D. R. Sabirov1, Sabirov Jahangir Ruzievich2
1National Cancer Research Center of the Ministry of Health, Tashkent city, USA
2Head of the Military Medical Faculty at the Tashkent Medical Academy, Tashkent
Correspondence to: Sabirov Jahangir Ruzievich, Head of the Military Medical Faculty at the Tashkent Medical Academy, Tashkent.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Abstract
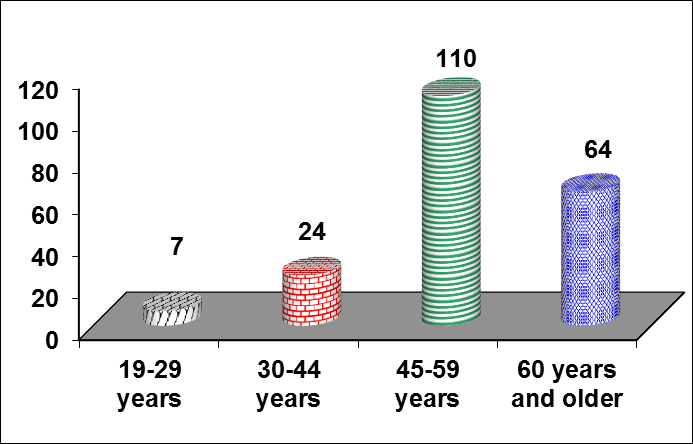
Background:The purpose of this report is improvement of the results of reconstructive operations (RO) in diseases of the esophagus and esophagogastric junction by the current advanced techniques of blood- and lymph-saving surgeries and tools with use of bipolar biactive electrocoagulation.Patients and Methods:Our experience are based on the experience of 123 reconstructive operations performed on the esophagus and esophagogastric junction in the patients (cancer of esophagus -94, cancer of esophagogastric junction – 29) treated in the clinics during the period from 2006 to 2011 in comparison with results obtained in the patients of control group including 82 patients (cancer of esophagus – 62, cancer of esophagogastric junction – 18, achlasia of the cardia -1, esophageal leucoplakia – 1) undergone operation during the period from 2001 to 2005. Fig. 1 shows distribution of the patients in relation to age.Results:Evaluation of the criteria of efficacy of the proposed technique were performed in relation to time of the operative intervention, volume of blood loss, general volume of hemotransfusion, duration of lymphorreia in drenages.The comparisons of the groups of patients in relation to technique of operation in each of studied factors was performed based on analysis of tables of conjugate, for comparison by ordinal and interval predictors the nonparametric analysis was used (test of Mann-whitney). Analysis revealed presence of reliable statistic relation with choice of the technique of operation (χ, p=0,002). The result of regression analysis will confirm significant effect on the development of complications (coefficient B 2,606, standard error 1,061, coefficient of determinate a R2= 0,177 by Hagelkerke, correctly predicted values 90,6%, p=0,0014). Conclusions:The use of bloodless method of operation by application of bipolar bioactive coagulation and dissection. At all stages of operative intervention results in reduction of number of traumaticity of operative intervention, decrease aggressiviness of the operative technique, lowering blood and lymph loss, decrease in duration of the stages of operative interventions, increase in radical degree, reduction of findings of thromboembolic complications and characteristics of infectious complications.
Keywords:
Carcinoma of the esophagus, Carcinoma of the esophagogastric junction, Esophagus extirpation, Bipolar biactive coagulation and dissection, Complications, Postoperative lethality
Cite this paper: D. R. Sabirov, Sabirov Jahangir Ruzievich, A Comparative Study between Two Different Dissection Techniques in Management of Esophageal and Esophagogastric Junction Malignant Tumors, Clinical Practice, Vol. 3 No. 2, 2014, pp. 22-27. doi: 10.5923/j.cp.20140302.03.
1. Background
At present time the majority of reconstructive operations on the esophagus and esophagogastric junction have been carried out due to malignant diseases those indicate about the importance of this pathology. The successful resolution of such difficult problem requires to be taken into consideration with a lot of the important moments. The affection of the esophagus by a malignant tumour is the most frequent disease and has the worst prognosis among the tumours of gastro-intestinal tract. Sharing 80-90% of all tumours of this organ, the cancer of the esophagus usually occupies the fifth - eighth place in the statistics among all tumours of human and third among tumours of the gastrointestinal tract. According to the data IARC - International Agency for Research on Cancer (Lyons, France) - annually on the planet the cancer of esophagus occurs in 0.4 mln of population and 0,3 mln of population die due to this disease. In Uzbekistan these parameters were 3,6 per 100000 of population in 2010. The diversity of tne approaches to the treatment and significant risk of the surgical intervention in the patients with cancer of the esophagus and esophagogastric junction induces the increased interest to this most difficult field in the clinical medicine. Hopelessness of conservative therapy and bad prognosis disease in the cancer of esophagus and esophagogastric junction cause application of operative interventions as the leading methods of treatment [1, 2, 4, 5, 6, 8, 11]. The current tendency of development of surgical treatment of the cancer of esophagus and esophagogastric junction, on the one hand, increase of radicalism of interventions at the expense of performance of wide combined resections and lympho dissection [3, 7, 8, 10, 11], on the other hand, seeking to satisfactory functional results providing the quality of life for the patients by development of more physiologic techniques of esophagoplasty [8, 10, 11].In traditional technique of surgery in cases of reconstructive operation on the esophagus and esophagogastric junction it is noted that all stages of operation are carried out by a sharp way, i.e. mobilization of a body (esophagus, stomach, greater omentum etc.), dissection of the tissue is made by scissors or by blunt way, hemostasis is made by bandaging or sutured of tissue. The sharp mobilization of esophagus with mediastinal lympho dissection often results in wound of organs of the chest, increase in blood and lympha loss, increase of intra- and postoperative complications. The acute stomach mobilization with abdominal lymphodissection increases in traumatism of operative intervention (damage of organs and structures, bleeding) and reduces radical operation in tumor process (opportunity of preservation of fatty tissue with metastatic lymph nodes). Significant quantity of blood and lympha loss, injury degree and operation duration increase in risk of occurrence of severe complications in the postoperative period, such as pulmonary artery thromboembolia, and arrhythmia, pneumonia and pleuritis, intracavitary bleeding, long lymphorrhea, infectious complications and so on.The use of the improved technique of the organ mobilization (esophagus, stomach, greater omentum and others) and tissue dissection, performance of the whole volume of lympho dissection in reconstructive operations on the esophagus and esophagogastric junction allowed to decrease in duration of operation, to create safe hemo- and lymphostasis, considerably to reduce intra- and postoperative complications, to improve remote results of operative interventions.Such contradictory opinions in technique of dissection of organs and tissues, its effect directly on the process of operation and development of postoperative period has become basis for study of own material on this question.
2. Object and Methods
Our experience are based on the experience of 123 reconstructive operations performed on the esophagus and esophagogastric junction in the patients (cancer of esophagus -94, cancer of esophagogastric junction – 29) treated in the clinics during the period from 2006 to 2011 in comparison with results obtained in the patients of control group including 82 patients (cancer of esophagus – 62, cancer of esophagogastric junction – 18, achlasia of the cardia -1,esophageal leucoplakia – 1) undergone operation during the period from 2001 to 2005.Fig. 1 shows distribution of the patients in relation to age.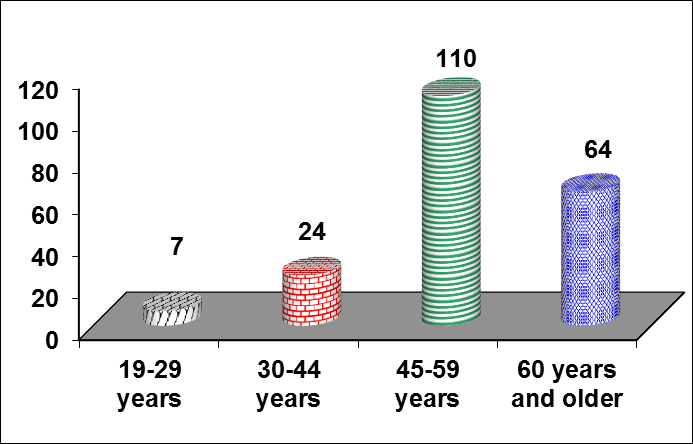 | Figure 1. Patients distribution in relation to the age |
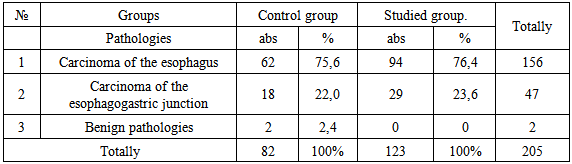
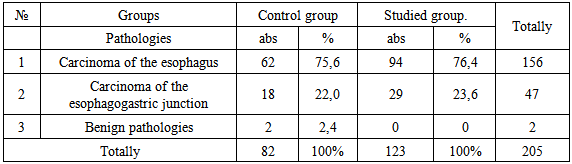
The specific weight included patients of the active age 68,8%. Out of patients 55 (43,5%) were men and 68 (55,5%) were women. Table 1 presented 205 peformed reconstructive operations distributed with regard to nosologies.Table 1. Distribution of the patients in relation to nosologies
 |
| |
|
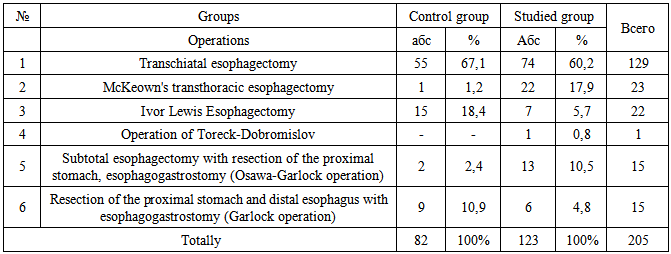
The patients of control group underwent reconstructive surgery performed with traditional technique, that is mobilization of the organ (esophagus, stomach, greater omentum and others), dissection of tissues were made by scissors or by blunt method, hemostasis was created by bandage or suturing of the tissue.The patients of the studied were carried out reconstructive operations with blood and lymph preservation with use of bipolar bioactive coagulation (BPBAC).The choice of the type of operation was made in relation to localization of the tumor process in the esophagus and esophagogastric junction, age and general state of the patient. At localization of tumor process in the upper middle toracic part of the esophagus there was performed standard McKeown's transthoracic esophagectomy (open three-field esophagectomy). At localization of cancer in the middle thoracic and lower middle parts of the esophagus as well as in the cancer esophagogastric junction type I. the choice of the type of operation was performed by the following steps: transchiatal esophagectomy (THE) was performed for patienta with low functional parameters; Ivor Lewis esophagectomy was carried out in the preserving patient. In cases of cancer of esophagogastric junction typeII the subtotal esophagectomy with resection of the proximal stomach, esophagogastrostomy (Osawa-Garlock operation) was performed, and in type III –total gastrectomy with transhiatal resection of the distal esophagus. Table 2 showed distribution of the surgical interventions with regard to volume of operation.Table 2. Distribution of the patients in relation to volume of operation
 |
| |
|
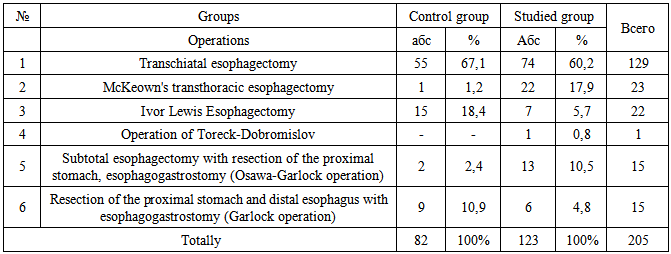
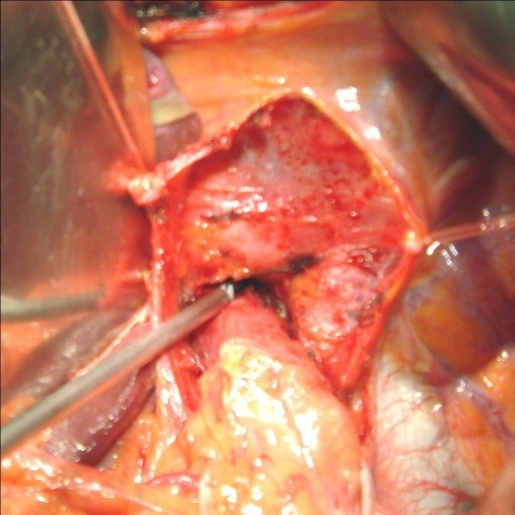
Depending on a level of the esophagus impairment in 4 (1,9%) patients the tumor process was located in the upper thoracic portion, in 128 (61,9%) – in the midthoracic, and in 14 (6,8%) lower portion, in 12 (5,8%) cases there was noted lesion of the mid-lower thoracic portion of esophagus, cance of the esophagogastric junction type I (by Siewert J.R.) in 17 (8,3%) type II of lesion of esophagogastric junction was noted in 30 (14,6%) cases. Among the operated patients due to malignant pathology 184 (89,7%) patients were operated at stage III (ТЗN1МО, Т4NanyМО). Of them cervical esophagogastroanastomosis was formed in 152 (74,1%), in a dome of right pleural cavity in 22 (10,7%), in the posterior mediastinum in 15 (7,3%), and in peritoneal cavity in 15 (7,3%) patients. Histological structure of tumor was squamous cancer in 162 (79,0%) patients, adenocarcinoma in 40(19,5%) case, and MALT lymphoma in 3 (1,5%) cases.There is presented description of the technique of blood and lymphs preserving operation with use of bipolar bioactive coagulation (BPBAC): mobilization of the esophagus with mediastinal lympho, mobilization and resection of the stomach, abdominal lympho dissection and omentectomy performed by bipolar coagulation forceps by staged use of the regime of coagulation and cutting (the set should include bipolar forceps of different size and form). If it is necessary the dissection of the tissue with scissors is made only after preliminary coagulation between branshes of the bipolar bioactive coagulation forceps (BPBAC) (diaphragm pulmonary ligaments, gastric ligaments, scarry tissue). Mobilization of the esophagus with use of forceps BPBAC. The detachment of the fatty tissue from precardium, low pulmonary ligaments, crossing of the lateral esophageal ligaments were performed by dissection between branshes of the BPBAC forceps (in the depth the endosurgical bipolar instrument endodissector is used) and stage by stage the anterior and lateral esophageal walls with the tumor will be mobilized to and above trachea bifurcation. The figures present mobilization with lympho dissection. | Figure 2. The stage of esophagus mobilization with use of bipolar coagulation |
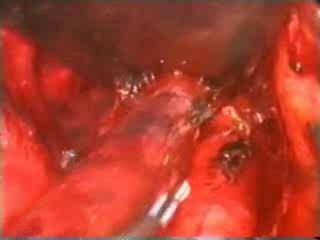
Then the posterior esophageal surface is mobilized by similar method separating it from prespinal fascia and aorta. All esophageal mobilization is performed with simultaneous monoblock separating of paraesophageal fatty tissue with lymph nodes and lympho collectors (not only lymph nodes, but all lymph apparatus including lymph vessels, nervous plexus with surrounding fatty tissue) by staged coagulation of tissues between nranshes BPBAC. Sometimes the structures of mediastinum are carefully palpated (pericardium, pulmonary arteries and veins) with palm of the hand; the esophagus is separated from membranous part of trachea and major bronchi. Further immediately zone of mobilization is visually controlled if it is necessary electrodissection is performed by endosurgical forceps BPBAC, peribronchial lymph nodes are removed.If the esophageal tumor involves the pericardium, the impaired site is dissected after staged coagulation between branshes of forceps BPBAC. In case of tumor invasion into the mediastinal pleura it is also resected between branshes of the BPBAC forceps. Figure 3 showed mobilized esophagus, hemostasis of the doubtful sites.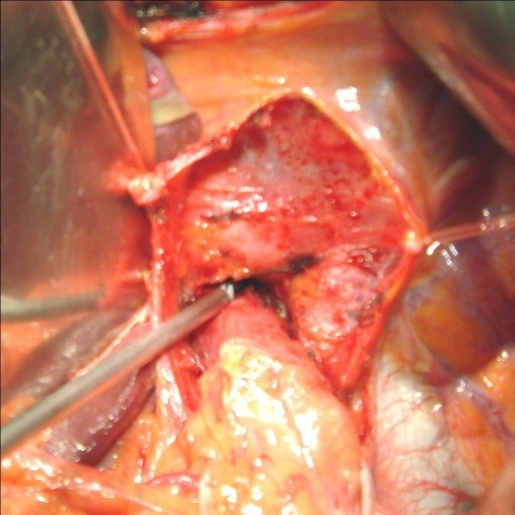 | Figure 3. The stage of lumpho dissection with use of endodissector |
 | Figure 4. The mobilized esophagus, hemostasis of the doubtful sites |
Separation of the tissues in burn (and some times in peptic) strictures with marked periesophagitis can be performed with use of the technique of partial staged bipolar bioactive electrocoagulation with BPBAC forceps.Mobilization of the stomach with use of BPBAC forceps. Mobilization of the stomach begins with mobilization of duodenum by Cocher together with head of pancreatic gland by dissection of the tissues between branshes of BPBAC forceps. The stomach is mobilized along the greater curvature with preservation of the right ventricle-omentum vessels with crossing of the tissues by staged bipolar coagulation between branshes of BPBAC forceps located as far as possible from the greater perigastric arch. If operation is performed due to esophageal cancer or cancer of the cardia with invasion into the esophagus, then lymphadenectomy was performed in volume D2 with use of BPBAC forceps. The use of BPBAC forceps allows maximally and fastly to remove the fatty tissue, maybe having already metastatic lymph nodes. The right ventricular artery is crossing and ligated under the pylorus at the place of its deviation from its own hepatic artery after it opening and maximal removal of its surrounding fatty tissue with BPBAC forceps. In case of need the lympho dissection is performed in the projection of the ehad of pancreatic gland.
3. Results and Discussion
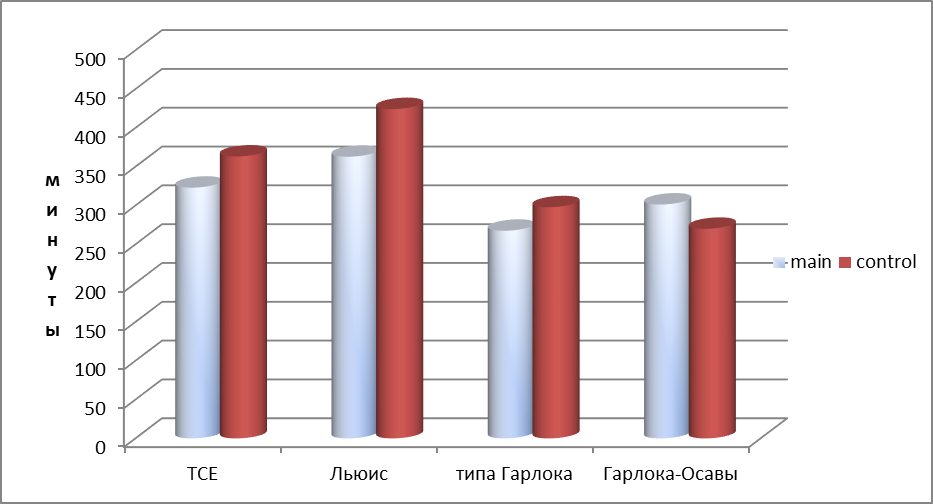
Evaluation of the criteria of efficacy of the proposed technique was performed in relation to time of the operative intervention, volume of blood loss, general volume of hemotransfusion, duration of lymphorreia in drenages.The comparisons of the groups of patients in relation to technique of operation in each of studied factors were performed on the basis of analysis of tables of conjugate, for comparison by ordinal and interval predictors the nonparametric analysis was used (test of Mann-whitney). Analysis revealed presence of reliable statistic relation with choice of the technique of operation (χ, p=0,002). The result of regression analysis will confirm significant effect on the development of complications (coefficient B 2,606, standard error 1,061, coefficient of determinatia R2= 0,177 by Hagelkerke, correctly predicted values 90,6%, p=0,0014) [9].The patients having previously operation by McKeownand Osawa-Garlock, were excluded from the comparative analysis because the quality of patients in the control group accounts for only one and two, respectively.Fig. 5 presents time (min) of operative intervention. There was revealed statistically reliable deffirence in use of the offered technique in comparison with the common one (p<0,05), thus in tanschiatal esophagectomy in the control group this time was 363 min, in the studied group – 323 min. In case of operation by lewis type the time in control group was 44,3 min, in the studied group – 362,9 min. On the average in groups these values were: in control – 403,2 min, studied group – 331,6 min.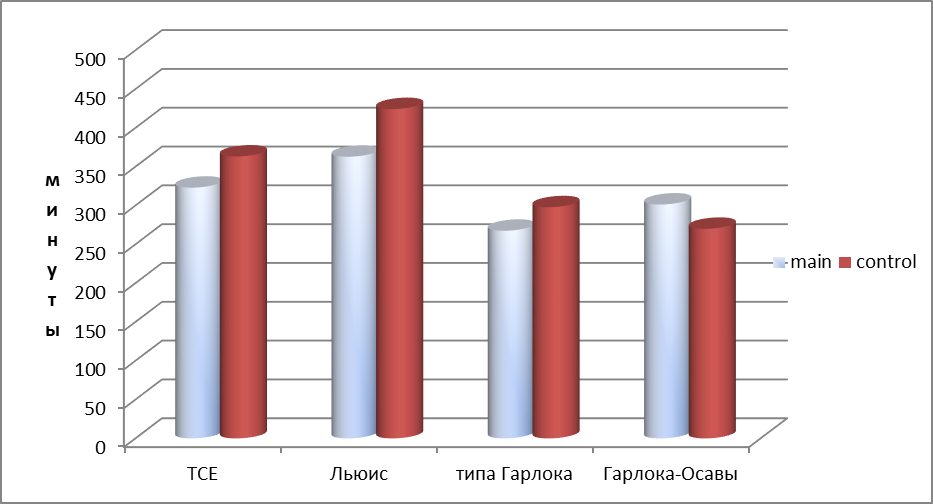 | Figure 5. Duration of operative intervention with regard to choice of operation |
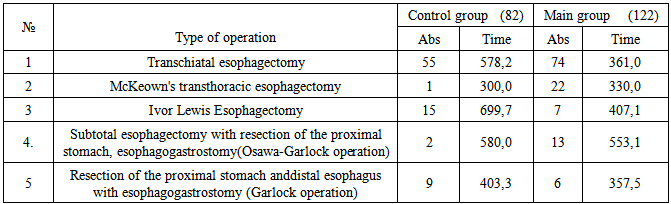
The next criterion was evaluation of the volume of intraoperative blood loss. There was revealed statistically significant difference in use of the technique proposed in relation to the common ones (p<0,05), thus, in transchiatal esophagectomy in control group the volume of blood loss was 578,2 ml, in the studied group 361 ml, in Ivor Lewis esophagectomy– 699,7 ml, in the studied group 407,1 mln, in subtotal esophagectomy with resection of the proximal stomach, esophagogastrostomy– 403,3 ml, in studied group – 357 ml. On the average in groups: 576,0ml, in studied group – 378,5 ml. In Table 3 there is presented volume of intraoperative blood loss in relation to technique of operation.Table 3. Distribution of the patients in relation to volume of blood loss (ml)
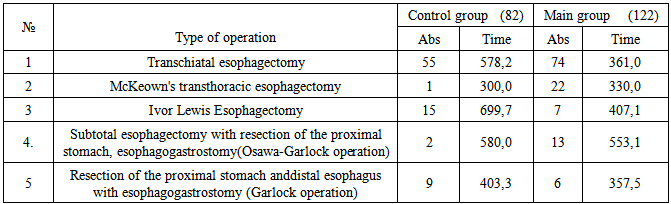 |
| |
|
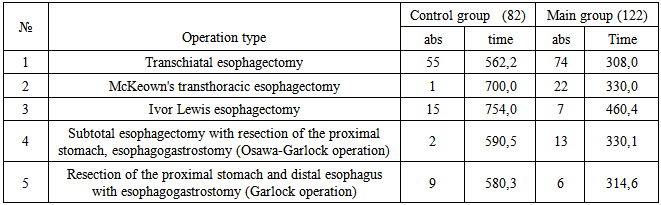
Table 4. Distribution of the patients in relation to volume of hemotransfusion (ml)
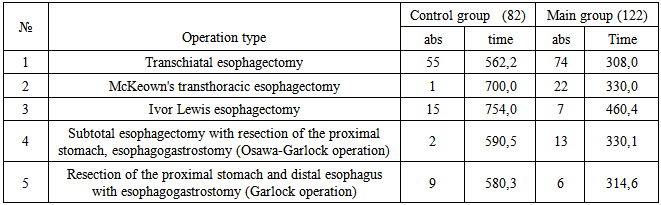 |
| |
|
The other criterion for evaluation was evaluation of the total volume of hemotransfusion, there was proved statistically significant difference in use of proposed technique in comparison with traditional (p<0,05), thus in transchiatal esophagectomy in the control group the volume of hemotransfsion was 562,2 ml, in the studied group 308 ml, in Ivor Lewis esophagectomy: in control group -754,0 ml, studied group – 506,4 ml, in resection of the proximal stomach and distal esophagus with esophagogastrostomy in control group – 580,3 ml, studied group – 328,6 ml. On the everag in groups: control -594,0 ml; studied group – 347,0 ml.The duration of lymphorrheia in drainages in the control grop during 10-14 day was noted in 7 (8,7%) patients, in the studied group this parameter was noted in 3 (3,6%).In early postoperative period after transchiatal esophagectomy the complicated development was noted in 24 (15,7%) patients, after McKeown's transthoracic esophagectomyin 19 (57,6%) patients and after Ivor Lewis esophagectomyin 40 (63,5%). Analysis of postoperative complications showe, that after transchiatal esophagectomy mainly reactive pleuritis occurred (to 7,5%), after McKeown's transthoracic esophagectomy and Ivor Lewis esophagectomy pulmonary (to 24,6%) and pleural (to 23,3%) complications. Postoperative bed-day, on the average, in control group was 27,6±2,3 days, in the studied group – 20,4±2,1 days.Total postoperative lethality was 6,02% (15 patients), and in this case: after transchiatal extirpation accounts for 6(3,9%), after thre-stage – 2(6,1%) and after transthoracic esophagus extirpation – 7(11,1%). The causes of death after transdiaphragmatic esophagus extirpation were as thromboembolia of the pulmonary artery in 4 cases, acute myocardial in faction in 2 cases. The acute pneumonia was a cause of decompensated respiratory insufficiency after thre-sage esophagus extirpation in 2 cases. The failure of the intrapleural esophagogastro anastomosis in 6 cases and acute pneumonia in 1 case after transthoracic extirpation finished by lethal outcome.Thus, the use of bipolar bioactive coagulation at the all stages of operative intervention allowed to reduce sharply the time of operation from 403-,2 min to 331,6 min, to reduce volume of blood loss from 576,0 ml to 378,5 ml, to achive lymph preserving effect, to minimize intra- and postoperative hemotransfusion.
4. Conclusions
The use of bloodless method of operation by application of bipolar bioactive coagulation and dissection. At all stages of operative intervention results in reduction of number of traumaticity of operative intervention, decrease aggressiviness of the operative technique, lowering blood and lymph loss, decrease in duration of the stages of operative interventions, increase in radical degree, reduction of findings of thromboembolic complications and characteristics of infectious complications.
References
| [1] | Bessa S.S., Al-Fayoumi T.A., Katri K.M., et al., “Clipless laparoscopic cholecystectomy by ultrasonic dissection,” Journal of Laparoendoscopic and Advanced Surgical Techniques A, vol. 18, no. 4, pp. 593-598, 2008. View at Publisher · View at Google Scholar. |
| [2] | Carbonell A.M., Joels C.S., Kercher K.W., Matthews B.D., Sing R.F., Heniford B.T. A comparison of laparoscopic bipolar vessel sealing devices in the hemostasis of small-, medium-, and large-sized arteries. J Laparoendosc AdvSurg Tech A 2003;13:377-80. |
| [3] | Entezari K, Hoffmann P, Goris M, Peltier A, Van Velthoven R. A review of currently available vessel sealing systems. Minim Invasive Ther Allied Technol 2007;16:52-7. |
| [4] | Harrell A.G., Kercher KW, Heniford BT. Energy sources in laparoscopy. SeminLaparoscSurg 2004;11:201-9. |
| [5] | Karl R.C., Schreiber R., Boulware D., Baker S., Coppola D.Factors affecting morbidity, mortality, and survival in patients undergoing Ivor Lewis esophagogastrectomy. Ann Surg. 2000 May;231(5):635-43. |
| [6] | Orringer M.B., Marshall B., Iannettoni M.D. Eliminating the cervical esophagogastric anastomotic leak with a side-to-side stapled anastomosis. J ThoracCardiovasc Surg. 2000 Feb;119(2):277-88. 6. Sugimachi K., Okudaira Y. // Jpn. J. Cancer Clin. - 1986 - Vol.32 N 10. - P. 1153-1156. |
| [7] | Newcomb WL, Hope WW, Schmelzer TM, et al. Comparison of blood vessel sealing among new electrosurgical and ultrasonic devices. SurgEndosc 2009;23:90-6. |
| [8] | Tachibana M., Yoshimura H, Kinugasa S, Dhar DK, Shibakita M, Ohno S, Ueda S, Fujii T, Nagasue N. Clinicopathologic factors correlated with number of metastatic lymph nodes in oesophageal cancer. Dig Liver Dis. 2001 Oct;33(7):534-8. |
| [9] | Tharwat Kandil, Ayman E. Nakeeb, Emad E. Hefnawy. Comparative study between clipless laparoscopic cholecystectomy by harmonic scalpel versus conventional method: a prospective randomized study. Journal of Gastrointestinal Surgery (Impact Factor: 2.36). 10/2009; 14(2):323-8. DOI:10.1007/s11605-009-1039-8. |
| [10] | Taziev P.M., Sigal E.I., Chernyshov V.A. Cancer of the oesophagus: surgical and multifunction treatment/ // Russian oncology journal. 2002. - №1. - С. 9-13. |
| [11] | Чиссов В.И.// Пути развития хирургического органосохранного лечения в онкологии. Вопросы онкологии. - 2002. - № 4-5. - С. 463-467. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML