-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Computer Science and Engineering
p-ISSN: 2163-1484 e-ISSN: 2163-1492
2021; 11(1): 1-8
doi:10.5923/j.computer.20211101.01
Received: Aug. 19, 2020; Accepted: Sep. 20, 2020; Published: Feb. 6, 2021

Use of Artificial Intelligence in Patient Experience in OP
Balagopal Ramdurai
Masters of Business Administration- ITM, Dubai, United Arab Emirates
Correspondence to: Balagopal Ramdurai, Masters of Business Administration- ITM, Dubai, United Arab Emirates.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In the current years, due to the significant developments in technologies in almost every domain, the standard of living has been improved. Emergence of latest innovations, advanced machinery and equipment especially in the healthcare domain, have simplified the diagonalizing process to a wide extent. Smart techniques employed in medical applications resolved the detection and rectification of various diseases. This work involves analysing how usage of Artificial intelligence practice can improve patient experience across the gamut of the healthcare industry primarily in the Out Patient (OP) Segment. As per industry statistics 88% of the patients are willing to shift the healthcare provider without hesitation. A 2018 study by The Beryl Institute found that 91 percent of patients think patient experience is extremely or very important, and it has an impact on the healthcare decisions they make.
Keywords: Artificial Intelligence, Patient Experience, Healthcare, Health tech, Out Patient, Predictive Analytics
Cite this paper: Balagopal Ramdurai, Use of Artificial Intelligence in Patient Experience in OP, Computer Science and Engineering, Vol. 11 No. 1, 2021, pp. 1-8. doi: 10.5923/j.computer.20211101.01.
Article Outline
1. Introduction
- In recent years, due to the rapid advancements in technologies, healthcare industry has witnessed lot of innovation to improve quality of patient care. With evolving technologies such as cloud computing, blockchain multiple use-cases have opened up new avenues for improving standards in health care sector. This document specifically works around improvement in Patient Experience with use of Artificial Intelligence techniques. How does one define patient experience- “The patient experience describes an individual's experience of illness/injury and how healthcare treats them. Increasing focus on patient experience is part of a move towards patient-centred care” & to simplify “ it begins with the front door and ends with the billing/payment clerk”. Therefore its imperative for health care providers to consider every touch points at every step of the care.According to (McCarthy, McGee, & O'Boyle and PricewaterhouseCoopers) Studies show that up to 65% of patient’s rate waiting times in clinics as unsatisfactory and 34% of patients said they would change their habits based on their experience. Five Key factors determining Patient Experience-As per the survey conducted across over 230 healthcare provider, top 5 things patients say to improve patient experience 1. 50% shorter wait-time2. 49% on advance knowledge of treatment costs3. 47% on not feeling rushed during appointments 4. 44% Providers with treating specific illness5. 41% easy to schedule appointments As healthcare organizations continue to focus on driving positive patient experiences, it’s changing the way chief information officers are looking at their jobs. No longer are CIOs simply looking at new ways to process and use data, but they are looking at how systems impact the patient & care Positive patient experiences need to go beyond strong patient-provider interactions and amenable facilities, although those factors are still important. Creating a positive patient experience must also include efficient care that connects patients with the right type of treatment, which requires providers to have the right kind of patient information.And CIOs are starting to recognize that.A 2018 survey from Impact Advisors and the Scottsdale Institute found that 80 percent of CIOs rank digital health and the patient experience as top healthcare priorities. And while much of that may include patient-facing tools such as wearable sensors or care management apps, CIOs are also putting a lot of weight on provider-facing data and processes that help them do their jobs better.And this is pushing more healthcare organizations to implement cutting edge technologies such as artificial intelligence (AI) and machine learning.
2. Artificial Intelligence in Healthcare
- As per Wikipedia, definition of AI in healthcare is defined as- Artificial intelligence in healthcare is the use of complex algorithms and software in other words artificial intelligence (AI) to emulate human cognition in the analysis, interpretation, and comprehension of complicated medical and healthcare data.The global artificial intelligence software market is forecast to experience massive growth in the coming years, with revenues increasing from around ten billion U.S. dollars in 2018 to an expected 126 billion by 2025.With Artificial Intelligence becoming part of mainstream application development, the functionality of the application is enhanced rapidly. The AI powered application becomes more outcome driven with tangible actionable abilities empowering CIO’s with datasets for better decision making abilities.With combining the power of data and machine learning enables healthcare providers to deploy software application which would improve patient experience and eventually the top line growth & bottom-line margins for the provider.The idea behind the success of AI in the medical field is due to the following reasons. First, AI can use sophisticated algorithms that are being used to learn various features from a large volume of healthcare data same as it being used in software engineering for various uses cases [1]. Artificial Intelligence (AI), has been playing a vital and growing role in the world in the past few decades. In fact, many people do not realize the form in which artificial intelligence can present itself in their daily life. When logging into email accounts, shopping using online platforms, requesting for car riding services, etc., all these uses artificial intelligence algorithms to improve user experience. But the most important field where AI is growing rapidly in the medical field, especially in treatment management and diagnostic [2].There has been profound impact on use of technologies combined with Artificial intelligence in the field of Telemedicine, which has helped reducing fatality of stroke patients [3].
3. Key Factors
- Certain key factors which deeply impacts the patient experience in Out Patient (OP) more than any-Wait time - most of the patients surveyed have pointed out longer wait-time usually creates low patient satisfaction level. Therefore reducing wait time becomes imperative. Wait-time across service locations- include patient waiting in the welcome desk to vitals to doctor consulting to pharma to lab to radiology and finally to billing /payment.Ease of appointment- Patient’s frustration grows with endlessly waiting/ hold over IVR (interactive voice response) and finally get to know about appointments few days away and no way to move up the slot if the appointment slot becomes free. Therefore ease of appointment booking is one of the key elements to improvements in patient experience.Ease of check-ins- The process of intimating the facility that the patient has arrived becomes crucial aspect to the experience, the ease with which patient checks-in at KIOSKS or at the welcome desk. The check-in process includes patient entering her identifier such as mobile number/ national id/ provider id and looking up the appointment & finally taking a token to get into the queue for availing services.Priority Patients- It’s important that provider recognize the aspect of patients with special needs or certain criteria such as senior citizen, pregnant women to get priority over others/normal patient. Ability to offer such priority care is crucial to patient experience.Care-time- Patients do not like to be rushed out of the care given by provider/doctor. There is a compelling need for comprehensive care with optimal time spent & not be rushed to consult next patient. This has direct impact on the wait-time experienced by the next patient.Navigation- One of the key elements which most facilities ignore, if the facility is quite vast & largely spread, most often patients gets lost & therefore its important to provide them with proper navigation to service delivery location.
4. Application of Artificial Intelligence
- The typical process followed in patient journey is getting through appointment, to visiting the clinic/ facility to check-in to validation of insurance to vitals and then dr. consultation and/or visit to pharmacy and availing services at laboratory or radiology.The way it its normally routed is through a queue management system. Many of the healthcare providers operate the inflow of patients over queue management solution. The combination of data procured from queue management and EMR can be of great use to improve patient experience. The dataset obtained from Queue management, EMR, pharmacy system, lab & other system such as wait-time in service delivery location/overall, care-time, transit-time between service delivery location and journey-time is used to derive a pattern & when applied with Artificial Intelligence Algorithms, unlocks datasets which can have profound positive impact on improvement of patient experience.Predictive modeling is healthcare is a proactive step towards identifying patients at risk of disease or adverse outcomes. One of the most common AI predictive model is the patient inflow into emergency department; re-admissions into emergency departments; disease or other outcomes; and in-patient mortality [5].a. Predictive Wait-time- which gives patients before hand the time they need to wait before availing a service which may help them to recalibrate their visit to the facility.b. Predictive wait-time can be calculated by the pattern analysis of care-time for the patient in a particular service including consulting, pharmacy, lab to name a few. Combining the cumulative wait-time, care-time at different service rendering point and with specific seasonal dataset predictive times can be achieved.c. Different dataset can run in parallel which can improve the accuracy of predictive wait-time, which includes specific doctor , specific nurse, based on over all service data, specific clerk working on the welcome desk, specific pharmacy based on pharmacist. The dataset could include seasonal variation including day of the week with combination of specific season including pre and post vacation season, holiday season, flu season, just after school re-opening.When these varied dataset are used, predictive wait-time becomes more meaningful. Which translates directly to appointments.Prediction of patient flow will help facility in optimizing hospital resources, improving operational planning, and, improving healthcare quality, planning and allocating hospital resources, increasing patient satisfaction [6,7].AI in predicting patient flowArtificial intelligence can be used to forecasting patient flow and avoid unnecessary trips to the emergency department. Rapid interpretation of clinical data would enable to segregate patients and predict outcomes in the emergency department operations. Consequently, AI directly influences the cost; efficient utilization of resources, cost and time; and quality of patient care [9]. At the time of arrival to the emergency, AI can stratify patients according to the risk and therefore facilitates efficient allocation of resources, which in turn improved patient outcomes. In the emergency department, AI can make a common diagnosis based on the radiographs and thereby accelerate the plan in patient care. At discharge, the AI can predict the possible outcomes, especially adverse events and provide a customized follow-up plan for the patient [9].Intelligent patient flow management system: Artificial Intelligence is applied in patient flow management to predict patient flow or efficiently manage patients in the healthcare facility. The key objectives of AI in the management of patient flow are [8,9]:• To forecast emergency department visits• To avoid unnecessary calls and visits to the health center• To customize a treatment plan• To render patient flow management more efficientA pilot study in Finland evaluated the impact of an Intelligent Patient Flow Management System (IFPM) in streamlining patient flow to hospital. The web-based system operation was based on the preliminary health issue information and symptom checking with intelligent medical diagnostics engine utilizing AI and machine learning algorithms. The primary objective of IPFM was to help patients avoid unnecessary calls and visits to their health center, and efficiently improve treatment planning and manage patient flow. The IPFM had a significant impact on healthcare cost. It was associated with a mean reduction of EUR 552,000 towards the total average service costs for 17,943 patients. A single unit cost reduction of EUR 31 translated into cost reduction towards one emergency department nurse visit (EUR 34); three emergency department nurse phone calls (EUR 10); nearly three primary care nurse phone calls (EUR 12); two primary care nurse letters or electronic contacts; one emergency department doctor consultation (EUR 35); more than one emergency department doctor phone call (EUR 23); more than one primary care doctor phone call (EUR 26); and one primary care doctor letter or electronic contact. The researchers concluded that an IPFM may reduce service costs in primary care setting [8].Patient flow prediction modelsPrediction of patient flow will help in optimizing hospital resources, improving operational planning, and, improving healthcare quality, planning and allocating hospital resources, increasing patient satisfaction [6,7]. Various forecasting methods that have been employed in predicting patient flow include linear regression, SARIMA, exponential smoothing, time series regression, and artificial neural network [9]. A few studies have attempted to predict patient flow to the emergency department or the outpatient using AI.Knowing the fluctuation in the volume of patient arrival in advance will help in taking off the stress of healthcare personals. Jiang et al., used a GA-based feature selection to compare the outcome with standard traditional forecast models (GLM, Auto Regressive Integrated Moving Average [ARIMA], and classical shallow artificial neural network [ANN]). However, these models work well when the prediction is based on one-week historical daily patient arrival data. The accuracy of prediction of these model declines if the prediction horizon is more than one week and hence fail to meet the demand for long-term decision making. In this context, Jiang et al., used a deep learning framework (Deep Neural Networks [DNN]) to predict the daily and hourly arrival volume of.AI for improving operational efficiencyResource optimization and patient crowding in the emergency department is a challenging issue. Resource requirement forecasting is essential to reduce the rising healthcare cost by optimizing the use and availability of healthcare resources. Yousefi et al., utilized machine learning and the genetic algorithm (GA) to determine optimal resource allocation in emergency departments. Yousefi et al., constructed a meta-model, with three power machine learning approaches (adaptive neuro-fuzzy inference system, feed forward neural network and recurrent neural network) using the bootstrap aggregating (bagging) and adaptive boosting (AdaBoost) ensemble algorithm. When applied to an emergency department, the GA algorithm was able to reduce the average length of stay by 15% [11].Predicting the waiting time and appointment delays can help in optimizing hospital resources and increasing patient satisfaction. Curtis et al., utilized several machine learning algorithms to predict waiting times at a walk-in radiology centers or delay times at scheduled radiology facilities across all four modalities (computed tomography, MRI, ultrasound, and radiography). Several variables were extracted from the radiology information system. Nine machine learning algorithms (neural network, random forest, support vector machine (SVM), elastic net, multivariate adaptive regression splines, k- th nearest neighbor, gradient boosting machine, bagging, and classification and regression tree) were used to fine-tune their parameters into the best possible training data fit. The root mean square error metric was used to determine the predictive accuracy of the algorithms. Among the nine machine learning algorithms, the elastic net was found to be better than other algorithms in accurately and efficiently predict the waiting time and delay time [12].Automated diagnostic decision support applications can fast track diagnostic decisions in the emergency department as well as within the hospital departments and wards [13]. Feature-rich AI models with several predictor variables were found to recognize patients at risk of experiencing an unplanned intensive care unit transfer [10]. Artificial intelligence algorithms are capable of predicting hospital readmissions within a specified duration of time and that indeed can reduce the cost in the health care system [8].patients under different severities with a prediction horizon of 28 days. The researchers accessed 245,377 patient records from 1st July 2009 to 31st March 2011 and obtained the daily and hourly volume. The data from 1st July 2009 to 22nd October 2010 were used for feature selection and hyper-parameter validation (around 70%) and the rest (from 23rd October 2010 to 31st March 2011) for performance testing. Based on the hospital triage system, patients were divided into five categories. Compared with other widely used prediction models, DNN-I (integrated)-GA achieved the highest accuracy with the lowest variance, which reflects its high-robustness [6]. The GA-based feature selection algorithm was improved by incorporating a fitness-based crossover. The improved GA-based feature selection algorithm outperformed a typical GA and four state- of-the-art feature selection algorithms (selection algorithm with minimal-redundancy-maximal-relevance framework, a simulated annealing-based wrapper feature selection algorithm, a variable importance-based feature ranking algorithm, a correlation-based feature ranking algorithm). The proposed integrated DNN-I-GA framework achieved higher prediction accuracy on the root mean square error and mean absolute percentage error metrics compared to the standard statistical models (GLM, seasonal-ARIMA, Auto Regressive Moving Average (ARIMAX), and ANN) and modern machine models (decision making SVM with radial basis functions (RBF) kernel [SVM-RBF], support vector machine with linear kernel [SVM-linear], random forest, relaxed LASSO [R-LASSO]) [6].
5. Dataset & Algorithm
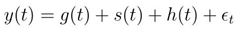
- Artificial Intelligence algorithms are usually trained on a large volume of data that is generated from health activities such as treatment assignment, diagnosis, etc. Learning from a large dataset will enable the algorithm to learn similar groups of objects and association between subject features and outcomes of the interest. Therefore a medical dataset will contain different kinds of information such as medical notes, physical examinations, images and clinical laboratory, recordings from medical devices, and demographics. In the diagnostic stage, AI algorithms require to analyse a substantial portion of data from diagnostic imaging and genetic testing. For example, researchers Topol and Jha advised radiologists to adopt AI technologies in order to analyse diagnostic images that contain large information data effectively. [1]Multiple algorithms are used and deployed under varied circumstances to get better accuracy, the types of algorithms used are regression and time series, and the study has found time series based gives better accuracy in terms of predicting certain data.Data sets used are- number of patients in flow/appointments, check-ins, no-show, walk-ins and in-terms of facility wait-time, care time, serve time, transit times and journey time along with the seasonal / peripheral data sets.What is time series forecast method-Time series forecasting is an important area of machine learning and It is important because there are so many prediction problems that involve a time component.Time series forecasting is the use of a model to predict future values based on previously observed values.When it comes to predicting absolute numbers with respect to patient, wait-time, time series forecasting proves edge over others. Time does play a important role in normal machine learning datasets.A time series dataset is different.Components of Time SeriesTime series analysis provides a body of techniques to better understand a dataset.Perhaps the most useful of these is the decomposition of a time series into 4 constituent parts:1. Level. The baseline value for the series if it were a straight line.2. Trend. The optional and often linear increasing or decreasing behavior of the series over time.3. Seasonality. The optional repeating patterns or cycles of behavior over time.4. Noise. The optional variability in the observations that cannot be explained by the model.Some the classical time series forecasting methods-1. Autoregression (AR)2. Moving Average (MA)3. Autoregressive Moving Average (ARMA)4. Autoregressive Integrated Moving Average (ARIMA)5. Seasonal Autoregressive Integrated Moving-Average (SARIMA)The latest one in the list is Prophet- Prophet is an open source library published by Facebook that is based on decomposable (trend+seasonality+holidays) models. It provides with the ability to make time series predictions with good accuracy using simple intuitive parameters and has support for including impact of custom seasonality and holidays!What’s new in Prophet?When a forecasting model doesn’t run as planned, we want to be able to tune the parameters of the method with regards to the specific problem at hand. Tuning these methods requires a thorough understanding of how the underlying time series models work. The first input parameters to automated ARIMA, for instance, are the maximum orders of the differencing, the auto-regressive components, and the moving average components. We use a decomposable time series model with three main model components: trend, seasonality, and holidays. They are combined in the following equation:• g(t): piecewise linear or logistic growth curve for modelling non-periodic changes in time series• s(t): periodic changes (e.g. weekly/yearly seasonality)• h(t): effects of holidays (user provided) with irregular schedules• εt: error term accounts for any unusual changes not accommodated by the model
6. Benefits to Providers
- While providers deploy Artificial intelligent based more patient focused care based solution, it offers an unique proposition for healthcare providers. With the dataset obtained on care-time, wait-time and serve-time, the ability of providers to gauge the productivity/ service level becomes high. With the set of data for specific nurse providers may be able to find out number of available hours for nurse against a service she is rendering. Similarly for doctors, how much care time he/she is giving on specific day/date and for specific services. Imagine a physical room being used for a service which see less number of patient against the available occupancy versus a service which see heavier inflow of patients, using the application provider can re-assign rooms based on the load it can take. Therefore, implementing of Artificial Intelligence based application will offer providers to focus on patient care improvement more holistically & offer immense benefits towards patient experience and same time streamline operational efficiency for th facilities.
7. Review of Existing Study
- Bate P, Robert G et al., (2006) Involving patients in service improvement and listening and responding to what they say has played a key part in the redesign of healthcare processes over the past five years and more. Patients and users have attended stakeholder events, participated in discovery interviews, completed surveys, mapped healthcare processes and even designed new hospitals with healthcare staff. However, to date efforts have not necessarily focused on the patient’s experience, beyond asking what was good and what was not. Questions were not asked to find out details of what the experience was or should be like (“experience” being different from “attitudes”) and the information then systematically used to co-design services with patients. Knowledge of the experience, held only by the patient, is unique and precious. In this paper, attention is drawn to the burgeoning discipline of the design sciences and experience-based design, in which the traditional view of the user as a passive recipient of a product or service has begun to give way to the new view of users as integral to the improvement and innovation process.Ansell, D., Crispo, J.A.G., Simard, B. et al. (2017) Accessibility and availability are important characteristics of efficient and effective primary healthcare systems. Currently, timely access to a family physician is a concern in Canada. Adverse outcomes are associated with longer wait-time for primary care appointments and often leave individuals to rely on urgent care. When wait-time for appointments are too long patients may experience worse health outcomes and are often left to use emergency department resources. The primary objective of our study was to systematically review the literature to identify interventions designed to reduce wait-time for primary care appointments. Secondary objectives were to assess patient satisfaction and reduction of no-show rates.Li, Wenhao and Sun, Zhankun and Hong, L. Jeff, et. al., (2020) Upon arrival at emergency departments (EDs), patients are classified into different triage levels indicating their urgency. Using data from an urban hospital in Canada, we find that within the same triage level, the average waiting time (time from triage to physician initial assessment) of discharge patients is shorter than that of admit patients for middle-to-low acuity patients, suggesting that the order of patients being served deviates from FCFS (first-come-first-served), and to certain extent, discharge patients are prioritized over admit patients. This observation is intriguing as among patients of the same triage level, admit patients - who need further care in the hospital - should be deemed no less urgent than discharge patients who only need treatment at the ED.Benjamin Harry Ziskind, Joshua David Bass, Scott Sebastian Sahadi, Benjamin Keeling Mathews et al (2016) An estimate is provided for how long a guest will have to wait to enter a ride, restaurant, restroom, or other point of interest at a venue. Wait-time are computed using one or more algorithms (e.g., Bayesian) that can combine direct measurements around the point of interest, historical measurements around the point of interest, and measurements taken from other systems not directly connected to the point of interest. Supporting systems will vary by venue and may include entry ticketing systems, network traffic, point of sale registers, event schedules, and proximity detectors in other parts of the venue. By comparing probabilities generated from this disparate data, current and future wait-time can be estimated and provided to front-end devices corresponding to guests or staff.Santibáñez, P., Chow, V.S., French, J. et al, (2009) Considers an ambulatory care unit (ACU) in a large cancer centre, where operational and resource utilization challenges led to overcrowding, excessive delays, and concerns regarding safety of critical patient care duties. Using simulation to analyze the simultaneous impact of operations, scheduling, and resource allocation on patient wait time, clinic overtime, and resource utilization. The impact of these factors has been studied before, but usually in isolation. Further, the model considers multiple clinics operating concurrently, and includes the extra burden of training residents and medical students during patient consults. Through scenario analyses found that the best outcomes were obtained when not one but multiple changes were implemented simultaneously. There developed configurations that achieve a reduction of up to 70% in patient wait-time and 25% in physical space requirements, with the same appointment volume. The key findings of the study are the importance of on time clinic start, the need for improved patient scheduling; and the potential improvements from allocating examination rooms flexibly and dynamically among individual clinics.Lewis, A.K., Harding, K.E., Snowdon, D.A. et al., (2018) review found low-level evidence suggesting an association between early access to community outpatient services and improvement of some patient outcomes. Specifically, shorter wait-time from referral to first visit for musculoskeletal pain services may improve patient work participation. Shorter wait-time for cardiac rehabilitation may improve patient exercise capacity. The effects of a short wait time for other patient conditions and patient outcomes, including quality of life, psychological symptoms and patient experience, are inconclusive. The modest benefits in health outcomes observed in reducing wait time for community outpatient services suggest that other possible benefits such as increasing patient flow should be explored.B. Nithya and V. Ilango, et al, huge data set like to perform predictive analysis or pattern recognition, machine learning is the way to go. Machine Learning (ML) is the fastest rising arena in computer science, and health informatics is of extreme challenge. The aim of Machine Learning is to develop algorithms which can learn and progress over time and can be used for predictions. Machine Learning practices are widely used in various fields and primarily health care industry has been benefitted a lot through machine learning prediction techniques. It offers a variety of alerting and risk management decision support tools, targeted at improving patients' safety and healthcare quality. With the need to reduce healthcare costs and the movement towards personalized healthcare, the healthcare industry faces challenges in the essential areas like, electronic record management, data integration, and computer aided diagnoses and disease predictions. Machine Learning offers a wide range of tools, techniques, and frameworks to address these challenges.
8. Conclusions
- To sum up “Patient experience starts at the entrance of the facility and ends with the checkout/billing clerk”.Patient experience has become an important corner stone for success for any facility. And recent study & survey shows growing number of investments towards enhancing the patient experience.Technologies combined with Artificial intelligence does show there is possibility of tangible outcome which does have increase in patient experience & satisfaction.Artificial Intelligence is definitely improving the healthcare industry. From predictive medical care and more accurate diagnosis to motivating the patients to take care of their health, AI will certainly continue enhancing the patient experience and healthcare expertise in general.Predictive algorithms to ascertain predictive wait-time will have profound impact on the patient experience and ascertaining care-time/serve-time will enhance the productivity of the personals serving and also pave way for optimizing the care loads for the facilities and manage the resources with optimal utilization.Artificial intelligence driven application seems to be an ideal tool for optimizing patient experience in hospitals & also provide the CIO’s with data insights to improve operational efficiency.With wide range of available AI algorithms its quite challenging for software manufacturers to single down to one. Software owners must be willing to adapt & evolve their algorithms and programs with the time. Despite available evidences on the benefits of deploying AI powered software application to streamline the patient flow management and boost operational efficiency, the application & approach is still in infancy. Further studies, research and working examples with large datasets are required for improving patient experience.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML