-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2021; 11(2): 15-19
doi:10.5923/j.cmd.20211102.01
Received: Jun. 24, 2021; Accepted: Jul. 14, 2021; Published: Jul. 30, 2021

Hypernatremia in Neonates Getting Exclusive Breastfeeding
Mohammad Basir Uddin 1, Md. Manajjir Ali 1, Md Rahimullah Miah 2, Shayma Siddique 3, Md Rubel Ahmed 4, Sirajum Munir Tanvir 4, Md. Abdul Hanif 4
1Department of Paediatrics, North East Medical College and Hospital, Sylhet, Bangladesh
2Department of IT in Health, North East Medical College, Sylhet, Bangladesh
3Department of Gynae and Obs, Parkview Medical College and Hospital, Sylhet, Bangladesh
4Neonatal Intensive Care Unit (NICU), North East Medical College Hospital, Sylhet, Bangladesh
Correspondence to: Mohammad Basir Uddin , Department of Paediatrics, North East Medical College and Hospital, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Neonatal hypernatremia and hypernatremic dehydration is a potentially fatal condition which adversely affects the central nervous system, leading to devastating consequences like intracranial hemorrhage, thrombosis and death. Hypernatremia previously thought to be unusual in exclusively breast-fed neonate but recently the incidence of hypernatremia and hypernatremic dehydration is rising. Hypernatremic dehydration is the most dangerous form of dehydration because of complications of hypernatremia itself and of its therapy. Clinical presentation is variable. Some present with lethargy; others are alert and hungry. This study emphasized the importance of early recognition and timely intervention of neonatal breast milk hypernatremia significantly reduces the consequences. Aim: Assessment hypernatremia and hypernatremic dehydration in neonate’s receiving exclusive breastfeeding. Methods: It was a retrospective study carried out in the Neonatal Intensive Care Unit (NICU) of North East Medical College Hospital (NEMCH), Sylhet, Bangladesh during the period of January 2018 to June 2019 who were investigated and found to have hypernatremia and whose mother’s breast milk sodium and serum sodium was also done. Neonate who on exclusively breast feed with serum sodium ≥ 150 mmol/l, normoglycemic, normocalcemic, no clinical and laboratory evidence of sepsis were included in this study. Results: Elevated breast milk sodium strongly interrelated with neonatal hypernatremia in exclusively breast-fed neonates. Conclusion: This study concludes the need for early recognition of hypernatremia and judicious fluid management is essential for better prognosis and highlighted the elevated breast milk sodium is an important etiological factor.
Keywords: Neonate, Hypernatremia, Hypernatremic dehydration, Exclusive breast feeding
Cite this paper: Mohammad Basir Uddin , Md. Manajjir Ali , Md Rahimullah Miah , Shayma Siddique , Md Rubel Ahmed , Sirajum Munir Tanvir , Md. Abdul Hanif , Hypernatremia in Neonates Getting Exclusive Breastfeeding, Clinical Medicine and Diagnostics, Vol. 11 No. 2, 2021, pp. 15-19. doi: 10.5923/j.cmd.20211102.01.
Article Outline
1. Introduction
- Human breast milk is undoubtedly the best source of nourishment for human infants [1]. The benefits of exclusive breastfeeding of a baby are well known. It reduces the incidence of many acute infections and chronic diseases and improved neurodevelopmental outcomes of the baby [2,3]. Hypernatremia assumed to be a rare complication of breast feeding [4]. Hypernatremia previously thought to be unusual in breast feed babies but recent reports suggested that the incidence of hypernatremia and hypernatremic dehydration is rising. The condition carries an acute morbidity and mortality [5]. Hypernatremia, a frequently encountered electrolytes disorder, define as a serum sodium level greater than 145 mmol/L. Serum sodium of >160mmol/L regarded as severe hypernatremia [6]. It is normal over the 1st week of life for the neonate to lose as much as 7% of its birth weight through normal dieresis. Weight loss >7% of birth weight is a cause for concern. In neonate, hypernatremic dehydration may be suspected as weight loss of more than 10% of birth weight at the end of first week of life [7]. Hypernatremic dehydration is a potentially lethal condition in neonate which adversely affects central nervous system, leading to devastating consequences like intracranial hemorrhage, thrombosis, and death [1]. Sodium content of breast milk at birth is high and declines rapidly over the subsequent days. In 1949, Macy established mean sodium content of colostrum in first 5 days is (22 ± 12) mmol/L and transitional milk from day 5 to day 10 is (13 ± 3) mmol/L and of mature milk after 15 days is (7 ± 2) mmol/L [8]. After the first few days of lactations, the breast milk sodium does not seem to show a significant diurnal change and does not appear to differ between either breast [9]. In Bangladesh works on this condition on neonate is very lacking. Our health personals may not fully accustom to this condition on newborn infant. But management can improve outcome of hypernatremic dehydration of exclusively breast feed neonate. This study aimed to orient our health care professionals, specially pediatricians, concerning some essential aspect of such important issue for early recognition and timely intervention of this condition so that devastating consequences in neonate can be avoided.
2. Materials and Methods
- Study Site and DesignAfter approval obtained from the institutional review board, this retrospective study conducted Neonatal Intensive Care Unit (NICU) of North East Medical College Hospital (NEMCH) Sylhet, Bangladesh during the period of January 2018 to June 2019, neonate who admitted with serum sodium concentrations of ≥150mmol/L and no explanation of hypernatremia other than inadequate milk intake. Sample sizeThe sample size was six. The observed patients were 4 males and 2 females, whose average age 10 days. Symptoms and signs of hypernatremia in neonates that we encountered various data were weight loss, lethargy, poor feeding, vomiting, irritability, reduce urine frequency. Exclusion and inclusion criteriaTerm exclusively breast feed neonates who found euglycemic, normocalcemic, sepsis screen negative, serum sodium ≥150mml/L and those mother’s breast milk sodium performed included in this study. Those mothers’ breast milk sodium could not perform; formula feeding baby, congenital anomalies and premature neonate excluded from the study.Data CompilationThe primary and secondary collected data compiled according to the research objectives.Data Analysis and InterpretationThe compiled data analyzed with update software for statistical analysis, like MS Excel 2019 and SPSS version 27. Then the analysis data interpreted for display as findings.
3. Results
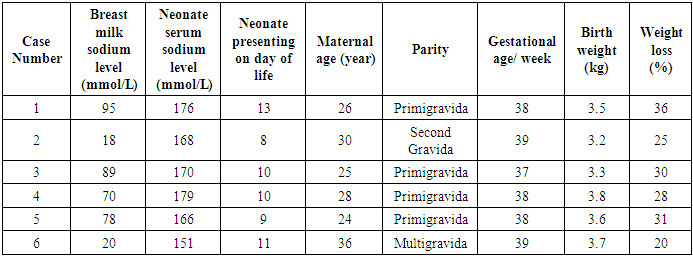
- A total 6 number of patients included in this study. Age range of patients at diagnosis was 8 days to 13 days. Mean age is being 10 days. Most of the mothers are primigravida and their mean age is 28 years. The main reasons for seeking medical attention were weight loss (100%), lethargy (61%), low urine output (50%), poor feeding (48%), vomiting (15%) and jaundice (10%). We performed a full sepsis evaluation including blood culture in all cases. We found none of the neonates to have bacteremia. Mean serum sodium at admission is 168 mmol/L and mean serum creatinine 1.2 mg/dL. Higher serum sodium concentration observed in four neonates born in primigravida mother. Their breastmilk sodium also significantly elevated.
|
|
|
4. Discussion
- Neonatal severe hypernatremic dehydration is a medical emergency with a high rate of morbidity and mortality. Diagnosis of neonatal hypernatremia often difficult and miss diagnosis as sepsis because clinical features in most cases resemble sepsis. Treatment of sepsis took as major management for this condition. Hypernatremia because of high breast milk sodium is an established entity [10]. The daily requirement of sodium 0.5 mEq/kg/day from birth to three months. Infants fed on mature human breast milk receive enough sodium to meet their needs for growth, dermal losses and urine losses [11]. The concentration of sodium in breast milk varies as the lactation period progresses and is independent of the mother's diet [12]. In 1949, Macy established mean sodium content of colostrum in first 5 days is (22 ± 12) mmol/L, transitional milk from day 5 to day 10 is (13 ± 3) mmol/L and of mature milk after 15 days is (7 ± 2) mmol/L [8] Various hypotheses like diminished breast milk production or delayed maturation of breast milk, have been put forward to explain the mechanism of elevated concentration of breast milk sodium. Sodium chloride and lactose concentrations combine reciprocally to maintain the milk's osmolality at a level similar to that of blood. Any fall in lactose concentration due to lactation failure could cause a rise in the sodium content of the milk [13]. Galactopoiesis failure could in turn be secondary to neonatal factors, such as primary suckling deficiency or poor suckling because of infection, or two maternal factors, such as stress, mastitis, or sore/retracted nipples. This can lead to a vicious circle in which when breast milk production reduced, the neonate becomes weak and sucks poorly and the drive for lactation drops further and dehydration occurs [1]. Therefore, variation in the normal physiology and maintaining high levels of sodium concentration in breast milk are closely associated with lactation failure [14]. Clinical presentation of hypernatremic dehydration usually are around ten days with the range from 3rd to 21st days of life consistent with the present study [6].Hypernatraemic dehydration can occur in the first-born or even in babies whose mothers have previously breastfed successfully [15]. The sodium load excreted by newborn infants is less than that excreted by older infants and children, so newborns are particularly sensitive to the effects of high serum sodium concentration. The relatively higher levels of insensible water loss per kilogram of body weight in infants, and less efficient conservation of water due to renal immaturity at this age, predisposes this group to dehydration. Thus, a high sodium intake in the presence of inadequate feeding can lead to hypernatremic dehydration in the newborn, as seen in the present study. The source of extra sodium in our patients was from high sodium in the breast milk [1].In this study, four out of six infants showed signs of severe dehydration, which was successfully treated as per protocol. Two babies did not show any sign of dehydration but were having hypernatremia biochemically. None had convulsion at the time of presentation. None of the babies were breast milk withheld. We monitored them while they continued breastfeeding. The level of sodium in the serum of babies and in the breastmilk returned to normal. Elevated breast milk sodium thus appears to be the etiological factor in these cases. Sodium content of breast milk at birth is high and declines rapidly over the subsequent days. Mortan (1994), studied the breast milk of 130 women as they breasted feed; women who failed to establish a good breast feeding did not show the normal decline in sodium content [16]. Hypernatremia associated with hyperglycemia and mild hypocalcaemia, the mechanism is unknown [17]. Our reported one case developed hypocalcemia and managed with intravenous calcium gluconate.While hypernatremia itself can cause seizure, seizures can itself occur during treatment, especially during fluid resuscitation. For this reason, hypernatremic dehydration should rehydrated slowly. Rapid correction of increased serum sodium concentration predisposes to osmotic changes in the brain which can exacerbate the existing cerebral edema. Hence, oral rehydration with expressed breast milk or direct breastfeed or a fluid rehydration at a rate of 100 ml/kg/day can be done [18]. Banister et al., reported on the IV (intravenous) treatment of 36 infants with hypernatremic dehydration, infants who were rehydrated at a rate of 150 ml per kg per 24 hours where they gave more likely to develop convulsions than those 100 ml per kg per 24 hours [19]. In our NICU, none of the hypernatremic babies had seizure either before or during the treatment.
4.1. Management
- Neonates who were active and accepting oral feeds continued only breast feeding and monitored. We managed accordingly with those who were lethargic or showed signs of severe dehydration. Recommendations for treating hypernatremic dehydration comprise an emergency phase (restoration of vascular volume with 20 mL/kg of isotonic intravenous [IV] fluid such as normal saline with 154 mmol/L of sodium) followed by a rehydration phase (the sum of the free water deficit and maintenance fluid requirements administered evenly over 48 hours). Assuming 70% of the infant’s body weight is water, the free water deficit (L) = 0.7 x WT (kg) [1-current sodium/desired sodium]. During rehydration phase, 5% dextrose in 0.2% normal saline (31 mmol/L of sodium) is the usual IV fluid composition. In case of higher serum sodium level, 5% dextrose in 0.45% normal saline usually considered. Oedema in brain, seizures, and death can occur if hypernatremia corrected too rapidly. In cases of severe hypernatremic dehydration, management plan is more difficult. If serum sodium is >175 mmol/L, traditionally isotonic IV fluids, which are actually hypotonic in relation to patient’s serum considered. We can calculate free water content of IV fluid from the formula: Free water (%) = 1- (IV fluid sodium/serum sodium). Thus, when serum sodium is 154 mmol/L, 0.9% normal saline has 0% free water, but if serum sodium is 195 mmol/L, it provides 21% free water. If a patient has a serum sodium, they should calculate the free water deficit of 195 mmol/L and an extensive amount of 0.9% normal saline gave to restore vascular volume, serum osmolality may fall rapidly, leading to cerebral edema and death. Therefore, if the serum sodium is greater than 175 mmol/L, various amounts of 3% normal saline (513 mmol/L sodium) should added so that the IV fluid sodium concentration is approximately 10 to 15 mmol/L lower than the serum sodium level. The maximum rate of decrease of serum sodium level should be 0.6 mmol/L per hour or 15 mmol/L per day. The free water deficit should be calculated to lower the serum sodium level by 15 mmol/day. The correction time may take longer than 48 hours. Frequent monitoring of serum electrolytes (4-6 hourly) along with change of rate of infusion or composition of IV fluid is essential to avoid too rapid correction of serum sodium level [6].
4.2. Best Practice
- Neonatal sepsis like presentation in exclusively breast feed neonate is not always really sepsis but borne in mind about neonatal breast milk hypernatremia.
4.3. Limitations
- Small sample size needs a wide-scale study.
5. Conclusions
- Breast feeding associated neonatal hypernatremia is not as rare as it is commonly believed. Poor feeding and weight loss could be a reason to suspect neonatal hypernatremia in an otherwise healthy baby. Closed monitoring of the mother and baby in the first week of life for successful establishment of breast feeding is essential. There is no reason to stop breastfeeding even if the breast milk sodium is high as it decreases as time progresses. Hypernatremia and hypernatremic dehydration can be prevented by educating mother regarding breast-feeding technique beginning in the antenatal period.
6. Declaration
- FundingThis research work is self-finance.Data AvailabilityThe data are being used to support the findings of this research work are available from the corresponding author upon request. Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of Northeast Medical College, affiliated with Sylhet Medical University, Sylhet, Bangladesh for kind supports.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML