-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2014; 3(1): 7-10
doi:10.5923/j.cp.20140301.03
Hereditary Gingival Fibromatosis - A Case Report
Anand Kishore1, Vivek Srivastava2, Ajeeta Meenawat2, Ambrish Kaushal3
1King George Medical College, Lucknow
2BBD College of dental sciences
3Chandra Dental College & Hospital
Correspondence to: Anand Kishore, King George Medical College, Lucknow.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Hereditary gingival fibromatosis is characterized by a slow benign enlargement of gingival tissue. It causes teeth being partially or totally covered by enlarged gingiva, causing esthetic and functional problems. It is usually transmitted both as autosomal dominant trait and autosomal recessive inheritance although sporadic cases are commonly reported. This paper reports three cases of gingival fibromatosis out of which one was in a 15 year old girl treated with convectional gingivectomy.
Keywords: Hereditary gingival fibromatosis, Inherited disease, Gingivectomy
Cite this paper: Anand Kishore, Vivek Srivastava, Ajeeta Meenawat, Ambrish Kaushal, Hereditary Gingival Fibromatosis - A Case Report, Clinical Practice, Vol. 3 No. 1, 2014, pp. 7-10. doi: 10.5923/j.cp.20140301.03.
1. Introduction
- Hereditary gingival fibromatosis (HGF) or Idiopathic gingival fibromatosis is a rare, benign, asymptomatic, non-hemorrhagic and non-exudative proliferative fibrous lesion of gingival tissue occurring equally among men and women, in both arches with varying intensity in individuals within the same family [1]. It occurs as an autosomal dominant condition although recessive form also does occur. Consanguinity seems to increase the risk of autosomal dominant inheritance. It affects the marginal gingival, attached gingival and interdental papilla presenting as pink, non-hemorrhagic and have a firm, fibrotic consistency [2].It also shows a generalized firm nodular enlargement with smooth to stippled surfaces and minimal tendency to bleed. However, in some cases the enlargement can be so firm and dense that it feels like bone on palpation [3]. Here we present three cases of gingival fibromatosis out of which one was in a 15 year old female patient.
2. Case Reports
- A 15 year old female patient came to the department of periodontics at CDC hospital, Lucknow (U.P), India with chief complaint of generalized gingival swelling since 3 years (Fig. 1). On accounting detail history the patient revealed that the swelling initiated slowly and has assumed the present size within 3 years. On further communication with the patient it was revealed that her mother was also having the gingival enlargement before the patient’s birth and she got operated in the village government hospital. No further relevant medical history was present.
 | Figure 1. Gingival enlargement |
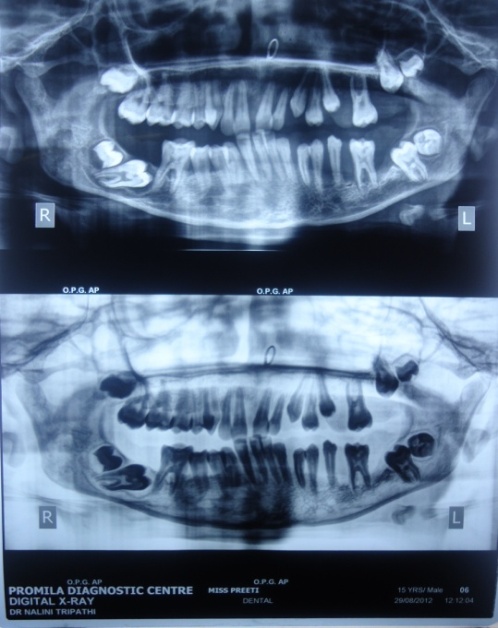 | Figure 2. OPG showing impacted molars |
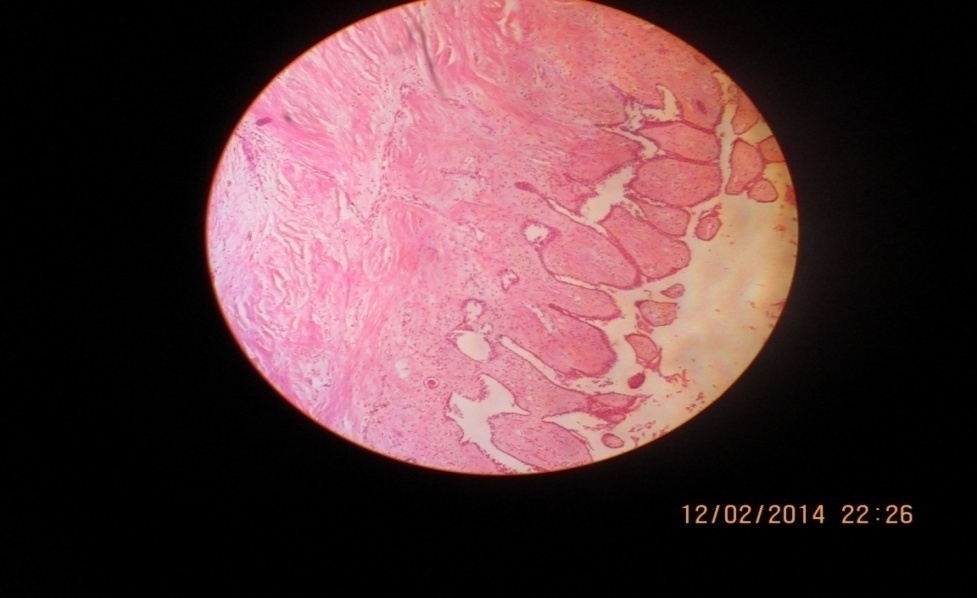 | Figure 3. Showing irregular fibrosis & inflammation |
 | Figure 4. Showing the surgery performed under LA |
 | Figure 5. Post operative showing no recurrence |
 | Figure 6 & 7. Showing localized gingival enlargement treated with electrocautery in cutting and coagulation mode |
3. Discussion
- Hereditary gingival fibromatosis is also associated with Rutherford, Laband, Murrey-Puretic-Drescher, Cross and Ramon syndrome. It is also seen in Lysosomal storage disease [3]. It is a rare benign fibrous growth of gingiva with genetic and clinical heterogeneity. It manifests as an isolated form which is mostly sporadic or with an syndrome. The etiological factors contributing for gingival fibromatosis reported were administration of certain drugs (Phenytion, Cyclosporine, Nifedipine), inflammation, systemic conditions (leukemia), hormonal conditions (Pregnancy, puberty or Hyperthyroidism) and nutritional conditions like Vitamin C deficiency [4].In the present case the patient has not reported any systemic disease or any dependency on medication. On clinical examination neither syndromic signs were revealed nor the hemogram did showed any abnormality. It was assumed that the patient may be suffering from scurvy but there were no signs of petechiae, echymosis or spontaneous bruising of the extremeties.A chromosomal abnormality involving 2p21-p22 and 5q13-q22 has been found in HGF. A mutation in the son of sevenless-1 (SOS-1) gene has also been suggested as the possible cause. An unknown cause of HGF confined to the fibroblasts in the gingivae has been suggested which says that there is an increase in the proliferation of gingival fibroblasts or increased collagen synthesis rather than decreased levels of collagenase activity may be involved [5]. It was reported that HGF is characterized by excess accumulation of extracellular matrix (ECM) and fibroblasts cause remodeling of ECM, which causes disturbed collagen turnover or change in fibroblast proliferation resulting in gingival overgrowth. Likewise, oral keratinocytes modulate ECM protein expression and activity of fibroblasts; whereas keloid keratinocytes promote proliferation and production of collagen of underlying fibroblasts and inhibit apoptosis indicating the role of epithelium-connective tissue in diseased condition. This suggests that epithelium in HGF plays a part in pathogenesis of gingival overgrowth [6].Integrins are heterodimeric membrane glycoprotiens involved in cellular processes like cell-ECM and cell-cell interactions. The gene expression of collagen and MMP-1 is regulated by α1β1 and α2β2 where α1β1 reduces the expression of collagen while α2β2 stimulates collagen and collagenase gene expression in both two and three dimensional cultures. Although, excess ECM accumulates in HGF, it is reported that these integrins play important role for this change to occur. Heat shock protein (Hsp) 47 which is the major collagen binding heat inducible glycoprotein in fibroblasts found to be involved in several fibrotic diseases such as connective tissue diseases and dermal fibrotic diseases. Its expression is found in basal and suprabasal layers of HGF epithelium [7].As stated non-syndromic forms of HGF are transmitted as autosomal dominant traits and gene locus is present on chromosome 2p. Based on FISH analysis it was found that there are 2 gene loci on the short arm of chromosome 2 located in 2p21-2p22 and 2p13-p16 [8]. It is found that the patient with HGF shows the sign of failure of eruption of permanent molars which is consistent with our case also as the permanent molars in our case failed to erupt. Maxillary molars impaction can be due to abnormal osteofibrosis of alveolar bone while impaction of mandibular molars implies abnormal development of dental germ near to lower margin of mandible [9].The most characteristic feature of HGF is gingival enlargement of both maxillary and mandibular gingiva. In case of maxilla the enlargement can be due to both osteofibrosis and fibromatosis while in the mandible there is only fibromatosis without the mandibular bone affected which is seen in our case also [9]. Another feature is absence of involvement of periodontal ligament and the enlargement occurs peripheral to the alveolar bone within the attached gingiva [10] which is consistent with our case also as there is focal involvement of periodontal ligament at buccal area of molar only.The treatment modalities available for HGF include surgery, electrocautery and use of carbon dioxide laser. In the absence of carbon dioxide laser the most preferred method is conventional, external bevel gingivectomy, which should be done quadrant by quadrant with periodontal pack placement for 1week followed by 0.2% chlorhexidine oral rinse for 2 weeks [11]. Another treatment proposed for HGF includes radical surgery with the extraction of involved teeth which can be not convincing related to patient’s age and condition of teeth. To improve esthetics as well as treat periodontal disease the method of choice remains is undisplaced flap surgery [12, 13]. The classic treatment till today in developing countries is removal of excess gingival growth by scalpel but one should remember about the periodontal treatment which should be done before commencing the surgical part of the treatment plan [14]. It is reported that the patient of HGF undergoes repeated surgeries; therefore careful counseling of both parents and patient is of paramount importance. Education and motivation of patient should be properly done and is essential for maintenance of proper oral hygiene and regular recall visits [15].In the present case the method of treatment implied was surgery by scalpel method along with oral prophylaxis. The patient was counseled for repeated follow ups every month but it turned for 4 months only without any post operative complications and recurrence.
4. Conclusions
- The present case was of hereditary gingival hyperplasia (HGF). Patients with this condition require great care and motivation. It should be remembered that even correctly performed gingivectomy may not prevent from recurrent illnesses. To lower the risk of recurrence, eliminating the irritant, correct dental hygiene and regular cleaning along with frequent controlled visits should be performed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML