-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2015; 4(1): 12-17
doi:10.5923/j.cp.20150401.03
Analysis of Extracted and Retreated Root Canal Treatment Failures in a Nigerian University Teaching Hospital
Bamise C. T.1, Dada B.2, Gureje G. A.2
1Department of Restorative Dentistry, Faculty of Dentistry, Obafemi Awolowo, University, Ile-Ife, Nigeria
2Department of Restorative Dentistry, Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife, Nigeria
Correspondence to: Bamise C. T., Department of Restorative Dentistry, Faculty of Dentistry, Obafemi Awolowo, University, Ile-Ife, Nigeria.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
The study evaluated the reasons for extraction and retreatment of failed endodontically treated teeth diagnosed within a period of three years in a University Teaching Hospital. Seventy one patients who attended the out-patient clinic with a diagnosis of endodontic failure and subsequent referral for extraction or retreatment. Information regarding the failed teeth was collected on a data form. Seventy one failures were analyzed. 45.7% from females and 54.9% males. Age range of 20 to 29 years had the highest number of failures. 50.7% were mandibular teeth while 49.3% accounted for the maxillary teeth. 91.5% were molars/bicuspids and 8.5% anteriors. 66.2% of the teeth were restored with amalgam and Jacket crowns had 2%. 47.7% failed within 6 months and 25.4% failed after 2 years. 57.7% had multiple visits while 42.3% had single visit. 74.6% of the failed therapies were performed by Resident doctors. Endodontic failures were 36.6% and 63.4% non endodontic. 57.7% of endodontic failures were maxillary teeth (57.7%) and 55.6% of non endodontic failures were mandibular teeth.73.1% of the endodontic failures occur in multiple visits while 51.1% of non endodontic failures occur in single visit. Radiographically, 50% of the endodontic failures were poorly filled. Failures were mainly molars restored with amalgam and substantially failed within 6 months. Most posterior endodontically treated teeth should be restored with crowns. Complex cases should be referred to specialists to reduce incidence of endodontic failures.
Keywords: Endodontically-Treated Teeth, Retreatment, Tooth Extraction
Cite this paper: Bamise C. T., Dada B., Gureje G. A., Analysis of Extracted and Retreated Root Canal Treatment Failures in a Nigerian University Teaching Hospital, Clinical Practice, Vol. 4 No. 1, 2015, pp. 12-17. doi: 10.5923/j.cp.20150401.03.
Article Outline
1. Introduction
- The key to successful endodontic treatment is to thoroughly debride the canal system of infected or necrotic pulp tissue and microorganisms, and to completely seal the canal space, thus preventing the persistence of infection and/or reinfection of the pulp cavity [1]. Root canal treatment usually fails when the initial procedure falls short of minimum acceptable technical standards [2]. Undoubtedly, the major factors associated with endodontic failure are the persistence of microbial infection in the root canal system and/or the periradicular area [3]. Siqueira (2010) [4] further stated that the reason many teeth do not respond to root canal treatment is because of procedural errors that prevent the control and prevention of intracanal endodontic infection. Often the clinician is misled by the notion that procedural errors, such as broken instruments, perforations, overfilling, underfilling, ledges and so on are the direct cause of endodontic failure [4]. In most cases, procedural errors do not jeopardize the outcome of endodontic treatment unless a concomitant infection is present. In truth, a procedural accident often impedes or makes it impossible to accomplish appropriate intracanal procedures. Thus, there is potential for failure of root canal treatment when a procedural accident occurs during the treatment of infected teeth [3].Nevertheless, there are some cases in which the treatment has followed the highest technical standards and yet failure results [3]. Scientific evidence indicates that some factors may be associated with the unsatisfactory outcome of well-treated cases. They include microbial factors, comprising extraradicular and/or intraradicular infections, and intrinsic or extrinsic nonmicrobial factors [3, 5]. Analysis of the reason for all extractions of endodontically treated teeth carried out by Vire (1991) [6] has revealed three types of failures; unrestorable tooth fractures, involvement in periodontal problems and endodontic failures.Endodontic failures were less frequent and are commonly caused by bacterial recontamination of the root canal from the oral cavity [7], due to loss of temporary restorations or leakage of an inadequate final restoration. Failure of a root-filled tooth can be due to less than optimal endodontic therapy but inadequate or unsuccessful restorative treatment has been described as the major issue. Among Endodontic specialists, the chances of achieving a successful result in initial non-surgical endodontic treatment are generally considered good with estimates as high as 97% [8], however, on a general note outcomes vary based on the clinician's skill and experience [9]. In order to improve the success rate, it has been emphasized that undergraduate and continuing education in endodontics should be given more emphasis, and that the referral of difficult cases to dentists with advanced knowledge and training in endodontics should be made possible for the benefits of patients [10, 11, 12]. It is the aim of the study to evaluate the reasons for extraction and retreatment of failed endodontically treated teeth for a period of three years in the Dental Unit, Obafemi Awolowo University Teaching Hospitals Complex Ile Ife Osun State Nigeria.
2. Competing Interests
- Authors declared that no competing interest exist
3. Methodology
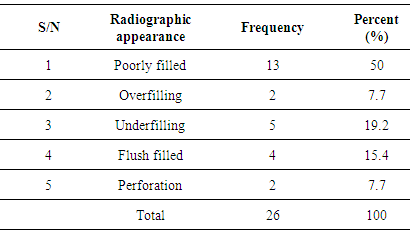
- Teeth included in the study were from seventy one patients who reported in the clinic and were diagnosed of endodontic failure with subsequent referred for extraction or retreatment. Analysis of the reasons for all the retreatment and extractions of all the failures over a period of 4 years were done in the Restorative clinic, Dental unit of Obafemi Awolowo University Teaching Hospitals Complex Ile-Ife Nigeria.The sample size was not predetermined, however cases of endodontic treatment failure recorded during predetermined period of three years was the sample size. Information regarding the failed cases was collected on a data form. All root-filled teeth presented with coronal fracture, tenderness to pressure, pain, swelling, and active sinus tract were declared as an endodontic failure cases. The teeth and the surrounding tissues were examined and the quality of coronal restoration was also observed. A well developed radiograph was taken for each case and was thoroughly read under illumination of X-ray viewer in our clinic by at least two of the authors, to determine the cause of failure by observing the status of root canal filling or any other abnormality in the root canal system. The root filling more than 2 mm short of the radiographic apex were considered under filled while filling that ends beyond the radiographic apex were considered overfilled. Any voids or radiolucent space running along the entire or some of the working length of root filling were considered poorly filled. Perforation and separated instrument were also looked for [13]. The subjects were then scheduled for re-root canal treatment, endodontic surgery or extraction as the case may be. For the purpose of analysis the failed cases were classified as endodontic failures and non endodontic.
4. Results
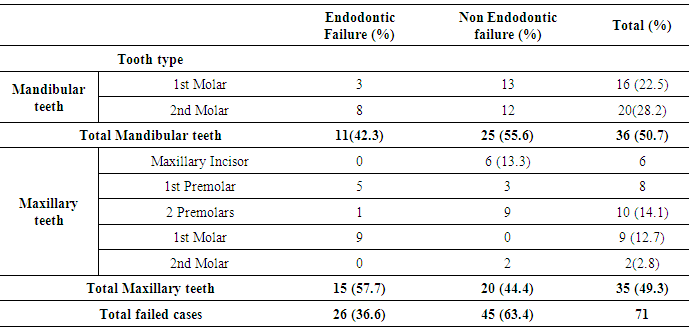
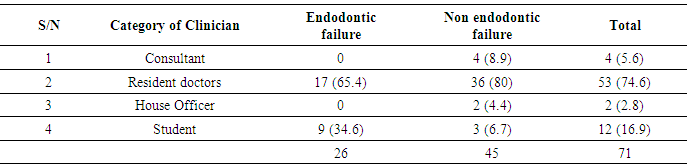
- Seventy one failed endodontically treated teeth indicated for extraction or endodontic retreatment were analyzed. 45.7% were from females while 54.9% were males. This results shows that age range of 20 to 29 years had the highest number of failed cases (43.6%). 40 to 49 years of age shows the least number of failure. Table 1 shows that 50.7% of the failures were mandibular teeth while 49.3% accounted for the maxillary teeth. 91.5% were molars and bicuspids and 8.5% anteriors. Percentage contribution of the tooth types in descending order: mandibular second molar had 28.2%; mandibular first molar 22.5%; maxillary 2nd premolar 14.1%; maxillary first molar 12.7% and maxillary 2nd molar. There were no mandibular anteriors and premolars.
|
|
|
|
|
|
5. Discussion
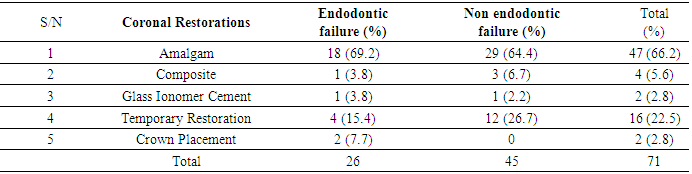
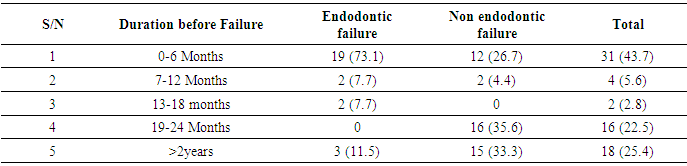
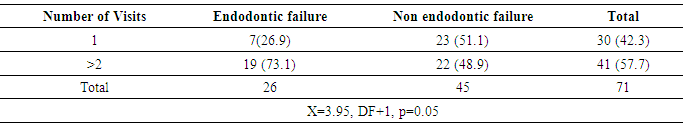
- Root canal treatment fails when the treatment is carried out inadequately. However, there are some cases in which the treatment has followed the highest standards yet still results in failure. Undoubtedly, several major and minor factors had at various times been associated with endodontic failure [3].The failed endodontically treated teeth in this study were slightly more in males than females. This observation may not have accurately reported the prevalence across gender because the total number of root canal treatment done within the period evaluated was not determined. In this instance, it appears that male patients were more conscientious about returning for their follow–up examinations than females. In a study by Rashid (2008) [14], females had a higher failure rate compared to males. These differences, however, were not statistically significant. The female predominance was also attributed to conscientousness of the female patients about returning for re-examination. Age of the patient is known to affect the outcome of root canal treatment [15]. Predominantly, the failed root canal therapies were seen in younger age groups. This further supports the report of Dummer and McGinn (1984) [16] that the prognosis of root canal therapy is better in older patients because of the tighter apical foramina, lack of completely patent auxiliary canals and dense periapical bone. Older teeth with more restricted canals were more successfully obturated than very young teeth with large-diameter canals. However, difficulties are encountered in (adult) teeth in which canals, through time, continue to narrow down as a result of deposition of mineralized tissue [17], as well as the decrease in healing ability of elderly patients [18].Our findings show that mandibular molars accounted for most failures; this is similar to the comment of McComb (2008) [7] in a review article that the most common endodontic failures are seen in mandibular molars. Although Mandibular first molar has been described as the most frequently root filled tooth and the tooth with the greatest rate of endodontic failure [6], a preponderance involvement of mandibular second molar was observed in this study. This could be explained by the pattern of provision of RCT with respect to the teeth involved which tends to follow the reported order of susceptibility of teeth to caries. Mandibular second molars have been observed to be the most susceptible teeth to caries [19, 20]. This was further confirmed by our finding that the commonest reason for the initial endodontic therapies of the evaluated teeth is caries and its sequelae.Although it is agreed that radiographic technical quality of endodontic therapies influences the outcome, issue such as adequacy of coronal restorations plays significant role in the endodontic failure [21]. Majority of the failed endodontics were restored with amalgam with placement of crowns on less than 10% of them. This is contrary to the view that clinical longevity of endodontically treated posterior teeth especially molars and bicuspids is significantly improved with coronal coverage [22, 23, 24]. A high incidence of failure for posterior endodontically treated teeth without cusp coverage has been reported and evidence strongly supports that placement of a crown to encircle the tooth can increase the resistance of posterior teeth to fracture [22]. Aqualina et al. (2002) [23]. found that endodontically treated teeth without crowns failed at a 6 times greater rate than uncrowned teeth. McComb (2008) [7] in a review of the restoration of the endodontically treated tooth mentioned that it is the current teaching in most dental schools (in Canada) to give serious consideration to the provision of full coverage crowns for endodontically treated posterior teeth, particularly molars. Slightly less than half (43.7%) of the failures occur within 6 months after completion and most of them were endodontic failures. In the evaluation for failure of all endodontically treated teeth that were extracted over a 1 year period, Vire (1991) [6] observed that extraction occurred much quicker in teeth involved in endodontic failure. This author therefore concluded that failure of true endodontic origin is less frequent but appears to occur faster than that of other categories.Our evaluation revealed that the failed teeth associated more with multiple visit especially those of endodontic origin. In a systematic review of the effectiveness of single-versus multiple-visit endodontic treatment of teeth with apical periodontitis, Sathorn et al. (2005) [25] concluded that based on the current best available evidence, single-visit root canal treatment appeared to be slightly more effective than multiple visit, i.e. 6.3% higher healing rate. Those who believed that successful root canal treatment can be accomplished in one visit have rationale in the literature. Studies concerning postoperative pain [26, 27], as well as healing rates, shows the treatment outcomes to be similar, whether completed in one visit or in multiple visits [28]. Those who advocated multiple–visit procedures proposed that the antimicrobial property of inter-appointment calcium hydroxide placement is required to ensure successful periradicular healing [28, 29], Furthermore, when flare–ups occur during multiple–visit procedures, they can be addressed prior to obturation [30]. This is not an option in a single–visit treatment regimen. When flare–ups occur, non–surgical re–treatment or surgical intervention is usually necessary [31].Majority of the failed endodontic procedure were originally performed by Resident doctors [doctors undergoing postgraduate training]. Also, most of the failures occurred in molars (Upper/Lower) and premolars. This observation, coupled with the fact that the evaluated teeth were mostly molars that are complex in nature and associated with numerous anatomical variations of the canal system renders them difficult to be treated successfully by non endodontist and resident doctors. The teeth included in this study were filled by cold lateral condensation technique. This technique in conjunction with a root canal sealer is most widely accepted technique for root canal filling. It is a simple and versatile technique [32]. However, it must be stated that undergraduate students lack extensive endodontic practice and limited exposure to this procedure which may results in inadequate endodontic treatment. Although our undergraduates are under strict supervision when working on posteriors, sizable amount of the failed procedures was performed by students. At a more scientific level, it is apparent that endodontic outcomes depend on the expertise of the treating clinician [33]. In four cases treated by consultants, although the root canal filling was adequate, failure occurred as a result of non endodontic origin.Inadequate or unsuccessful restorative treatment has been described as the major issue in endodontic failure [7] which is evident in this study. More than half of the failures were due to fracture of the natural coronal tooth structure, split tooth and loss or fractured restoration. They were considered failed because the remaining coronal sound tooth tissues were unrestorable. Only two of the evaluated teeth were crowned and had endodontic failure.Although in a different setting, the percentage of endodontic failures found in our study was more that what Vire (1991) [6] found in a busy Military Hospital in USA. A potential cause of endodontic failure is bacterial recontamination of the root canal. In most cases, the failure is as a result of microorganisms persisting in the apical portion of the root canal system, even in well-treated teeth [4]. If microorganisms persist in the root canal at the time of root filling or if they penetrate into the canal after filling, there is a higher risk that the treatment will fail [34, 35]. How high the risk of reinfection will be is dependent on the quality of the root filling and the coronal seal [36].Half of the endodontic failures in this study presented radiographically as poorly filled. The absence of voids within root fillings and between the root fillings and canal walls have been strongly correlated with lower risk of post-treatment disease. Several studies had found that a root filling that is less dense and non-homogenous will have a negative impact on the treatment outcome [37, 38]. In a review by Siqueira (2001) [4], voids and other minor flaws in the obturation, which often are not detected radiographically, may be responsible for the rapid recontamination of the root canal system. This probably explains rapid manifestations of endodontic failures seen in this study.
6. Conclusions
- Mostly the failed teeth were from young male patients. They were mainly molars restored with amalgam and substantially failed within 6 months. This lends credence to the fact that restoration of endodontically treated posterior teeth should be done with complete crowns to reduce the prevalence of non-endodontic failures. This must be instituted as a policy especially in institutions where various categories of dental surgeons are involved. The initial root filling was predominantly performed by resident doctors. This observation to a large extent, in addition to where students are involved in treatment underscores the recommendation that the procedure should be performed under close supervision of consultants. The more complex cases referred to endodontic specialists to reduce incidence of endodontic failures.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML