-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2015; 4(2): 19-27
doi:10.5923/j.cp.20150402.01

A Comparison of Lower Quadrant Electromyographic Activity in a Sit to Stand, Squat, and Vertical Jumping Task with and without Therapeutic Taping
Paolo Sanzo, Carlos Zerpa
School of Kinesiology, Lakehead University, Thunder Bay, Canada
Correspondence to: Paolo Sanzo, School of Kinesiology, Lakehead University, Thunder Bay, Canada.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective:The purpose of this investigation was to examine the effects of therapeutic taping (no tape, placebo, Kinesiotape, Leukotape) on lower extremity electromyographic (EMG) activity during three functional tasks (sit to stand, squat, vertical jump). Design: One group, repeated measures design. Subjects: Ten normal and healthy university students (4 females, 6 males; mean age 24 years ± 7.1; height 170 cm ± 10.8; and body mass 69 kg ± 14.4). Methods: Subjects completed four testing sessions with different tape (no tape, placebo, a mechanical correction type of technique with Kinesiotape and Leukotape). Three trials of a sit to stand, squat, and vertical jumping task were completed. Four Delsys dipole EMG instruments with two input channels each were used to measure mean surface EMG activity for the erectorspinae, gluteus medius, vastus lateralis, vastus medialis obliques, semitendinosus, lateral gastrocnemius, tibialis anterior, and peroneus longus muscles. The data were analysed using descriptive statistics and repeated measures ANOVAs. The rejection criteria were set at an alpha level p < .05. Results:Subjects' EMG muscle activity demonstrated a significant interaction effect between the type of tape and muscle type (F(21, 2848)=2.728, p=.0005, η2=.02) with significant differences in muscle type EMG activity for placebo and Leukotape. A statistically significant interaction effect was also evident between the functional task and muscle type (F(14, 2856)=2.956, p=.0005, η2=.014). The highest activation levels were evident for the vastus medialis obliques and tibialis anterior muscles for all functional tasks. A statistically significant interaction effect was also found between the type of tape and functional task (F(6,2868)=2.108, p=.049, η2 =.004) with a higher effect on muscle type EMG activity levels when using placebo tape during the vertical jumping task. Conclusions:Different patellar taping techniques do not produce consistent clinical effects via an alteration in muscle EMG activity. Placebo taping had the greatest effect on EMG activity for most muscles; the vastus medialis obliques and tibialis anterior had the greatest increase in EMG activity with the application of all types of tape. Other taping techniques have been described to inhibit or facilitate lower quadrant muscle activity and, as a result, future research in a symptomatic population comparing facilitatory to inhibitory taping techniques may produce further information on the exact clinical effects on EMG activity as compared to a mechanical correction technique.
Keywords: Placebo tape, no tape, Kinesiotape, Leukotape, Electromyographic activity, Function
Cite this paper: Paolo Sanzo, Carlos Zerpa, A Comparison of Lower Quadrant Electromyographic Activity in a Sit to Stand, Squat, and Vertical Jumping Task with and without Therapeutic Taping, Clinical Practice, Vol. 4 No. 2, 2015, pp. 19-27. doi: 10.5923/j.cp.20150402.01.
Article Outline
1. Introduction
- The incidence rate of knee pain ranges from 3-40% [14, 25] and the prevalence of knee pain has increased over the past 20 years with 25% of adults experiencing pain at some point in his/her lifetime [8, 23]. One of the most common causes of knee pain is patella-femoral pain syndrome (PFPS) [22]. Even minor knee injuries and disorders such as PFPS, may progress, leading to limited functional capabilities and disturbances in work and sport participation, future surgery, and other comorbidities affecting overall health [8, 23]. When dysfunction and pain is present and persists, individuals often change the way in which tasks are completed in an attempt to alleviate some of the pain. These subtle changes often allow individuals to be able to complete his/her required daily functional tasks despite the pain. These compensatory movement strategies also lead to protective patterns [7] and are often accompanied by changes in the central nervous system and higher centres resulting in possible changes in motor control and activation patterns in muscle [4].The presence of knee pain is also often accompanied by range of motion (ROM) and strength changes, instability, locking, and swelling. This further contributes to changes in movement patterning and leads to muscle inhibition and delays in the onset/offset of activation [10, 27]. The resulting muscular weakness and timing delays may lead to further instability and an increased incidence of falls in the older population [9].Although the etiology and pathogenesis is not well understood, it has been theorized that PFPS may be the result of patellar misalignment, abnormal lateral tracking or imbalances between the articular, ligamentous, and muscular structures and neural system [11, 13].The treatment for knee pain, swelling, and weakness, and the resultant dysfunction associated with PFPS may include a variety of conservative measures such as strength and balance exercises, electrotherapeutic modalities, and taping techniques, as well as topical, oral, and injectable pharmacological medications and surgery [3, 6].Therapeutic taping is commonly used to treat patients with PFPS despite the lack of clinical efficacy and the unclear mechanisms of effect. The number of high quality studies available examining the effects of therapeutic taping is limited and clinicians often base treatment decisions on the subjective responses of the individual and previous experience and outcomes generated when used with other patients. When examining the limited studies available looking at the effects of therapeutic taping on electromyographic (EMG) muscle activation levels, the findings reported vary and can be contradictory.It has been proposed that the application of therapeutic taping may affect the alignment of the patellar articular and ligamentous structures and alter proprioceptive feedback [12]. The method by which certain taping techniques are applied has been proposed to realign the patella within the trochlear fossa thereby reducing pain, improving quadriceps and patellar function, and tracking of the patella. This may, in turn, modify the magnitude (increase or decrease) the activation level and/or timing of vastus medialis obliques (VMO) relative to the vastus lateralis (VL) muscle [13]. Cowan et al. proposed that the tape increasedthe amplitude or timing in the VMO and decreased the amplitude and timing of the VL [11, 12].When examining the use of therapeutic taping in other anatomical regions, contradictory findings have also been found. Huang et al. [17] examined the effect of elastic taping on the calf muscles during a maximal vertical jump. Thirty-one healthy adults were tested with the application of Kinesiotape (KT) and placebo tape and vertical jump height, vertical ground reaction force, and EMG activity was measured. Increased EMG activity was found in the medial gastrocnemius muscle with the application of KT but placebo tape did not affect EMG activity.Similar changes were reported with the use of therapeutic taping in the ankle by Ji-Yeon et al. [18]. The EMG activities of the plantar-flexor and dorsi-flexor muscles during inclined walking using tape was examined in 15 women with limited ankle dorsiflexion. The EMG activity in the medial gastrocnemius and tibialis anterior was measured using surface EMG and it was reported that the mean EMG activity of medial gastrocnemius increased while tibialis anterior activity decreased between heel strike and toe off. There is, however, not a clear cut consensus on the effects of therapeutic taping on muscular activity. In fact some studies have reported that the application of tape may produce a reduction in EMG muscle activity [21] or no change or effect.Jun et al. [19] compared different therapeutic taping techniques (KT, McConnell tape, sham tape) on the neuromuscular characteristics (spinal reflex excitability of the VMO and VL; normalized EMG of VMO, VL, medial gastrocnemius, and biceps femoris; VMO/VL ratio; joint kinematics; and pain) during functional task performances in 13 individuals with PFPS. They reported a significant reduction in pain under all conditions during the single leg squat and stair climbing tasks but no significant changes in EMG [19]. Similar results have been reported by Alano de Almeida Linsa et al. [1] and Boucher et al. with no significant effect reported with the application of tape on the EMG activity of the VL [5].In a systematic review completed by Barton et al. [2], it was reported that there is a growing body of evidence to support the association of gluteal muscle strength deficits in patients with knee pain secondary to PFPS. Therefore, the findings may be dependent on the muscle that is chosen to be examined.Altered neuromuscular activity in the hip joint has also been reported by Bolga et al. [4] to be a contributing factor of knee pain secondary to PFPS. Therefore, it is important to consider muscles proximal and distal to the location of the therapeutic tape application and the affected joint.The clinical benefit and therapeutic effect of tape is unclear and contradictory. As a result, the purpose of this investigation was toexamine the effects of therapeutic taping (no tape, placebo, Leukotape (LT), KT) on lower extremity muscle type EMG activity during three functional tasks (sit to stand, squat, vertical jump). The guiding questions for the purpose of the study were: 1) Is there a significant interaction effect between the type of tape and muscle type EMG activity? 2) Is there a significant interaction effect between the type of tape and functional task on muscle EMG activity? 3) Is there a significant interaction effect between functional task and muscle type EMG activity?
2. Methods
2.1. Subjects
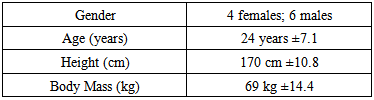
- Ten normal, healthy participants (see Table 1) were recruited via convenience sampling characterized by the selection of easy to obtain members of the population. Healthy participants were defined as individuals without any current or previous history of knee pain, surgery, or dysfunction; nor any other medical conditions or diseases that would preclude participation. Participants who had knee pain; any previous traumatic, inflammatory, or infectious pathology in the lower extremity; fracture, dislocation, or subluxation of the patella; surgery to the knee; signs or symptoms of osteoarthritis; or allergies to adhesive taping were excluded from the study.
|
2.2. Instrumentation
- Four Delsys dipole EMG instruments with two input channels each were used. The Delsys EMG instruments were interfaced with an AD instrument Technologies Power Lab unit and software to read the raw EMG signal for each muscle. There were a total of four amplifiers, eight electrodes, and four grounds used for each participant. The amplifiers were attached to a stand behind the participant so as not to impact on the functional performance of each task. Adhesive bipolar surface EMG electrode sensors were connected to each muscle group and the signal was fed into the Delsys EMG amplifiers that were linked to the AD instrument Power Lab Unit. Mean surface EMG activity for the erector spinae, gluteus medius, VL, VMO, semintendinosis, lateral gastrocnemius, tibialis anterior, and peroneus longus muscles was measured in the participant’s dominant leg.
2.3. Procedure
- Ethical approval for completion of the study was received from the university research ethics board. All procedures and risks were then explained to the participants, and informed written consent was obtained. All of the testing procedures took place at the university multipurpose laboratory. Participants completed a Waterloo Footedness Questionnaire [15, 16]. This questionnaire was completed in order to determine foot dominance as only the participant’s dominant leg was used for testing purposes. The order of the taping interventions (no tape, placebo, KT, LT) and functional tasks performed (sit to stand, squat, vertical jumping) was randomized. During the initial test session, age, and anthropometric measures (height in centimeters and body mass in kilograms) were also taken.Participants completed four separate testing sessions using a different type of tape for each session. Testing sessions were scheduled approximately 24 to 48 hours apart but was also dependent on the participant’s availability. The colour of the tape was standardized for each type and brand. This approach was implemented for the purpose of blinding the participant to the intervention received based on the colours of the tape and to minimize any bias that the tape colour may have introduced. For the placebo taping technique, beige coloured zinc oxide sports tape was used. The tape was the same colour as the LT and KT. The tape was applied to the anterior aspect of the patella without the application of any tension and/or compressive forces (Figure 1A). For the LT procedure, a mechanical correction technique was used. One end of the beige coloured LT was secured to the lateral patellar border. A medial glide was applied to the patella while maintaining tension in the tape. The LT was then firmly anchored to the medial aspect of the knee and soft tissue insuring that the medial tissue was lifted and folds were present in the tape. This allowed for expansion and lengthening of the LT (Figure 1B). A second piece of LT was anchored to the middle of the patella. A medial tilt was applied to the patella and the tape attached to the medial aspect of the knee, as previously described for the first piece of LT [24].For the KT technique, a patellar correction procedure was used with two pieces of beige coloured KT. The length of the first piece of KT extended diagonally from the medial femoral condyle over to the lateral margin of the patella. The KT was cut in the middle for approximately two thirds of the length of the tape forming two tail pieces. The four edges of the KT margins were also trimmed so that rounded edges were present. For the first piece of tape, the KT was anchored to the medial portion of the VMO muscle so that the tape tails were facing diagonally in an inferior and lateral direction. The subject was then instructed to flex his/her knee and the two tail pieces of the KT were tensioned with the upper KT tail piece being applied first to the lateral margin of the patella. This was followed by the subject then extending the knee back to neutral and the second lower KT tail piece being applied over the patella slightly offset from the first piece of KT [20, 24]. For the second piece of KT, the same length of tape and preparation procedures were used. With the subject’s knee in a fully extended position, the KT was anchored to the anterior and medial aspect of the knee with the KT tails facing superiorly and laterally. The subject flexed his/her knee as the upper KT tail was firmly anchored to the lateral margin of the patella with maximum tension. With the knee still in a flexed position, the lower KT tail was also anchored to the lateral margin of the patella without any tension applied [20, 24] (Figure 1C).
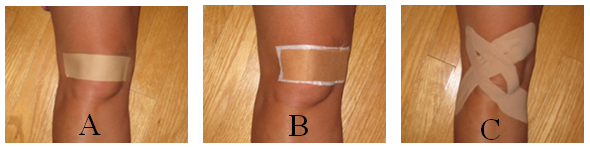 | Figure 1. Placebo taping (A), LT (B), and KT techniques (C) |
2.4. Signal Processing and Filtering
- A power spectrum analysis was conducted to determine the cutoff frequency of the signals. The cutoff frequency of the EMG signals ranged from 6 to 8 Hz. After each signal cutoff frequency was determined, the raw EMG signal was rectified using a mathematics absolute value function. A 10 Hz low pass filter was applied to the rectified signal to eliminate any high frequency noise that could potentially interfere with the EMG readings. The average EMG from each rectified signal was computed.
2.5. Data Analysis
- Descriptive statistics were used to compare the mean and standard deviations for EMG with and without tape for each muscle. Three independent variables (muscle type, functional task, and taping condition) and one dependent variable (mean EMG) were examined. Two-way repeated measures ANOVAs were used to detect significant interaction effects between the independent variables, muscle type (the erector spinae, gluteus medius, VL, VMO, semintendinosis, lateral gastrocnemius, tibialis anterior, and peroneus longus muscles) under four taping conditions (no tape, placebo, KT, LT) while completing a functional task (sit to stand, full squat, and maximum vertical jumping task). A Bonferroni correction was implemented to keep the error rates at an alpha level of .05.
3. Results
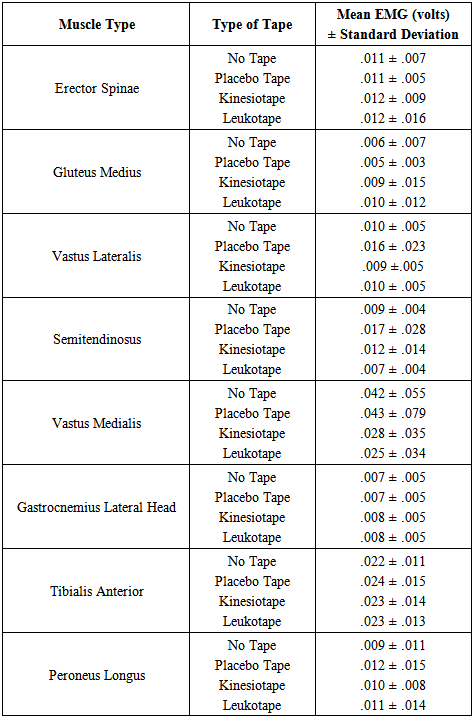
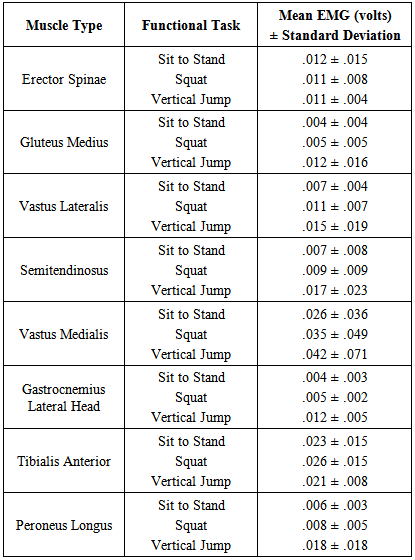
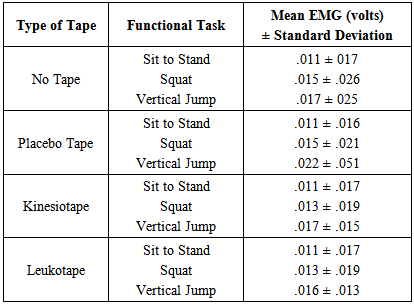
- Subjects' EMG measures demonstrated a significant interaction between the type of tape and muscle type (F(21, 2848)=2.728, p=.0005, η2=.02). Bonferroni mean comparisons revealed significant differences in muscle type EMG activity for placebo and LT. As depicted in Figure 2, muscle type EMG activity seems to converge across all tape conditions, however, a significant low effect on muscle activation was evident when using placebo and LT. Descriptive statistics for the EMG activity (volts) for muscle type by type of tape is highlighted in Table 1.
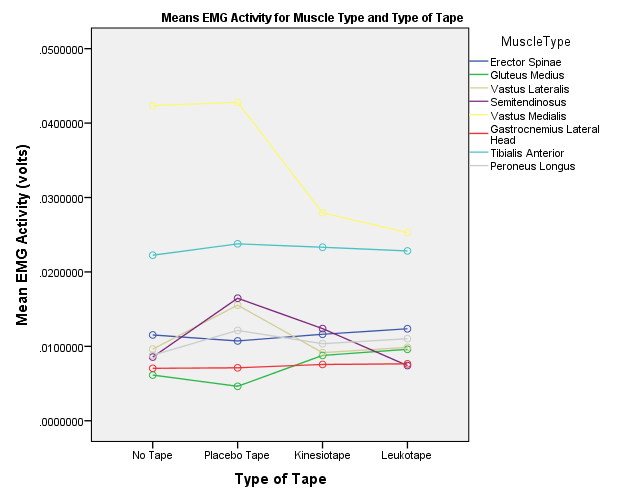 | Figure 2. Mean EMG activity (volts) for the muscle type and type of tape |
|
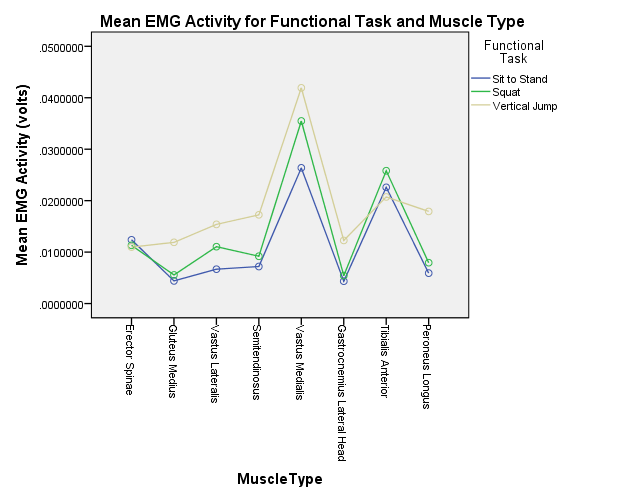 | Figure 3. Mean EMG activity (volts) for the functional task and muscle type |
|
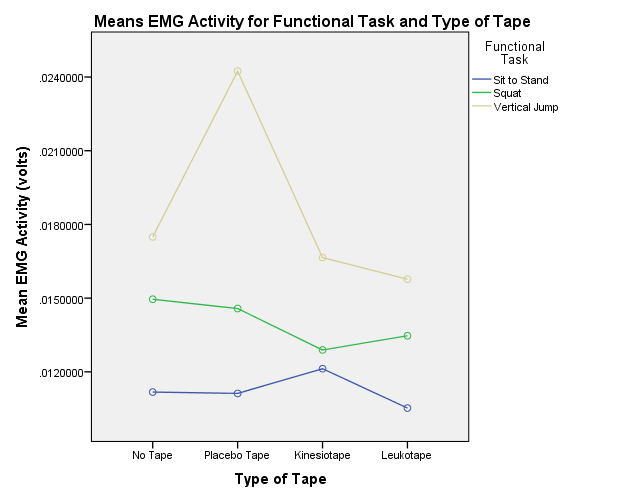 | Figure 4. Mean EMGactivity (volts) for the functional task and type of tape |
|
4. Discussion
- The purpose of this investigation was to examine the effects of therapeutic taping (no tape, placebo, KT, LT) on lower extremity EMG activity during three functional tasks (sit to stand, squat, vertical jump). The current findings, however, suggest that different patellar taping techniques do not produce consistent clinical effects via an alteration in muscle EMG activity. Placebo taping had the greatest effect on EMG activity for most muscles; the VMO and tibialis anterior had the greatest increase in EMG activity with the application of all types of tape. The number of studies examining the effects of therapeutic taping on EMG activity is limited and the overall conclusions remain contradictory. These varied responses and reports are consistent with the findings of the current study. The varied responses may be due to several factors including the different outcome measures used and the presentation of the results and findings [13]. Different types of tape and methods of application, the type of functional tasks performed (weight bearing versus non weight bearing) [4], different muscles being tested, and the method in which the muscle activity was recorded makes comparison of the studies difficult.In the current study, a mechanical correction technique was used for the KT and LT compared to placebo or no tape as clinically this is one of the most common techniques applied. The theory behind a mechanical correction technique is that the abnormal patellar position will be realigned thereby reducing pain that is present; this, however, may not necessarily mean that the recorded muscular EMG activity will be affected. The proposed off-loading of pressure with the mechanical correction technique may be beneficial in reducing subjective pain as the excessive compression to the articular surfaces of the patella may be part of the contributing factor to pain development [11, 13]. The participants of the current study included a normal healthy population without any knee pain or dysfunction; as a result, the lack of knee pain may have contributed to some of the inconsistent changes seen in EMG muscular activity with the application of tape. With some functional tasks, certain tapes had a greater effect than in other tasks. These different tapes then did not produce the same effects on the other tasks having very little effect. It is possible that the effect of the tape may be task dependant.The proposed patellar realignment with the application of therapeutic tape may be very small and not detectable with the current measurement and observational techniques used for research purposes. These small changes may be enough to alter intra-articular and inter-osseous pressure and this may be clinically significant; treatments producing even minute changes in compression may not be visible or statistically significant but may have clinical relevancy in justifying the use of tape [13].It has been reported that a coordinated contraction between the VMO and VL is required in order to maintain optimal patellar alignment [13]. In a normal and healthy population, the activation levels and timing of muscular contraction may already be balanced and unaffected. Tape applied to these individuals may not produce meaningful change or consistent EMG findings since there were no significant deficits to begin with [13]. The current findings support this notion as the effects were quite varied with the LT or placebo taping producing opposite effects at times and then reversing and being at the other extreme with different functional tasks. The responses to taping may, therefore, be dependent upon the functional task or sport specific maneuver that is performed by the individual and possibly the vigour and speed of the movement (i.e., sit to stand versus maximum vertical jumping task).The current literature available continues to provide contradictory findings with some reports of decreased or increased activation levels of various muscles; presently it appears that tape does not change the EMG activity consistently in the VMO and VL. As a result, it is important to examine a wider array of muscles in the lower quadrant as has been done in the current study. Bolga et al. reported the importance of considering the effect that gluteus medius had in patients with PFPS [4]. If it is clinically important to increase the activation or strength in the gluteus medius muscle, the current findings, in which the application of KT and LT resulted in the greatest increases in gluteus medius activity, further justify the use of tape as an adjunct to some of the proposed exercise programs. As more emphasis in rehabilitation programs for patients with knee pain secondary to PFPS, overuse tendinopathies, osteoarthritic degenerative changes, or following arthroscopic surgery is placed on quadriceps and gluteus medius strengthening, the use of tape may assist with the early activation of these muscles to help the patient return to normal functioning and strength earlier [1, 2].Optimal alignment has also been reported to be important from the perspective of realigning the patella within the trochlear fossa not only to reduce pain but also improve quadriceps and patellar function and tracking of the patella in relation to exercise. This has been reported to be very important in order to provide effective retraining strategies for the lower quadrant musculature during rehabilitation [13].The findings of the current study have also demonstrated that the application of therapeutic taping had the greatest effect on the VMO and tibialis anterior muscles. This may also be beneficial during rehabilitation programs attempting to facilitate these muscles following injury as the pain or swelling present in the knee commonly results in a protective inhibition in the quadriceps [21, 26]. It has been proposed that quadriceps retraining should be performed in a pain free range [13]; because previous studies have reported that the application of tape is effective at achieving this, the present findings further justify the use of tape to increase activity in the VMO. Furthermore, it is important to consider the use of taping during retraining and in rehabilitation programs since the VMO and tibialis anterior muscles play key roles in the dynamic stability and eccentric control of the knee and ankle region especially during tasks that require loading or during the contact phase of walking and running.A limitation to this study was the small sample size used. Due to the time constraints on the individuals and the number of testing sessions that participants had to voluntarily attend, a small sample was used for the current study. Future studies should incorporate a larger sample size as this may elucidate some of the significant interactions that may be present. Another limitation was due to the use of surface EMG and the multiple cords that were attached to the participant, as this may have altered the method by which each functional task was performed. Since the EMG activity was recorded in multiple muscles simultaneously, cross talk may have also provided some alteration in the EMG signals. The EMG signals were measured immediately following the completion of the functional tasks and it has also been proposed that in some cases the muscle activity may actually increase 24-48 hours after the application of tape, so this is another consideration that may have contributed to the current findings [28].Future investigations should incorporate the use of wireless or fine wire EMG to eliminate the effect of the numerous cords on the performance of the tasks. Also, the study should incorporate a pathological group compared to normal healthy controls. A similar evaluation can then be applied or the use of other functional tasks such as walking, running, or stair climbing included. Future studies also need to examine multi modal treatment as some of the current study designs have examined the effects of tape in isolation but clinically rehabilitation programs are not designed in this manner. The interaction of tape with other interventions must be considered and evaluated in the design of future studies. If the study design does not represent the current clinical practice or standard of care, then it is difficult to draw a conclusion that is meaningful and clinically relevant.
5. Conclusions
- Different patellar taping techniques do not produce consistent clinical effects via an alteration in muscle EMG activity. The effect of the tape may be dependent upon the specific muscle type or the type of sport or functional task being performed. In the present study, the application of placebo tape had the greatest effect on EMG activity; the VMO and tibialis anterior had the greatest increase in EMG activity with the application of all types of tape. Due to the variable effects found, healthcare providers may choose specific types of tape based on availability in his/her clinical setting, cost of the different types of tape, and patient preference but also being mindful of the specific task that the patient/athlete is required to complete.Therapeutic taping continues to be a widely used treatment option with a variety of theoretical concepts justifying its use. The efficacy and exact effects continue to not be well understood and further studies are required to elucidate on the concepts.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML