-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2014; 3(1): 1-3
doi:10.5923/j.cp.20140301.01
Necrotizing Sialometaplasia of Hard Palate - A Case Report
Ambrish Kaushal1, Ninad Moon2, Vikas Kumar3
1Associate Professor, Chandra Dental College & Hospital, Lucknow, Uttar Pradesh, India
2Professor, RKDF Dental College & Research Centre, Bhopal, Madhya Pradesh, India
3Senior Lecturer, Chandra Dental College & Hospital, Lucknow, Uttar Pradesh, India
Correspondence to: Ambrish Kaushal, Associate Professor, Chandra Dental College & Hospital, Lucknow, Uttar Pradesh, India.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Necrotizing Sialometaplasia (NSM) is an uncommon inflammatory condition that affects salivary glands. It appears as an aggressive looking lesion in an adult possibly resembling squamous cell carcinoma and mucoepidermoid carcinoma. Here we report a case of necrotizing sialometaplasia in a female on left side of hard palate mimicking carcinoma. A correct diagnosis to avoid mutilant surgical treatments is essential, considering that it is a self limiting disease.
Keywords: Necrotizing sialometaplasia, Inflammatory gland disease, Hard palate
Cite this paper: Ambrish Kaushal, Ninad Moon, Vikas Kumar, Necrotizing Sialometaplasia of Hard Palate - A Case Report, Clinical Practice, Vol. 3 No. 1, 2014, pp. 1-3. doi: 10.5923/j.cp.20140301.01.
1. Introduction
- Necrotizing Sialometaplasia (NSM) is a benign, self healing lesion of salivary glands which can arise in any area containing salivary glands. It mainly involves the mucoserous glands of the hard palate, but other reported sites include nasal cavity, trachea, parotid gland, sublingual gland, submandibular gland, larynx, buccal mucosa, maxillary sinus, tongue, tonsil and retromolar trigone[1]. It is a rare inflammatory disease of minor salivary glands first described by Abrams et al in 1973[2] while its histopathological characterstics described by Brannon were predominance of coagulative necrosis of acini in early lesions and squamous metaplasia, reactive fibrosis in later lesions. Anneroth, Hansen and Imbrey Edwards described five histological stages of NSM: infarction (necrosis), sequestration, ulceration, repair and healing[3]. It requires a great knowledge as it mimics with malignant neoplasms on clinical and histological examination like squamous cell carcinoma and mucoepidermoid carcinoma. We report such a case of necrotizing sialometaplasia in a patient without ulceration in hard palate.
2. Case Report
- A female patient aged 40 years came to the department of oral & maxillofacial surgery with the chief complaint of swelling in the left side of palate since 2 months (Figure 1). She reported about the extraction of 26 which she underwent four months back and after which the swelling started and slowly grown in size. On intraoral examination there was a presence of swelling on the left side extending from distal side of 24 to 28 region till mid palatine raphe. On palpation the swelling was soft in nature and tender and the overlying mucosa was of same color as the adjacent mucosa. An excisional biopsy under local anaethesia has been performed and the tissue has been sent for pathological examination (Figure 2 & 3).
 | Figure 1. showing swelling of palate (arrow) |
 | Figure 2. injecting local anaesthesia in swelling |
 | Figure 3. excisional biopsy of swelling done |
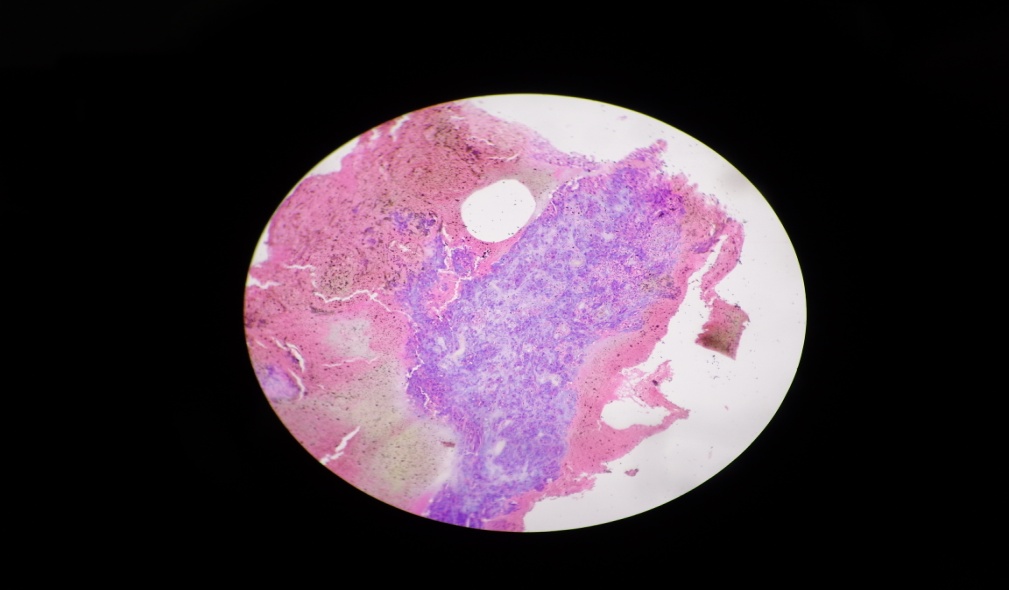 | Figure 4. (10X magnification)dense granulation tissue |
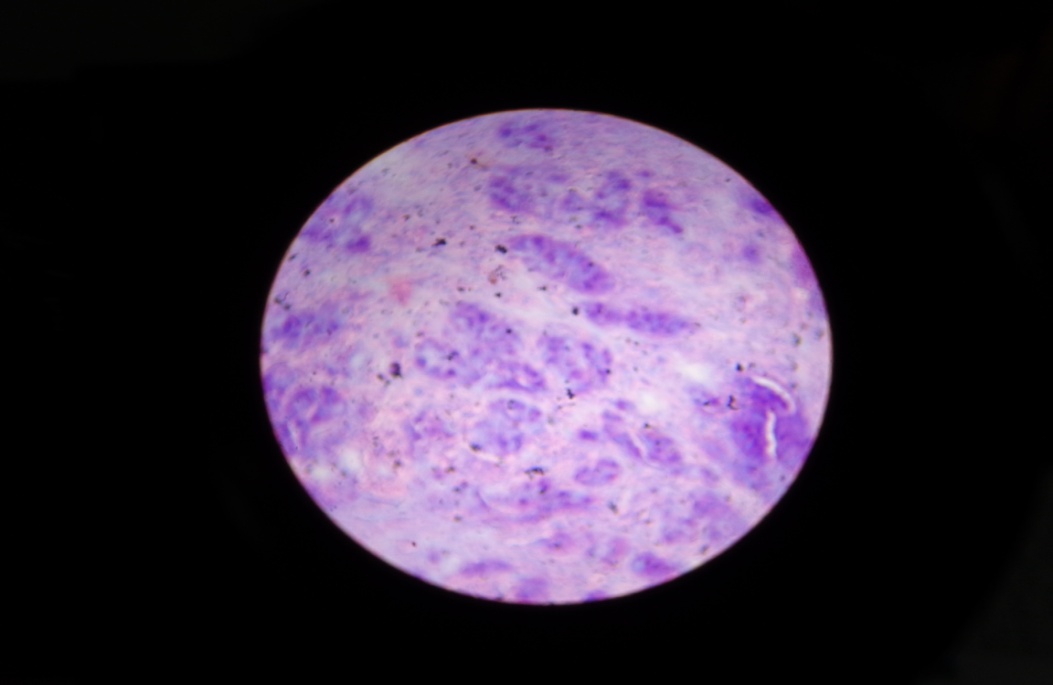 | Figure 5. (40X magnification) showing acinar necrosis |
3. Discussion
- Necrotizing sialometaplasia (NSM) is a benign self healing lesion of salivary glands with unknown exact etiology, but ischemia of local blood supply in the salivary gland lobules is most widely accepted theory. However, thrombotic vessel hypothesis adjacent to the lesion has thus far had only minimal microscopic support. Other causes of ischemia reported were local trauma, local anaesthesia, ill fitting dentures, smoking alcohol consumption, radiation, allergies, upper respiratory tract infection, intubation, surgical procedures, cocaine use and chronic vomiting [2,6,13]. Taking the causes reported into consideration the patient reported here underwent surgical extraction of tooth under local anesthesia.Intraorally NSM mainly involves junction of hard and soft palate presenting initially as a tender swelling. Subsequently the oral mucosa breaks up forming deep ulcer with a yellowish grey lobular base. Symptoms are generally disproportionately slight compared with size of the lesion. Most patients indicate mild complaints of tenderness or dull pain[5]. In our case the patient reported regarding tenderness and swelling but there was no ulcer formation.Anneroth et al assumed five stages of pathogenesis of necrotizing sialometaplasia i.e. infraction, sequestration, ulceration, repair and healing which can occur simultaneously in different areas, but the damage depends upon the healing capacity of the host tissues[4]. If the injury is extensive the sequestration of the necrotic tissues results in ulcer formation with dense inflammatory response[10], which is not observed in our patient. The histopathological features most helpful in the diagnosis are the ulcerated mucosa, pseudoepitheliomatous hyperplasia of epithelium, acinar necrosis, squamous metaplasia, preservation of lobular architecture, mucin pooling and granulation tissue formation[7,8]. The histopathological features in our given biopsy specimen are same accept the presence of ulcerative mucosal epithelium.Necrotizing sialometaplasia resolves spontaneously and usually no tteatment is required as the prognosis is excellent and spontaneous resolution usually occurs within weeks[9]. There was no untoward complication reported in our case also. If the histopathological diagnosis reports benign the treatment concludes and the patient is followed up and even a full thickness palatal lesion communicating with nasal cavity resolves completely in six months[14] which is done in our case but if malignant additional treatment is required[11,12].
4. Conclusions
- Necrotizing sialometaplasia is a benign self limiting disorder of salivary glands. It is misdiagnosed clinically and microscopically as a malignant neoplasm causing inappropriate treatment outcomes. Since it is a self limiting disease process therefore it requires no tteatment. To conclude clinicians and pathologists should be aware of this lesion as to avoid errors in th diagnosis and treatment of this benign pathologic condition.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML