-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
2012; 1(1): 1-3
doi: 10.5923/j.cp.20120101.01
Delayed BCG Granulomatous Reaction in An Immunocompetent Adult: A Case Report
Abraham A Ayantunde
Department of Surgery, Queen Mary Hospital, Frognal Avenue, Sidcup, DA14 6LT, United Kingdom
Correspondence to: Abraham A Ayantunde , Department of Surgery, Queen Mary Hospital, Frognal Avenue, Sidcup, DA14 6LT, United Kingdom.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
BacillusCalmette-Guerin (BCG) vaccine, a live attenuated strain of Mycobacterium bovis was developed in 1908 and it was first used in 1921. Its safety profile is widely accepted globally, with just a few side effects including cutaneous inflammatory papules and granulomas which are common within the first few weeks after vaccination. A few reports of delayed BCG granulomas many years following vaccination exist. A case of delayed BCG granulomatous reaction in an immunocompetent 29 year old female patient is herein described.
Keywords: BacillusCalmette-Guerin, Acid fast bacilli, Tuberculosis, Vaccination, Granuloma
1. Introduction
- BacillusCalmette-Guerin(BCG) vaccine, a live attenuated strain of Mycobacterium bovis was developed in 1908 and it was first used in 1921[1]. BCG vaccination has been used worldwide in an effort to control more serious infection by Mycobacterium tuberculosis. Intradermal or subcutaneous administration is performed, although the former is the preferred method. Immunisation with BCG is generally considered to be very safe with few side effects. There have been various reports of complications arising from BCG immunisation, including cutaneous manifestations[2].A case of 29 year old immunocompetent female with delayed BCG granulomatous reaction presenting years after immunisation is described.
2. Case Presentation
- A 29 year Caucasian female was referred by her family doctor to the surgical outpatient department presenting with recurrent swelling and redness over her BCG scar in the right deltoid region over a few months duration. She noticed that the swelling comes up and enlarges when she is stressed and regresses when she ‘feels alright’. She did not have associated pruritus of the swelling. There was no associated history of fever, chest symptoms, cough, night sweats or nodules in any other parts of the body. Her appetite and weight were entirely stable. There was no history of recent travel abroad or any tuberculosis (TB) contact. She did not have any history suggestive of immunodeficiency.She appeared clinically well with no lymphadenopathy or clubbing. She had no systemic signs of note. Examination of the right deltoid region revealed a 1cm by 1cm firm nodule over a scar consistent with previous BCG immunization. The nodule was non tender and not warmer than the surrounding area (figure 1). All blood tests including full blood count (FBC), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were within normal limits. Her chest radiograph was also normal (figure 2). An ultrasound scan of the right deltoid lump showed a well-defined, discrete, soft tissue mass measuring approximately 1.3cm by 0.7cm (figure 3). Fine needle aspiration cytology (FNC) showed that the nodule was largely formed by necrotic cellular debris with clusters of spindle cell and epitheloidhistiocytic granulomata. The cytomorphological appearance was suggestive of histiocytic granulomata reactions (figure 4). Ziehl- Neelsen staining for acid fast bacilli (AFB) of the tissue was negative. Routine bacterial culture was also negative. We did not proceed to polymerase chain reaction (PCR) in this patient because she had no risk factors for the development of tuberculous infection or immune suppression.She was followed up in conjunction with the chest specialists and it was concluded that this lesion was not cutaneous TB having considered the clinicopathological features. There were no clinical, laboratory or chest radiograph features suggestive of tuberculosis. The nodule subsequently resolved after a follow up period of eight months without any active treatment.
3. Discussion
- BCG granuloma is a rare complication of BCG vaccination. Cutaneous response to BCG immunisation is usually an inflammatory papule infiltrated by cellular infiltrates developing within four weeks of vaccination. This then develops into an ulcer healing within three months of onset to leave a small flat scar, a life-long evidence of immunisation against TB. There are various local cutaneous reactions and complications of BCG vaccination or therapy including erythema, ulceration from tissue necrosis, abscess formation, blistering, psoriatic reaction, and keloid formation[3-9]. Cutaneous TB infections are distinct entities from the cutaneous reactions to BCG vaccination. True cutaneous TB such as tuberculous chancre, tuberculosis verrucosa cutis, lupus vulgaris, scrofuloderma, orificial tuberculosis, military tuberculosis, metastatic tuberculous abscess and papulonecrotictuberculids are usually diagnosed by positive AFB staining, culture and confirmation by PCR. Most of these cases are usually cutaneous manifestations of systemic TB[10,11].Granulomatous reaction at the BCG vaccination site is uncommon years after immunisation and few of such cases have been reported[4,6-8]. The patient described herein developed cutaneous granuloma at the site of BCG scar after 29 years following vaccination. To the best of my knowledge, only one case of cutaneous granuloma has been reported, developing 50 years after BCG vaccination[7]. We did not proceed to PCR in this patient because she had no other risk factors for the development of tuberculous infection or immunosuppression. The granulomatous reactions at the BCG scar site may have been due to stressful conditions. Gasior-Chrzan[4] hypothesized that the granulomatous reaction was due to a protein in the BCG vaccine itself as stains, culture and PCR studies were all negative. Granulomatous reactions have also been reported in patients treated with BCG immunotherapy for urinary bladder cancer and malignant melanoma[9,12-14]. The natural history of BCG associated granuloma is not yet clearly defined. However, the majority have been reported to undergo spontaneous resolution. Caseating granulomas after BCG vaccination or after instillation for treatment of bladder cancer is that of healing naturally[12,14]. These lesions in the absence of AFB staining, negative culture or PCR may not require antituberculous treatment. However, treatment is required in patients with underlying immunodeficiency and those with extensive granulomatous reactions at the BCG vaccination site. A wide variety of treatment options exist including curettage and cauterisation of the ulcer, trial with clarithromycin and antituberculous agents[4,6]. Curettage of ulcerated nodule with the use of clarithromycin is recommended particularly if the nodule is associated with lymphadenopathy[2]. The use of anti- tuberculous agents is generally recommended for cutaneous complications of BCG vaccination especially in the immunocompromised individuals[2,4,6].This case is unique due to presentation many years after BCG vaccine immunisation. The patient was actively followed with complete resolution of the lesion by last clinic attendance eight months after the presentation. High index of suspicion is therefore required in the diagnosis of BGC granuloma as this particular finding may present several years following BCG vaccination in the absence of any identifiable risk factors for the development of tuberculous infection.
 | Figure 1. Cutaneous 1cm X 1cm lesion in the right deltoid region |
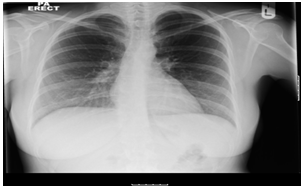 | Figure 2. Normal plain chest radiograph |
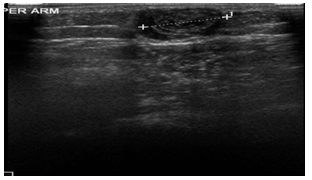 | Figure 3. Ultrasound scan of the right deltoid region lesion |
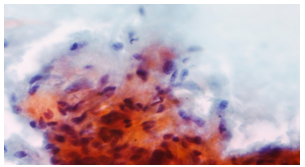 | Figure 4. Fine needle aspiration cytology showing histiocytic granulomatous reactions |
4. Conclusions
- It seems therefore that the delayed granulomatous reaction in this immunocompetent patient was most likely due to proteins in the BCG vaccine rather than true cutaneous tuberculosis. This patient was not offered any active therapy having considered all clinicopathological features together including the absence risk factor for tuberculosis infection. However, a careful and close monitoring until the granulomatous lesion is seen to have resolved is recommended in all cases.
ACKNOWLEDGEMENTS
- The author thanks Dr K Satkunam, Chest Physician and Dr Khan of the Department of Pathology of Queen Mary’s Hospital for their contributions.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML