-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2014; 3(2): 14-21
doi:10.5923/j.cp.20140302.02
Therapeutic Taping of the Knee and Its Effect on Lower Quadrant Range of Motion and Strength
Paolo Sanzo, Carlos Zerpa, Eryk Przysucha, Daniel Vasiliu
School of Kinesiology, Lakehead University, Thunder Bay, Canada
Correspondence to: Paolo Sanzo, School of Kinesiology, Lakehead University, Thunder Bay, Canada.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Objective: To investigate the effects of different taping techniques (no tape, placebo, Kinesiotape, Leukotape) on lower extremity range of motion (ROM) and strength. Design: Randomized, one group pre-test post-test design. Subjects:10 healthy male and female university students. Methods: Participants completed four testing sessions randomly receiving different types of taping techniques. Hip, knee, and ankle ROM and strength were measured with and without tape. ROM and strength change scores were computed by subtracting pre-test from post-test scores. The data were analyzed using descriptive statistics and two way repeated measures ANOVAs. The rejection criteria were set at an alpha level < .05. Results: Inferential statistics revealed a significant interaction effect between type of tape and movement type in relation to hip ROM change scores, F(15,135)=1.73, p=.05; and significant interaction for type of tape and movement type in relation to knee ROM change scores, F(9,81)=3.92, p=.0001. There was also a significant interaction effect between type of tape and movement type in relation to knee strength change scores (p=.028). Conclusions: Taping of the knee resulted in reduced hip and knee mobility. The application of Leukotape reduced knee ROM more and should be considered when choosing a type of tape. Taping affected knee strength but there was not a consistent difference between the types of tape used.
Keywords: Leukotape, Kinesiotape, Placebo, Range of motion, Strength, Hip, Knee, Ankle
Cite this paper: Paolo Sanzo, Carlos Zerpa, Eryk Przysucha, Daniel Vasiliu, Therapeutic Taping of the Knee and Its Effect on Lower Quadrant Range of Motion and Strength, Clinical Practice, Vol. 3 No. 2, 2014, pp. 14-21. doi: 10.5923/j.cp.20140302.02.
Article Outline
1. Introduction
- Therapeutic taping is commonly used to treat a variety of musculoskeletal disorders in the knee, shoulder, ankle, cervical spine, and lumbar spine regions. In recent years, the vibrant colours of certain types of tape and high profile media exposure with its use on athletes during the Olympic Games have provided a lot of interest and an increase in its use. The hypothesized effects of therapeutic taping include the facilitation, and in some cases the inhibition, or alteration of the timing of muscle activity [1-5]; the realignment of joint position [6-8]; the improvement in proprioception [9, 10] and; the reduction in pain and frequency of injury [11-13]. The true merit and efficacy of therapeutic taping is controversial as there is conflicting evidence present on the proposed effects. Despite the questions about its utility, taping continues to be widely used to treat a variety of musculoskeletal disorders. A common disorder in which therapeutic taping is used is patellofemoral pain syndrome (PFPS).Knee pain secondary to PFPS is a common complaint with the incidence ranging from 3% to 40% [14]. It is reported to be one of the most common causes of knee pain in active adults and adolescents [15]. In the United States, the incidence rate for PFPS is 22 cases/1000 persons per year with females having a 2.5% higher prevalence than males [16]. In Britain, PFPS accounts for approximately 5% of all injuries seen in the athletic population, and 25% of all knee injuries [16]. The development of PFPS also impacts on the overall cost of healthcare as it has been reported to lead to the development of long lasting knee pain and osteoarthritic changes that may involve much costlier interventions [13].Although the exact cause and pathophysiology of PFPS is unknown, several hypotheses are present. PFPS may be the result of abnormal patellar tracking that results in excessive compressive forces on the posterior aspect of the patella. Another hypothesis is that PFPS develops because of structural abnormalities in the lower quadrant such as an increased quadriceps angle or a by malpositioned patella that may affect the orientation, pull, and the force generated by the quadriceps muscle [6, 11, 15]. This structural abnormality may indirectly affect the tracking of the patella and the centralization of the knee cap within the trochlear fossa leading to increased shear and compressive forces in the knee and the subsequent development of PFPS [18]. PFPS may also be associated with abnormal length tension and flexibility issues in the muscles and tissues that cross the knee [9]. Abnormal length in the iliotibial band, or vastus lateralis, rectus femoris, hamstring, or gastrocnemius muscles, for example, may further impact the tracking of the patellofemoral joint [9]. PFPS may also develop due to muscular imbalances related to strength and endurance issues in the lower quadrant muscles such as insufficiency in the vastus medialis or gluteal muscles [9].Interventions for PFPS include stretching and strengthening exercises, activity modification, therapeutic modalities such as biofeedback or electrical neuromuscular stimulation, bracing, and therapeutic taping [15]. There are a variety of taping techniques used clinically in the treatment of PFPS, but the exact mechanism of their effects is unknown with variable findings reported [9, 11]. Kinesiotape (KT) and Leukotape (LT) are two types of tape most commonly used clinically. The number of studies available examining the effects of therapeutic taping on pain, function, range of motion (ROM), strength, kinetics, kinematics, and muscle activity is limited and controversial [19]. In a study completed by Callaghan and Selfe [20] patients reported an instantaneous improvement in pain and function with the application of tape but longer term effects were uncertain. Other systematic reviews have reported that the current evidence does not support the use of therapeutic taping [21-23]. Limited studies examining the effects of therapeutic taping on ROM and strength are present and the studies that are available present conflicting results or no significant effects [24-26]. When researchers have attempted to examine the effects of therapeutic taping, the use of a placebo comparative group, the effects of the tape on proximal and distal joints, and the comparison of one method or type of tape directly to another is lacking. Many of the muscles around the knee joint span multiple joints including the hip and ankle. As a result, the application of therapeutic taping to the knee may impact on the quadriceps femoris or gastrocnemius muscles, for examples, and may affect the hip or ankle joint. Therefore, the purpose of this pilot study was to investigate the effects of no tape to the application of three different types of taping techniques (placebo taping, KT, and LT) on hip, knee, and ankle ROM and strength in a group of healthy controls.
2. Methods
2.1. Subjects
- Participants included 10 healthy university students who did not have a history of knee pain. Healthy participants were defined as individuals without any current or previous history of knee pain, surgery, or dysfunction; nor any other medical conditions or diseases that would preclude participation. Participants who had knee pain; any previous traumatic, inflammatory, or infectious pathology in the lower extremity; fracture, dislocation, or subluxation of the patella; surgery to the knee; signs or symptoms of osteoarthritis; or allergies to adhesive taping were excluded from the study. A total of 5 participants were excluded from the study. Two participants were excluded from the study due to the fact that they were asymptomatic but had previous knee surgery. Three participants met the inclusion criteria but chose not to participate due to the time commitment and number of testing sessions required.
2.2. Apparatus
- A long arm Baseline® Absolute-Axis™ plastic goniometer was used to complete all of the ROM measures. The use of a measurement device with strong evidence of reliability and validity is an important prerequisite for assessment in clinical practice, as well as for the collection and interpretation of research results [27]. This method of ROM measurement has been reported to be an accurate method of determining joint mobility. The reliability of goniometric ROM measurements has been reported to range from fair (intra-class correlation (ICC) intra-tester 0.82; ICC inter-tester 0.68) [28] to high for knee flexion (ICC intra-tester 0.99; ICC inter-tester 0.90) [29]; and high for knee extension (ICC intra-tester 0.98; ICC inter-tester 0.86) [29]. The variability in reliability when measuring ROM may be due to the utility of the instrument, but may also be due to the anatomical variation of the landmarks in the subject, and in the ability of the investigator to locate the joint fulcrum [27]. The reduction of measurement error and the improvement in the reliability of this measure can be achieved by testing ROM with the patient positioned in supine lying, using a set of standardized instructions and landmarks, and using only one investigator to complete the measures [28].A Baseline® Electronic Push-Pull Dynamometer (500 lbs capacity) was used to complete all of the resisted isometric strength measures. Manual muscle testing continues to be the most commonly used method of measuring muscular strength [31]. Measurements of muscular strength with the use of a dynamometer has been reported to be superior and to have moderate to strong correlations (0.48-0.90) [32-34].
2.3. Procedure
- Once the project received ethical approval by the university ethics board, the purpose and methodology of the study was explained, verbal and written consent was obtained, and participants completed a Waterloo Footedness Questionnaire. This was completed in order to determine foot dominance as the participants dominant leg was used for testing purposes. The order of the taping interventions, ROM, and strength testing was randomized. During the initial test session, age, and anthropometric measures (height in centimeters, weight in kilograms) were also taken. Bony landmarks were identified and ROM of the hip (flexion, extension, abduction, adduction, internal rotation, external rotation), knee (flexion, extension, internal rotation, external rotation), and ankle (plantarflexion, dorsiflexion, inversion, eversion) were measured. The subject was positioned in supine lying and maximal ROM was measured (in degrees) in a single trial for each movement using a long arm goniometer. All goniometric measurements and land marking were performed by a single examiner according to the techniques described by Norkin and White [35]. Three repetitions of hip, knee, and ankle strength were also measured (in lbs. of force) using a Baseline Manual Muscle Tester for the movements described above. The joint was positioned in its resting position and the mean strength of three trials of resisted isometric testing was recorded for each movement.Participants completed four separate testing sessions using a different type of tape for each session. Testing sessions were scheduled approximately 24 to 48 hours apart but was dependent on the participant’s availability. The colour of the tape was the same for each type and brand. This approach was implemented for the purpose of blinding the participant to the intervention received based on the colours of the tape and to minimize any bias that the tape colour may have introduced. The order of the interventions (no tape, placebo, LT, KT) was also randomized. Strength and ROM measures were completed with no tape followed by measures taken after the application of the tape. The study design flow diagram is illustrated in Figure 1.
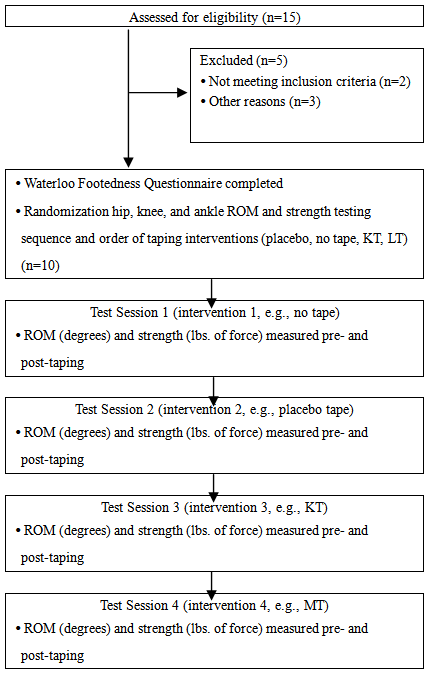 | Figure 1. Study design flow chart |
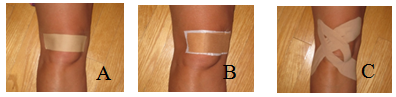 | Figure 2. Placebo taping (A), LT (B), and KT techniques (C) |
3. Results
- The sample consisted of 10 normal, healthy university students (4 females, 6 males); mean age 24 years ±7.1; height 170 cm ±10.8; and weight 69 kg ±14.4. There was a significant interaction effect for the type of tape on movement type in relation to hip ROM change scores F(15,135)=1.73, p=.05. As depicted in Figure 3, the type of tape affected hip movement by resulting in a decrease in the ROM. While significant differences were found across different types of tape, F(3,27)=5.11, p=.006, pair mean comparisons only revealed a significant difference between no tape and placebo tape.
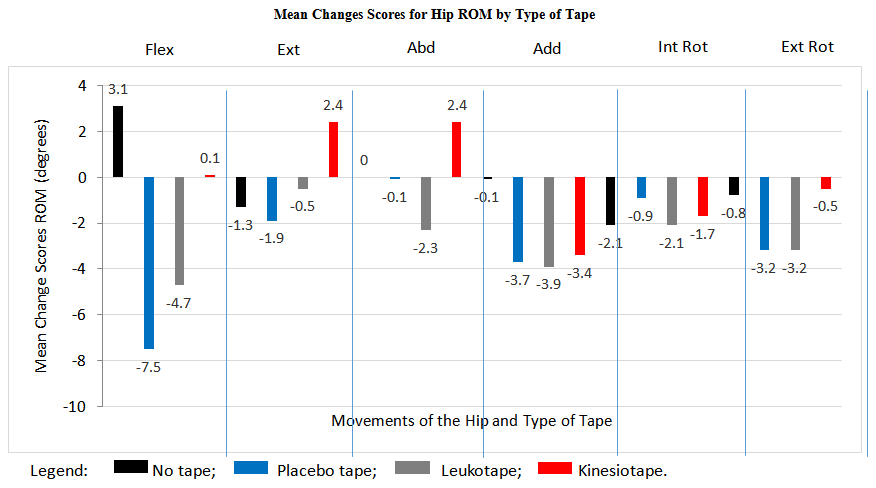 | Figure 3. Mean changes scores for hip ROM by type of tape |
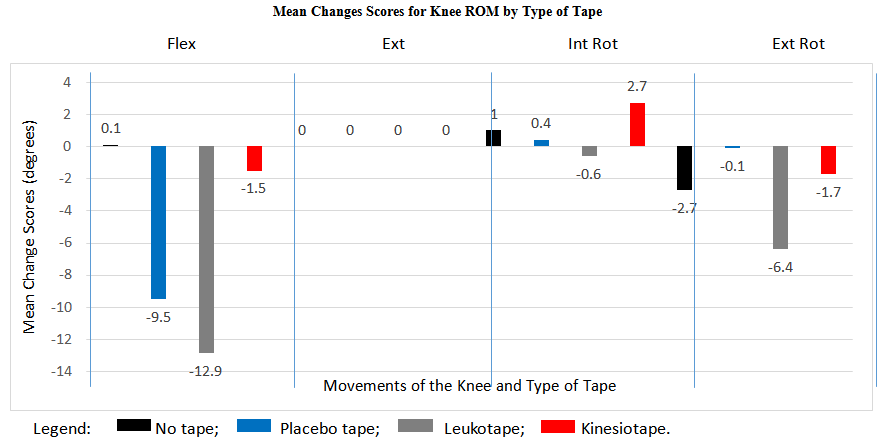 | Figure 4. Mean changes scores for knee ROM by type of tape |
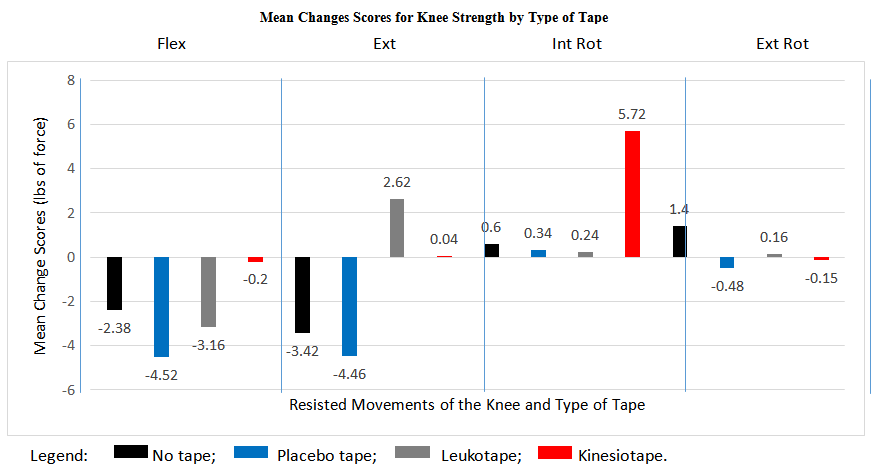 | Figure 5. Mean changes scores for knee strength by type of tape |
4. Discussion
- The use of taping for PFPS continues to be commonly used clinically as a therapeutic intervention. The findings of the current pilot study are consistent with some of the reported effects in that it primarily has a significant effect on the ROM of the hip and on the ROM and strength of the knee. At the hip joint the application of taping to the knee primarily had a trend of slightly reducing the available hip ROM. The greatest change in hip joint ROM was in flexion in which no tape resulted in an increase by 3.1 degrees of flexion compared to a reduction by 7.5 degrees for hip flexion with the application of placebo taping. For all other hip movements the application of tape resulted in no change or a slight reduction in ROM by 2-3 degrees. Such a small change in ROM may be clinically insignificant from a functional perspective but further investigation is required.When examining the effects on knee ROM, therapeutic taping also generally had a tendency to reduce knee mobility. LT resulted in the greatest decrease in knee flexion and external rotation ROM. LT also resulted in a greater reduction than KT and this may have been due to the lack of elasticity present in the LT. The KT is very elasticized and had little effect on ROM. This may be a clinically significant consideration for the healthcare provider that is using LT in a patient that must perform a functional activity or work task, or in an athlete that is involved in a sport that requires significant amounts of knee flexion. The optimal choice for the healthcare provider may be to use KT as this will not result in a restriction in knee flexion and simultaneously provide other therapeutic effects that the practitioner may be hoping to achieve. LT is more rigid than the zinc oxide tape that was used for the placebo taping intervention and this was readily apparent with a greater reduction in knee flexion ROM with the LT. With regards to the effect on knee strength, the application of taping does not appear to effect knee strength change scores.Although we are not able to make specific inferences based on cause and effect from the current study, the application of therapeutic taping to the patellofemoral joint appears to affect the ROM of the hip and knee. There was, however, no significant effect of therapeutic taping to the ankle joint. This is consistent with some of the studies that have reported ROM effects with the application of therapeutic taping on other joints [37, 38]. Some of the proposed mechanisms described in other studies by which ROM may be affected include a change in blood flow to the taped area and the induction of a physiological change that facilitates a change in ROM [38]. It has also been proposed that ROM changes may be related to a sensory feedback system that reduces the fear of movement in patients that have pain [37]. In the present study participants were pain free so there may be another neurophysiological feedback loop not related to pain that may be affecting ROM. Due to the limited number of studies that have examined the effects of therapeutic taping on joint ROM, further study is required to elucidate on these proposed mechanisms and conclusively state what the therapeutic effects are related to.Therapeutic taping did not have a consistent and statistically significant effect on knee strength (slightly decreased knee flexion and extension strength and increased knee internal and external rotation strength) and this is contradictory to some of the reported research findings [39, 40]. Vithoulka et al. [39] reported an improvement in quadriceps eccentric peak torque when compared to placebo taping or no taping in a sample of female non-athletic participants. Fu et al. [40] also reported similar results with an improvement in the peak torque with concentric quadriceps contractions in healthy collegiate athletes. In the present study, the use of placebo taping or no taping resulted in a decrease in knee extensor strength compared to a slight increase in strength when LT and KT were applied. The methodological assessment of strength and instrumentation used in the current study differs from the previous studies in that the present study examined static maximal resisted isometric strength rather than eccentric peak torque or isokinetic strength measures. Further research is required, however, to determine whether different types of tape have an effect on strength in a pathological population, if there is any long term effect on strength changes, and to determine the exact mechanism by which this is achieved.In the present pilot study, attempts were made to integrate suggestions in the study design from other researchers that had previously examined the use of therapeutic taping in a variety of populations. The current authors used a consistent colour of tape as a method of blinding the participant to the intervention that was received and also examined the effect of tape on multiple joints. This has been highlighted in previous systematic reviews and meta-analyses as potential weaknesses of the available studies [22, 23]. As a result, an attempt was made to integrate these suggestions into the current design. The extrapolation of the findings of this pilot study, however, are limited due to the small sample size, and further research is required with a larger sample size, and with the application to a symptomatic population.The current study design, however, examined and compared the use of multiple types of tape in comparison to a placebo and no tape group within one study. This type of comparison examining the effect on proximal and distal joints, over multiple testing sessions is unique and adds valuable information to the limited data on therapeutic taping. With a larger sample size, and the combination of this information with the kinematic, kinetic, and surface EMG data, the effects of different taping techniques can be further explored in the future.Future research work will examine joint ground reaction forces using a force platform, muscle recruitment patterns in the lower extremity using surface electromyography, and lower extremity and patellar kinematics using 2D video analysis. These data have already been collected for the functional movements of sit to stand, vertical jump, and full squat with and without tape. The results shall be reported in a future submission.
5. Conclusions
- The application of therapeutic taping to the knee appears to have an effect on hip ROM and on knee ROM and strength production. In the knee, the application of more rigid tapes like LT and zinc oxide tape may reduce knee ROM and this outcome may be a consideration for the healthcare provider when choosing which type of tape to use. In the case of knee strength, the application of different taping techniques does not appear to have a consistent effect between types of tape. Further research is required to determine the exact effects of tape on the ROM and strength of proximal and distal joints.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML