-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2015; 4(1): 6-11
doi:10.5923/j.cp.20150401.02
The Treatment of Chronic Rotator Cuff Tendinopathy of the Shoulder with Radial Shockwave Therapy
Paolo Sanzo
School of Kinesiology, Lakehead University, Thunder Bay, Canada
Correspondence to: Paolo Sanzo, School of Kinesiology, Lakehead University, Thunder Bay, Canada.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Objective: To assess the effects of radial shockwave therapy (RSWT) on shoulder function, pain, range of motion (ROM), and strength in patients with chronic rotator cuff tendinopathy (RCT). Design: One group pre-test post-test design. Methods: 24 subjects (17 males and 7 females) diagnosed with chronic RCT had their shoulder strength and ROM measured along with functional status via the Upper Extremity Functional Scale (UEFS) and shoulder pain with the P4 Scale and pain at rest, after activity, and overall improvement in pain using a visual analog scale (VAS) pre-treatment. Each subject was then treated with RSWT consisting of 2000 shockwaves set at an intensity of 2.5 bars, 10-15 Hz, and 11.5 Mp. The applicator was positioned so that treatment was completed over the insertion point of the supraspinatous muscle. Each subject received three treatments in total spaced one week apart over a three week period of time. Shoulder strength, ROM, UEFS, P4 and VAS scores for pain and overall improvement were measured again three months post-treatment. A Wilcoxen Signed Rank Test and Dependent t-Test was used to analyze the data comparing pre-treatment to post-treatment effects with an alpha level set at p<.05. Results: A significant improvement was found post-treatment in the UEFS score (Z=-3.895, p=.0001); in the P4 score (Z=-4.078, p=.0001); in the VAS for shoulder pain at rest (Z=-3.062, p=.002); shoulder pain following activity (Z=-4.138, p=.0001); and in the overall improvement in shoulder pain (Z=-4.11, p=.0001). A significant improvement was also noted in the ROM for shoulder flexion (t(23)=-2.075, p<.013); abduction (t(23)=-3.54, p<.002); internal rotation (t(23)=-2.503, p<.02); and external rotation (t(23)=-3.78, p<.001). A significant improvement was also noted in shoulder strength for abduction (Z=-2.585, p=.01) and external rotation (Z=-2.64, p=.008).
Keywords: Radial shockwave therapy, Rotator cuff, Tendinosis, Pain, Function, Range of motion, Strength
Cite this paper: Paolo Sanzo, The Treatment of Chronic Rotator Cuff Tendinopathy of the Shoulder with Radial Shockwave Therapy, Clinical Practice, Vol. 4 No. 1, 2015, pp. 6-11. doi: 10.5923/j.cp.20150401.02.
Article Outline
1. Introduction
- Shoulder pain secondary to rotator cuff tendinopathy (RCT) is the third most common cause of musculoskeletal pain after low back and neck pain [3]. Shoulder impingement resulting in RCT is also a frequently reported secondary diagnosis for patients initially complaining of neck and arm pain related to other disorders [12]. The most commonly affected tendon in RCT is the supraspinatous (80%), followed by the infraspinatous (15%), and subscapularis (5%) tendons [12].The annual incidence of RCT ranges from 7-36% with the average age of onset being 55 years and the peak incidence occurring in middle age between 30 and 50 years [13]. Rotator cuff tendinopathy is also equal among genders and is one of the most prevalent and costly work related musculoskeletal disorders [10, 13]. The incidence of work related shoulder pain is often associated with highly repetitive work tasks using the arms, forceful exertion in completing work tasks, awkward postures, and jobs with high psychosocial demands [12]. Eighteen percent of individuals working in manual labor jobs often develop and report shoulder pain secondary to RCT [3]. The etiology of RCT is multi factorial but reports suggest links to age related degeneration, microtrauma, and macrotrauma [30]. Rotator cuff tendinopathy is often a self-limiting disorder [9, 15] but when it does not improve or when conservative treatment fails, the next steps are a matter of debate. When RCT continues and progresses, the disorder often leads to further functional limitations, chronic pain and weakness, and eventual tearing of the rotator cuff with half of individuals over the age of 80 presenting with a rotator cuff tear [30]. As can be seen, much still needs to be learned about the etiology, pathophysiology, and management of RCT.Many treatments exist for RCT but few are supported by strong scientific evidence with many contradictory findings reported. Treatments for RCT include a variety of interventions such as therapeutic modalities, medications, exercise, and surgery. The evidence for the efficacy of conservative treatment, however, is not well established and remains controversial. One such treatment includes radial shockwave therapy (RSWT) but the utility of this therapeutic option remains controversial, with the mechanism of action and effectiveness remaining unclear. Several clinical trials have been completed examining the effects of shockwave therapy on RCT and calcifying tendinitis with mixed results [20, 23, 28, 32].Albert et al. [1] examined the effects of high versus low energy shockwave therapy on individuals with greater than a 3 month history of calcifying tendinitis of the rotator cuff and with a calcification that measured greater than 10 mm in size. They found that individuals receiving high energy shockwave therapy (.07-.44 mJ/mm2) had an improvement in pain and function as measured on the Constant and Murley score. No signficant change was reported with low energy shockwave therapy (.02-.06 mJ/mm2). There was also no change in the size of the calcium deposit with either treatment.Similar findings using high energy shockwave therapy has also been reported by Farr et al. (2011) with a reduction in pain during weight bearing reported and an improvement in overall function with a single treatment of high dose shockwave therapy (.3 mJ/mm2) [6].Conversely, Gerdesmeyer et al. [9] reported that both high and low energy shockwave therapy were effective in decreasing shoulder pain, improving function, and reducing the size of the calcification in comparison to placebo. High energy shockwave therapy, however, was more superior to the low energy shockwave therapy. Ioppolo et al. [13] reported similar effects when comparing two different ranges of energy flux density in the treatment of supraspinatous calcifying tendinitis with higher energy also being superior to lower energy treatment.Schofer et al. [21] also reported improvement in pain and function with shockwave therapy treatment but reported no significant difference between the high versus low energy treatment groups.Several systematic reviews and meta-analyses have also reported conflicting findings. Moderate positive results have been reported by Bannuru et al. [2], Harniman et al. [10], Huisstede et al. [12], and Speed [26] on the use of focused, high energy shockwave therapy in RCT.Overall, there are a limited number of high quality studies available examining this area and the level of evidence is moderate supporting the use of high energy shockwave therapy to treat calcific RCT in reducing pain and improving function; the level of evidence is low for the use in the treatment non-calcific RCT [5, 8, 14, 16, 17, 31].As a result, the clinical rationale for this study was to support, develop, and update the evidence based protocols and clinical guidelines for the use of RSWT in the treatment of non-calcific RCT in an attempt to optimize the quality of care for patients with shoulder pain and dysfunction secondary to supraspinatous involvement [12]. Therefore, the purpose of this study was to investigate the effects of RSWT on shoulder pain, function, ROM, and strength in patients with chronic RCT.
2. Methods
2.1. Subjects
- Participants included 24 individuals diagnosed with chronic RCT of the supraspinatous muscle. Descriptive data for height, weight, side of involvement, and length of time that the shoulder pain was present is summarized in Table 1.
|
2.2. Apparatus
- A long arm Baseline® Absolute-Axis™ plastic goniometer was used to complete all of the ROM measures. The use of a measurement device with strong evidence of reliability and validity is an important prerequisite for assessment in clinical practice, as well as for the collection and interpretation of research results. This method of ROM measurement has been reported to be an accurate method of determining shoulder joint mobility [19].A Storz D-Actor 100© RSWT unit was used for treatment for all participants.
2.3. Procedure
- Once the purpose and methodology of the study was explained and consent to participate was obtained, anthropometric measures were taken and self report outcome measures completed. Age, height (cm), weight (kg), and length of time that the pain was present (months) was recorded.Functional status was measured via the Upper Extremity Functional Scale (UEFS). The UEFS is a 20-item self report questionnaire that is scored on a 5-point scale (0 to 4). It can be used to assess upper extremity functional status on a variety of conditions and levels of severity [18, 27]. The total calculated UEFS score ranges from 0 to 80 with higher scores indicating greater functional ability. The UEFS has been validated in upper extremity dysfunction, shoulder impingement and post-surgical patients with a test-retest reliability ICC of .85-.95 reported [27].Shoulder pain was measured using a visual analog scale (VAS). The subject was asked to consider the following questions when filling out the linear VAS scale: (1) their level of shoulder pain at rest; (2) their level of shoulder pain following activity; and (3) their overall improvement in shoulder pain. Overall improvement was defined as the change in shoulder pain level from the onset of treatment related to the study with subjects considering the pre-treatment overall improvement score as being zero. Subjects marked the VAS at the point that corresponded to their pain intensity or overall improvement level. The amount of pain or overall improvement level was estimated by measuring in millimeters the distance from the “no pain” marker to the mark provided by the subject for each question. The VAS has been shown to have good validity, reliability, and psychometric properties. The reported test-retest reliability for the VAS ranges from .71-.99 [7, 22] and the pooled value for construct validity ranges from .71-.98 [11, 29].Shoulder pain was also measured with the P4 Scale. The P4 Scale is a four item self report questionnaire scored on an 11-point scale (0 to 10). The total P4 Scale score ranges from 0 to 40 with higher scores indicating greater pain. It has a reported internal consistency of .90-.92 and test-retest reliability of .79-.81 [25]. This alternate measure was also used in order to examine changes in shoulder pain and prevent any ceiling or flooring effects that may occur when using a VAS. The minimal detectable change for the VAS has been reported to be a change in ±2.8 mm [4] so if a participant reported a starting score of less than 2.8 or greater than 7.2, the VAS may not be sensitive enough to pick up pain changes whereas the P4 Scale has a larger score range and may provide an alternate measure without some of the described limitations at the extremes of the VAS.After the self-report measures for pain and function were completed, active ROM and strength of the shoulder were assessed with the participant in standing. Active ROM for the shoulder joint was measured and recorded in degrees using a Baseline Absolute-Axis™ goniometer. Resisted isometric strength of the shoulder was measured, graded, and recorded using the 5-point Oxford scale (grade 5 - movement against gravity with full resistance; grade 4 - movement against gravity with some resistance; grade 3 - movement against gravity only; grade 2 - movement with gravity eliminated; grade 1 - visible and palpable muscle contraction but no movement and; grade 0 - no contraction).After the baseline pre-treatment measures were completed, the subject was treated with RSWT. Each subject received 2000 shockwaves set at an intensity of 2.5 bars, 10-15 Hz, and 11.5 Mp using a Storz D-Actor 100© RSWT unit. The applicator was positioned so that treatment was completed over the insertion point of the supraspinatous muscle. Each subject received three treatments in total spaced one week apart over a three week period of time. Shoulder ROM and strength and the UEFS, P4, and VAS for pain at rest, after activity, and for overall improvement were measured again three months post-treatment. A Wilcoxen Signed-rank Test and Dependent t-Test was used to analyze the data comparing pre-treatment to post-treatment scores.
3. Results
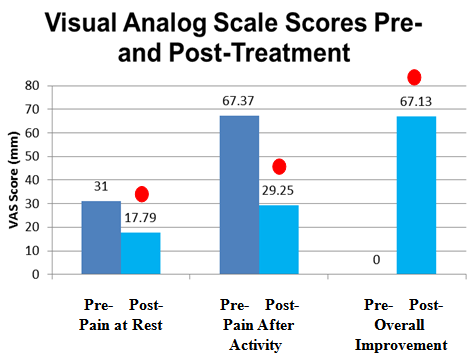
- After completing the pre-test evaluations and receiving three treatments of RSWT, the 24 participants with chronic RCT of the supraspinatous muscle completed the post-test evaluations at three months post-treatment. A Wilcoxen Signed-rank Test revealed that following the RSWT intervention, participants had a statistically significant improvement in shoulder pain on the VAS at rest (Z=-3.062, p=.002); in shoulder pain after activity (Z=-4.138, p=.0001); and for overall improvement in shoulder pain (Z=-4.11, p=.0001) (figure 1).
 | Figure 2. Mean P4 Scale scores pre- and post-treatment for shoulder pain. (- - indicates statistical significance) - indicates statistical significance) |
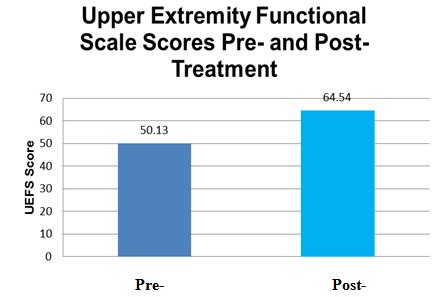 | Figure 3. Mean Upper Extremity Functional Scale scores pre- and post-treatment. ( - indicates statistical significance) - indicates statistical significance) |
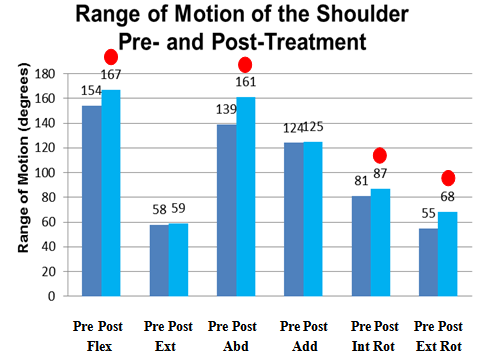 | Figure 4. Mean range of motion of the shoulder pre- and post-treatment measured in degrees. ( - indicates statistical significance) - indicates statistical significance) |
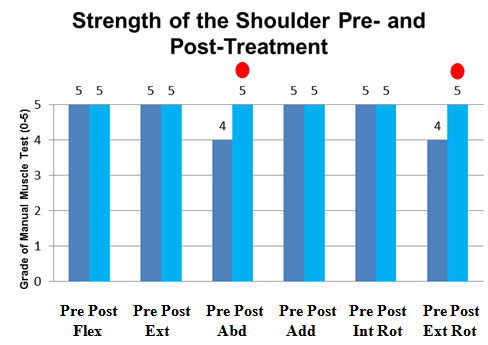 | Figure 5. Mean strength grade for resisted isometric testing of the shoulder pre- and post-treatment as measured with manual muscle testing and Oxford Scale. ( - indicates statistical significance) - indicates statistical significance) |
4. Discussion
- This study examined the effects of RSWT in participants with chronic RCT. The results revealed that RSWT improved shoulder function, reduced shoulder pain, improved ROM for active shoulder flexion, abduction, internal rotation, and external rotation, and strength for the shoulder abductors and external rotators.Radial shockwave therapy has been reported to be an effective treatment in some trials and ineffective in others, but the evidence and efficacy remains controversial [2, 10, 12, 26]. The results of this study add to the merit and body of literature supporting the use of RSWT clinically for chronic RCT.When examining, comparing, and contrasting the results of the current study with other studies, there are some key points to be highlighted. Positive effects were reported by Gerdesmeyer et al. [9], Ioppolo et al. [13], and Schofer et al. [21] with lower energy and the use of RSWT and this is consistent with the results of the present study. These authors also highlighted that better results were obtained with the use of higher energy, focused shockwave therapy which the present study did not use. Several recent systematic reviews, however, reported only moderate positive effects on pain, function, and on the overall size of the calcific deposit with the use of focused, high energy shockwave therapy in the treatment of calcific RCT but limited effects in the treatment of RCT without the presence of calcification [2, 10, 12, 26]. When attempting to compare the results across studies difficulties arise in that different shockwave generators have been used (electrohydraulic, electromagnetic, piezoelectric, radial) with varying parameters (number of impulses, energy flux density, and frequency of treatments). No consensus on the appropriate number of sessions and dosage, focal zone, and the amount of pressure that should be used for each device is available. Comparison of the data becomes even more challenging as a result.Limitations in the number of high quality and well designed studies using shockwave therapy is consistently cited but is not just unique to the use of this therapeutic intervention. A common criticism can also be applied to many other proposed clinical interventions used in the treatment of RCT and other tendinopathies and shoulder syndromes. Clinical researchers face this as an ongoing criticism to develop research projects that are meaningful and clinically relevant to clinicians but at the same time designed using sound research methods with strict controls. The counter to this argument is that in using stricter controls the meaningfulness of the findings or real world application may be lost. In addition to providing meaningful results, one of the other goals of clinical research is to foster and promote health care policy change and bring the research findings from the bench to the bed side. The present study has attempted to do this and highlight that RSWT can be used as a method of improving pain, function, ROM, and strength in patients complaining of chronic supraspinatous RCT.Some of the limitations of the current study are related to the design of the study. A one group pre-test post-test design was used and future studies should incorporate the addition of a control group or a placebo group as a comparator. A larger sample size with longer follow up as well may further add to the strength of supporting the use of RSWT in the treatment of chronic RCT. Future research combining the use of RSWT with other interventions such as education, active stretching or strengthening exercises, or with the use of other therapeutic modalities in the treatment of chronic RCT may also provide valuable information to the clinician. With the high variability in the number of types of units available, examining different types of shockwave generators in the treatment of RCT as well, may further clarify some of the mixed results in the available literature.
5. Conclusions
- Radial shockwave therapy offers a potential treatment option for patients diagnosed with chronic RCT. This therapeutic option has demonstrated the ability to improve shoulder function, decrease shoulder pain, improve shoulder ROM, and improve shoulder strength.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML
 - indicates statistical significance)
- indicates statistical significance)