for high experience and occurrence.
2.4.3. Tool III: Work Stress Assessment Questionnaire
- It adopted from Villiers, 2010 includes stress Likert scale with 32 questions to determine sources of work stress as nurses perceived which the instrument adopted, valid and reliable had 4 selective options ranged from the usually source of stress, sometimes the source of stress, all the time's source of stress, rarely source of stress respectively. [25]
2.4.4. Tool V: Health Status Assessment Sheet
- It includes 13 Likert scale items developed by Hart, 2009 adopted, valid and reliable to determine nurses' health status through assess symptoms associated with moral distress that nurses had as insomnia, arthralgia, dyspnea, anorexia, tachycardia and others which had 4 selective options ranged from usually, sometimes, all the times, rarely respectively. [9]
2.5. Pilot Study
- A pilot examine was done after the improvement of the tools on 4 nurses (10% of attendants) to evaluate the applicability of all tools, then necessary modification was done according to its result and expertise opinions. Otherwise, these nurses were then excluded from the sample of research work to guarantee the strength and stability of the answers.
2.6. Ethical Considerations
- Formal endorsement was taken from the dean of nursing college and hospital director. A concise clarification of the reason & significance of the study given to the nurses & guaranteed that the acquired data will be secret and utilized just for the goal of the study. Secrecy of the data was guaranteed by the researchers.
2.7. Methods of Data Collection
- A structured questionnaire was filled out independently and individually with the attendants. Collecting of information was carried out from the choosing settings by the researcher utilizing the developed tools; the data were gathered inside 6 months which began from February 2016 to July 2016. Each nurse was individually met and filled the questionnaire; the data collection from all the nurses throughout 2 days' week, the purpose of the study was disclosed before get the questionnaire sheet, & it appropriated to be replied inside thirty to fifty minutes then collected.
2.8. Statistical Analysis
- Data were gathered, spared & saved in a database record. Statistical analysis took place by the SPSS 19 PC programming measurable bundle "software statistical package". Data were illustrated and summarized by tables and figures, "Chi-2" was utilized to evaluate the correlation between 2 qualitative variables & "t test" were utilized to compare between 2 or more proportions and "person test" for correlation coefficient between variables. Measurable Statistical significant level was considered at P-value less than 0.05 and highly significance at P-value less than 0.001.
3. Results
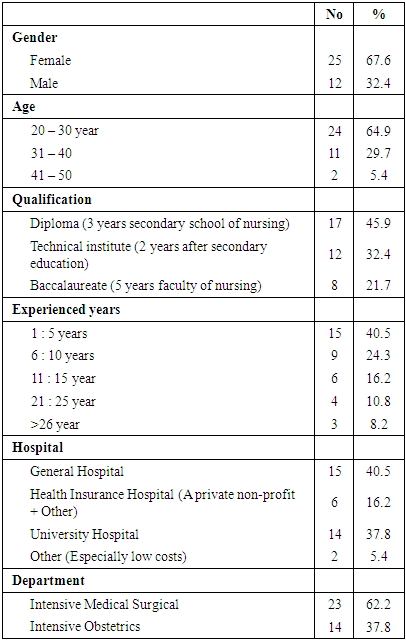
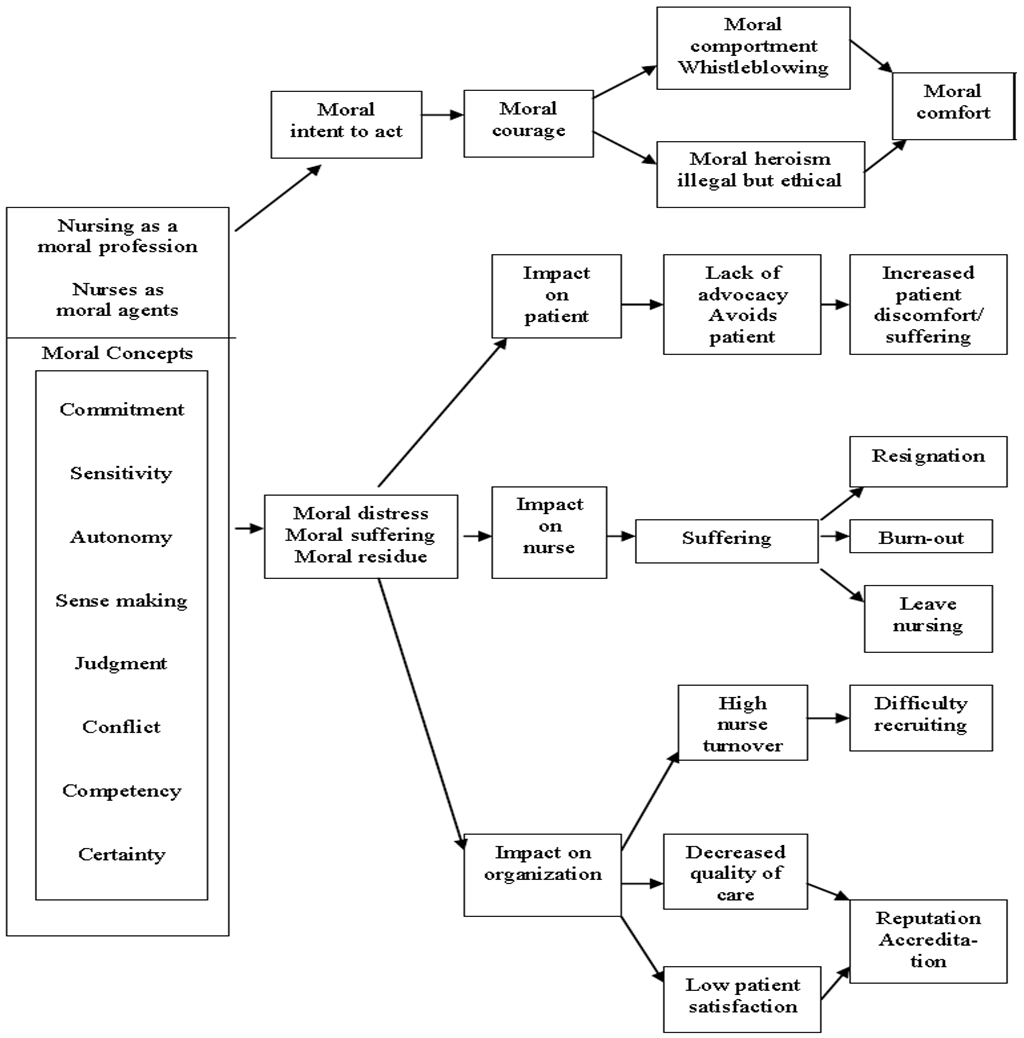
- Table (1): illustrates that more than two-thirds (67.6%) of subject were females, about one-third (64.9%) in the age group between 20-30 years and 45.9% had secondary nursing school qualification, 40.5% had below five years-experience in critical nursing work, 37.8% worked in intensive & emergency obstetrics unit while 62.2% worked in Intensive and Emergency Medical Surgical unit.
|
|
|
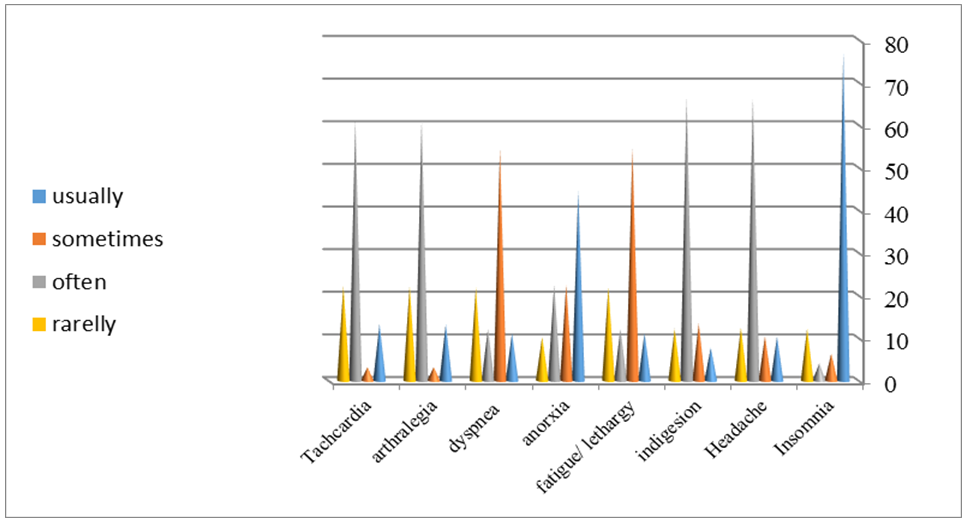 | Figure (2). Distribution of health problems / complaint as nurses perceived (N = 37) |
|
|
4. Discussion
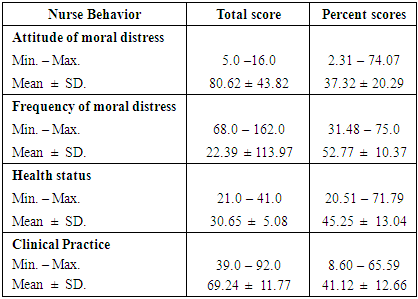
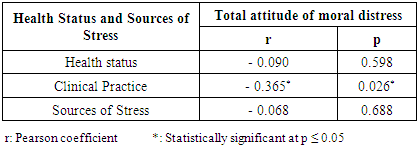
- A review an expansive sample of nurses found that more than 80% of the nurses announced high to terribly high job stress. Moreover, a review among the personnel of a United Kingdom health authority announced that nurses were under the greatest stress among all health care members. [26] Stress among the profession of nursing has been the most significant worldwide issues for a long while presently. [11] The concept of moral distress has conveyed a substantively different strategy for seeing a part of the inconveniences and troubles confronted by nurses in their practices. This concept highlights that nurse's distress may be an indication of nurse's conscientious moral engagement with her expert and professional practices that have confronted practices or an environmental situation that impedes them from acting as per their own specific moral principles and ethical standards. Moral distress might be a marker of problems in nurses' practices environments. This concept is depicted, identified, described & related to moral agency in nursing practice. [15] Professional stress and moral distress are considered common problems that effectsly affect negatively patients, and nurses, as well as the healthcare system as a whole. There are high levels of human contact in the profession of nursing, therefore, nurses are unavoidably confronted with issues like professional stress and moral distress. Moral distress is created when the conditions repudiate a person's convictions & inner moral values, and & he/she needs to act against those values as a result of those conditions and genuine limitations. The event of moral distress can involve distinctive repercussions for nurses, patients, and healthcare organizations. In confronting these conditions, the nurse may encounter sadness, trouble, contradiction, futility, & distress. Prolonging this condition leads to exhaustion of their resistance resources and cause disappointment and dissatisfaction with the workplace. The individuals who keep on working regardless of these conditions encounter stress and burnout alongside disappointment. [10] Traditionally, the profession of nursing has held an elevated expectation of ethical practice & moral behavior. Frequently, nurses in their clinical practices report the distress they experience when a standard that they have faith in is compromised in some designs. Different circumstances this distress occurs when the nurse does not trust that the treatment and medication is given to the patient is of the greatest interest or advantage of the patient, or does not mesh with the nurse’s sense of good & bad or right & wrong. Nurse instructors, through recounted discussions, conversations & comments, have shared with this author the moral distress they have encountered when the administration of their instructive unit settles on a choice they don't feel is in the best interest of the student nurse or the profession ones. These situations, albeit anecdotal, represent narrative cases of moral distress in nursing education. [27] As regarding the sociodemographic characteristics of the studied sample, the results of the current study illustrated that more than two-thirds (67.6%) of the subject were females, and more than half (64.9%) of them in the age group between 20-30 years and around half (45.9%) of them had secondary school of nursing education and more than one-third (40.5%) of them had below 5 years' experience in nursing work, more than one-third (37.8%) of studied sample worked in intensive obstetrics and worked in emergency units.Concerning the sources of work stressors, the present study revealed that more than one-quarter of nurses perceived that there is no need for them in the work, no feedback for their work competency and difficulty of unit rules and policies are always the sources of work stress and more than one-quarter of them often seen that frequent follow-up and evaluation, no chance to take action/decision making are often work stress for them. According to Alvemarka, 2004 many dilemmas seem to occur due to the lack of time or personnel being forced to prioritize their time between tasks that seem equally important. If there is a patient to attend to immediately, the time & effort spent on that patient will have consequences for other patients. [28] Many encounters between the health care providers & their clients should last a certain amount of time, & spending "too much" time with one patient implies that others should wait. The patient might be sitting in a waiting list for an operation, moreover, something ought to be ready for a patient who will come in later.From another point of view Huggins, 2008 stressed on that critical incidents are commonly viewed as a difficult but realistic part of working in intensive care unit, emergency department, & the other critical care settings. [13] On a daily basis, the nurse is exposed to a variety of stressful situations while practicing in critical care settings. Some of these daily occupational stressors include pharmacy delivery and lab value reporting delays, unmet staffing needs, interdepartmental demands, and the challenges of meeting physician, patient, and family expectations. While Karla, 2007 mentioned that factors showing the highest levels of distress were related to questions concerning aggressive treatment to the terminally ill patients. [29] The lowest levels of distress related to assisting suicide indicating that this situation rarely occurs. In this concern, Krista, 2016 highlighted the need for the promotion of organizational team-building, enhanced palliative care education for ICU clinicians, as well as advancement of institutionalized palliative care delivery techniques in the ICU. [14] The present study revealed that the mean ± SD (80.62 ± 43.82) of total nurses' moral distress, (113.97 ± 22.39) for frequent experience of moral distress situations, (30.65 ± 5.08) for health status resulting from moral distress, (69.24 ± 11.77) for implication of moral distress in clinical practice. This finding goes similarly with Ameri et al, 2015 who reported from Coley in their first study of moral distress that 80% of nurses experienced moderate to exaggerated level of distress in their working environment. [30] In Swedish, Alvemarka et al, 2004 mentioned that the changes have made health care more complex & ethics has increasingly become a required component of clinical practice. Considering this, it is not amazing that numerous health care providers experienced stress-related disorders. Stress due to ethical issues is generally referred to as moral distress. [28]Additionally, moral distress is the emotional & mental distress that accompanies & results from not having the capacity to act as per one’s values, beliefs, and moral conscience. [9] Regarding the correlation between nurses' attitude of moral distress, the source of work stress and their health status, our study revealed negative correlations between nurses' attitude of moral distress, the source of work stress and their health status. This finding goes in contrast with Karla, 2007 who documented a positive perception of the ethical climate and it was strong, negatively correlated with intent to turnover. [29] Particular climate factors, for example, relationships with companions and administrators, directed the impact of moral distress levels on intent to turnover. Implications are noted for administrative intervention in these factors to diminish critical care staff turnover. In addition to, the disappointment & dissatisfaction of nurses with their workplace resulting from moral distress and professional stress can lead to increase absenteeism rate, and strengthen the thought and desire to resign and leave the profession. In addition to these conditions, restricted human resources (HR), absence of support systems for the nurse in the clinical situations, organizational pressures, and the feeling of guilt when they can't give quality care, would all cause the thought and desire to leave the profession to turn into action. [10] Regarding the distribution of health complaint as nurses perceived, the current study revealed that near three-quarters of nurses usually complaint of insomnia, while the majority of them often a complaint of a headache, indigestion, arthralgia and tachycardia. These findings go in the same line with Hart, 2009 [9] who stated that the impact of moral distress can present as feelings of pain, headache, sleep dysfunctions, tiredness, and sorrow, loss of self-esteem, anxiety, depression, powerlessness, shame, grief, dread, heartache, and anguish. Langley, et al, 2015 added that Physical symptoms of moral distress may incorporate GIT effects, headaches, palpitations, insomnia and nightmares. [31] Additionally, Brazil, Dalmolin et al, 2012 reported that the moral distress that experienced by the nurses is manifested in the personal dimension, by emotional & physical alterations, and in the professional dimension, by job dissatisfaction, work disappointment, burnout and resign from the profession. [32] The adapting methodologies are utilized as a part of three dimensions: instructive, communicative, & organizational. Physical manifestations seem to happen in the 2nd stage of moral trouble as crying spells, loss of rest & sleep, loss of appetite, bad dreams, feelings of uselessness, tachycardia, headaches, muscle pain, sweating, shivering, gastrointestinal disorders, and stress. Therefore, considering the pertinence of moral distress among nursing experts, in their own life in addition in their association with work, the present research tended to the accompanying inquiry: "what implications does moral distress have on nurses?"; with the objective to identify, in national and global scientific literature over the last ten years, the implication that moral distress has on nurses, the similarities between moral distress and burnout, & the adapting techniques for moral distress. [32] Regarding the relationship between nurses' characteristics and studied variables, firstly, the current study revealed that the higher level of moral distress attitude, as well as work stress, were observed among the technical institute of nursing graduates. While the highest level of frequency of exposure to moral distress and clinical practice were observed among the graduates of technical secondary schools of nursing. Significant relationship found between nurses' work stress and their level of education. These results were not surprising as the majority of nurses in Egypt are high school level nurses reflecting an inadequate/insufficient quality of nursing education not only by internationally but even by the region’s local standard. Additionally, health status was at its highest level among the graduates of the faculty of nursing. These results were in similarity with Su et al., 2016 [7] documented significant occupation-related stress amongst staff nurses, especially those working at the base of the hierarchy, those who wind up sharing a large portion of the work load, such as nursing sisters, bedside nurses and staff nurses. Moreover, the results of research conducted by Hassan, et al, 2016 illustrated that, the severity of stress symptoms is more prevalent among secondary technical education (78.0%) compared to university one (11.0%). They found statistically significant associations between educational level and severity level of stress symptoms, p= (0.055 and 0.002). [33] Secondly, the results of our study showed that, overall, the moral distress scores for both sex were relatively high, moreover, both groups (males & females) had an equal moral distress attitude. Female nurses scored higher level of clinical practice than male ones while male nurses recorded higher level of frequency of exposure to moral distress and work Stress. This results not consistent with the study of O'Connell, 2015 who found that women in his study recorded significantly higher moral distress scores than did men. Moreover, this statistical difference was significant. [34] Moreover, Woods et al, 2010 [35] stated as cited in Hassan, 2016 [36] that, evidence of high vulnerability to stress is more widely available, at least for certain subgroups of women. The results revealed a statistically significant gender difference in the mean health status scores of participants, p ≤ 0.05. This result may be attributed to the fact that males newly participate in nursing jobs and unacceptable from the community and physicians in Upper Egypt; as some patients and doctors refuse nursing service provided by male nurses, that’s why they may have feeling of percussion as the exposing to discrimination between them and female ones which higher their work stress. Thirdly, the results of the present study revealed the presence of correlation between, place of work as well as years of experiences and moral studded variables. The highest observed level of distress attitude observed among nurses 6-10 years of experience. Although lower extremity in the years of experience (1-5) in nurses was a higher group frequently exposed to moral distress (57.10 ± 11.08), they were lesser one had work stress tension (35.34 ± 13.55). The more years of experience increased responsibility and thus increase the pressure of work and work stress. The higher level of health status (63.25 ± 7.40) was observed with the higher extremity (>26 years) experience in nursing with significant relationship between nurses' health status and their years of experiences, p ≤ 0.05. Moreover, the higher level of frequency of exposure to moral distress (55.43 ± 13.44) among nurses was observed at university hospital, while the higher level of work stress (45.43 ±16.41) was observed at health insurance hospital. This is may be related to the high rate of following of patients and overload of the work. This is in accordance with Gupta, 2017 who stated that nurses who affiliated to hospitals in large cities may show more strain, morale and quality of work life than others. Additionally, it has been seen that nurses who work in general governmental hospitals are more stressed than their counterparts working in private hospital. [8]Most recently, Krista, 2016 highlighted on ethical climate, ethnicity, a number of beds in the unit, access to a palliative care team, what's more, multiple regression analysis clarified that 37.7% of distress influenced by educational degree. [14] Palliative care teams varied in how present they were in the unit, with social workers reported as the most frequently identified team members, and other disciplines (physician, nurse practitioner, clinical nurse specialist, spiritual care practitioner) were reported present by less than 50% of the participants. Most noteworthy neglected palliative care needs included: psychological & emotional support for patient, family support, and objectives of care conversations. In this regard, Borhani et al, 2014 prescribed the relationship between leaving the job & different factors as monetary status of personnel and people’s desire to enter the nursing profession be investigated. [10]
5. Limitation of the Study
- 1. Lack of references, few studies were done regarding nurses' moraldistress.2. Nurses' work overload results in long waiting time to collect data as nurses were having no or little time to sit and complete the questionnaire. 3. Difficult communication and lack of cooperation with some nurses. Only 66.1% accepted to join in the study.
6. Conclusions
- Finally, from the foregoing discussion, it could be concluded that there are negative relationships between nurses' attitude of moral distress, source of work stress & health status, there are significant relation were found between nurse’s work stress and their level of education and between sex of nurse and health status, finally, between nurses' health status and their years of experience. Also, the most common work stressors are nurses perceived that there is no need for them in the work, no feedback for their work competency and difficulty of unit rules and policies are always the sources of work stress, frequent follow-up, and evaluation, no chance to take action/decision making are often work stress for them.
7. Recommendations
- 1. Further research studies ought to be designed on the effect of preventive measures for moral distress on clinical nursing practice and nurses' health status in non-critical areas and large sample size to generalize the result of study to improve their preventive attitude regarding moral distress, work stressors in numerous geographical zones to explore the perplexing components that hinder nurse's optimal general health. 2. As the results of this study are not generalizable, we propose the requirement for proceeding with research on moral troubles in underrepresented groups in nursing, including cultural and ethnic groups.3. Encourage mass media program to help nurses in the preventive measures of health complaint as insomnia, anorexia.4. The hospital polices should conduct programs for critical care nurses on conflicts, ethical dilemmas and how to solve it.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML