-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2024; 12(1): 6-10
doi:10.5923/j.cmd.20241201.02
Received: Jan. 16, 2024; Accepted: Feb. 6, 2024; Published: Feb. 29, 2024

Intradialysis Dynamics of the Activity of Free Radical Oxidation and the Antioxidant System
A. B. Daminov1, M. A. Sabirov2
1Tashkent Pediatric Medical Institute, Bogishamol, 223, Tashkent, Uzbekistan
2Republic Specialized Scientific-Practical Medical Center of Nephrology and Kidney Transplantation, Yunusabad District, Yangi Shahar 9, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

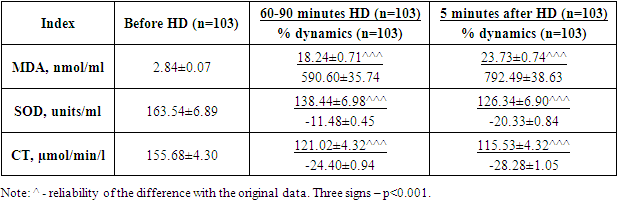
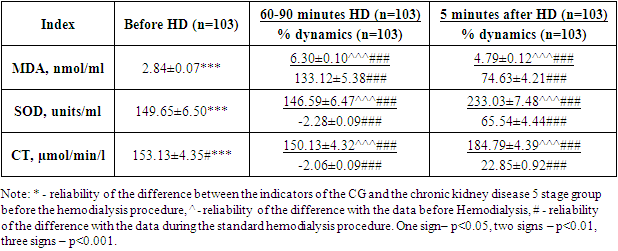
Hemodialysis by 60-90 minutes is associated with progressive activation of free radical oxidation (an increase in MDA concentration by 950.60% and a decrease in SOD activity by 11.48% and CT by 24.40%). Towards the end of HD, LPOactivation continues to progressively deteriorate. Intradialytic physical activity has a protective effect by limiting the activation of LPO, as well as promoting the activation of AOS.
Keywords: Hemodialysis, Free radical oxidation, Antioxidant system, Intradialytic physical activity
Cite this paper: A. B. Daminov, M. A. Sabirov, Intradialysis Dynamics of the Activity of Free Radical Oxidation and the Antioxidant System, Clinical Medicine and Diagnostics, Vol. 12 No. 1, 2024, pp. 6-10. doi: 10.5923/j.cmd.20241201.02.
Article Outline
1. Introduction
- Patients on program hemodialysis often develop haemorheological disorders. The mechanism of these disorders is complex and includes activation of platelets upon contact with the surface of the dialyzer membrane, vascular prostheses, circuit conductors [1,2], depletion of endothelial expression of the tissue thromboplastin inhibitor [3] and endothelial dysfunction, in which the expression of nitric oxide and prostacyclin by endothelial cells is impaired, plasminogen activator and thromboplastin [3,4,5]. Activation of von Wille-brandt factor on the platelet membrane during hemodialysis also contributes to the prothrombotic status of patients [6,7,8].In patients with chronic kidney disease stage 5, the concentration of homocysteine is increased [4,9], which is associated with both impaired renal clearance [10] and systemic changes in metabolic activity [11]. Also, metabolic changes in patients with chronic kidney disease stage 5 are characterized by hyperlipidemia and dyslipidemia [12].One of the key aspects of endothelial dysfunction in patients with chronic kidney disease stage 5 is the reduced bioavailability of nitric oxide [4]. The mechanisms of this phenomenon in this cohort of patients are not only the irreversible binding of the molecule by free hemoglobin, but also the inactivation of nitric oxide by free radicals that are formed during the activation of neutrophils during contact with the dialysis membrane [13] and the influence of homocysteine [14].A study [15] conducted during the dialysis procedure found that during dialysis in patients the concentration of malondialdehyde and the activity of superoxide dismutase increased, which reflects the activation of lipid peroxidation and antioxidant defense. The authors suggest that this reflects endothelial cell membrane damage and dysfunction, although the concentration of stable nitric oxide metabolites showed a nonsignificant increasing trend, which may be associated with increased macrophage nitrate synthase activity. In a Ukrainian study [16], on the contrary, a decrease in the concentration of stable nitric oxide metabolites was found, with regard to the concentration of malondialdehyde and the activity of superoxide dismutase and catalase, the result coincides with the Ryazan authors [15]. At the same time, the number of circulating endothelial cells did not change during hemodialysis, although the correlations between the concentration of malondialdehyde and the number of circulating endothelial cells were significantly positive.Therapeutic interventions to prevent intradialytic vascular dysfunction may include changes in the hemodialysis regimen - intensive nocturnal hemodialysis, changing the dialysate solution, the use of dialysate membranes with modified surface properties, but this approach is associated with financial and logistical difficulties, and in addition, does not yet have a sufficient evidence base. The use of drugs aimed at normalizing the functional state of the endothelium - levorotatory arginine - is controversial, since in patients with chronic kidney disease there is a systemic inflammatory reaction accompanied by activation of macrophage nitric oxide synthase, which calls into question the effectiveness of drugs that release nitric oxide [17]. Another group of drugs with proven endothelial effectiveness, statins, do not have a point of application in chronic kidney disease, since they are absorbers and not synthetics of cholesterol; in addition, in patients with chronic kidney disease, cholesterol has a cytostatic effect on inflammatory effectors [18].A possible treatment option could be dynamic physical activity (PE), which helps normalize the functional state of the endothelium [19]. Also, dynamic physical activity promotes the effective transition of extracellular fluid into the lumen of blood vessels and minimization of intradialytic hypotension [20,21]. The effect of physical activity on the functional state of the vascular wall in patients with chronic kidney disease requires a detailed study, including assessment of various mechanisms.Purpose of the study: To study the intradialytic dynamics of LPO and AOS activity against the background of standard hemodialysis and with the use of intradialytic physical activity.
2. Materials and Research Methods
- The present study included 103 patients with chronic kidney disease stage 5 and 20 age-matched healthy volunteers. All study participants signed informed consent and received explanations about the importance of physical activity in maintaining health and treatment tactics, as well as the complexity of the pathophysiological changes associated with the terminal stage of chronic kidney disease and chronic disease.All study participants underwent a laboratory and instrumental examination, including the LPO/AOS systems. The data obtained from the group of patients with chronic kidney disease 5 stage (103 people) were compared with the data obtained in the group of healthy volunteers (CG), 20 people).All patients with chronic kidney disease stage 5 included in the study were examined during 2 hemodialysis sessions, each after a 3-day break. The first session was carried out according to the standard method for the patient. Before the session (standard HD0), during the session at 60-90 minutes of hemodialysis (standard Hemodialysis 1) and after the end of hemodialysis (standard hemodialysis 2), patients underwent serial laboratory testing. The second hemodialysis session was carried out using intradialytic physical activity for 30minutes and 1hour of hemodialysis. Serial examinations were carried out according to the above-described scheme.During the study, the intradialytic dynamics of the studied pathophysiological changes were studied, and the dynamics were compared against the background of standard hemodialysis and hemodialysis with FN.The study included persons aged 18-70 years with chronic kidney disease stage 5 of various etiologies, who were aware of the essence of the disease, the effects and risks of using physical activity, and who agreed to participate in the study. The criteria for non-inclusion in the study were: the presence of pathology limiting physical performance or terminal organ failure, other than chronic kidney disease, malignant tumors, fever, acute period of infectious diseases or exacerbation of chronic diseases affecting performance and quality of life, incapacity of the patient or refusal of the patient to participate in the study.The majority of patients included in the study were in the age group of 40-49 years, slightly less often- 30-39 years. According to the etiology, in the majority of patients, chronic kidney disease developed due to chronic glomerulonephritis (36 people) and type 2 diabetes (33 people). According to hemodialysis experience, all patients were evenly represented in 3 categories: up to 6 months, 6-12 months and 12-24 months.Laboratory studies included hematological parameters. Blood was collected from the cubital vein using vacutainers with an appropriate anticoagulant. The studies were carried out on automatic analyzers - hematological and biochemical.Studies included:- concentration of malondialdehyde (MDA, nmol/ml), activity of superoxide dismutase (SOD, units/ml)) and catalase (CT, µmol/min/l) - biochemical analyzer after blood centrifugation and serum isolation.The intervention whose effectiveness was studied in this study was intradialytic exercise. For this purpose, a portable simulator was used, designed for pedaling with hands or feet in a sitting or lying position. The load was carried out for 30 minutes in the first hour from the start of hemodialysis. Most of the patients used foot pedaling with a resistance of 25 W and a pedaling speed of 60 rpm. In the case of muscle atrophy of the lower extremities, a low-intensity load was applied - without resistance and at a speed of 30 rpm. In the case of gangrene, amputation of the foot/part of the foot, trophic ulcers, severe painful form of peripheral neuropathy, manual pedaling without resistance was used at a speed of 60 rpm.All data obtained during this study were entered into summary tables in Excel for Windows 2007 and then sorted into groups in accordance with the purpose and objectives of the study. In the case of parametric data subject to a normal distribution, arithmetic means and their standard errors were calculated for the groups; intergroup comparisons were carried out using an unpaired Student's test. In the case of non-parametric characteristics, their frequency was determined and intergroup comparison was carried out using the chi-square table test and assessing its reliability using tables taking into account the number of degrees of freedom. The dynamics of indicators in groups was calculated as the average value of the relative dynamics of indicators for all participants in the group; the reliability of the dynamics was determined using a paired Student's test.
3. Research Results and Discussion
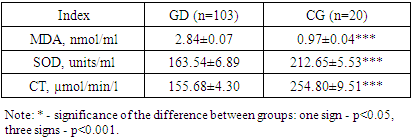
- During the study, 103 patients receiving program hemodialysis were examined before, during (during the 2nd hour of hemodialysis) and after the hemodialysis procedure, carried out after a 3-day break. The creatinine concentration in the main group of patients was 665.89±13.47 µmol/l vs 67.70±1.85 µmol/l in the CG (p<0.001) and did not differ depending on the age of the patients (670.69±20.04 µmol/ l, in patients under 41 years of age and 661.24±17.69 µmol/l, p>0.05) and the etiology of chronic kidney disease (668.55±28.37 µmol/l in patients with diabetes and 656.35±12.91 µmol/l in patients with non-diabetic etiology of chronic kidney disease, p>0.05).The study of the activity of LPO/AOS processes revealed a significant increase in the concentration of MDA and a decrease in the activity of SOD and CT in patients with chronic kidney disease 5 stage compared to the CG (p <0.001 significance of the difference in all three indicators from the CG). Also, in patients with chronic kidney disease 5 stage, an increase in the concentration of his CRP was found (p<0.001 significant difference from the CG), which indicates the activity of systemic inflammation in this cohort of individuals (Table 1).
|
|
|
4. Conclusions
- Hemodialysis by 60-90 minutes is associated with progressive activation of free radical oxidation (an increase in MDA concentration by 950.60% and a decrease in SOD activity by 11.48% and CT by 24.40%). Towards the end of hemodialysis, LPO activation continues to progressively deteriorate. Intradialytic physical activity has a protective effect by limiting the activation of LPO, as well as promoting the activation of AOS.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML