-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2021; 11(1): 8-13
doi:10.5923/j.cmd.20211101.03
Received: Mar. 26, 2021; Accepted: Apr. 21, 2021; Published: Apr. 30, 2021

Lipid Profile in Persons with Schizophrenia on Antipsychotic Medications in Uyo, South-South Nigeria
Henry E. Jombo1, Gabriel O. Ayoade2, Amadi Collins2, Unyime Aniekpon Fabian2, Enoobong K. Nkanga1, Nkemakolam F. Ndionuka2
1Department of Psychiatry, Faculty of Clinical Sciences, University of Uyo, Akwa Ibom State, Nigeria
2Department of Chemical Pathology, Faculty of Clinical Sciences, University of Uyo, Akwa Ibom State, Nigeria
Correspondence to: Henry E. Jombo, Department of Psychiatry, Faculty of Clinical Sciences, University of Uyo, Akwa Ibom State, Nigeria.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Treatment of schizophrenia with antipsychotic medications may be associated with increased risks for metabolic disorders such as weight gain, dyslipidemia, and insulin resistance. This study was conducted to determine the prevalence of dyslipidaemia in patients with schizophrenia on antipsychotic medications and the risk factors associated with it. Fifty two patients diagnosed with schizophrenia were evaluated for lipid profile abnormalities. Study sample had a mean of 26.42±10.8 years, 62.4% were males. Mean values of total cholesterol (TC), low density lipoprotein (LDL), and triglycerides (TG) were significantly higher in patients compared to subjects in controls. Dyslipidaemia was present in 26.9% of the total study sample. The risk of hyperlipidaemia is higher with all typical or atypical class of antipsychotic medications. Chances of hyperlipidaemia and weight gain were higher with long duration of antipsychotic medication use. Treatment with antipsychotic medications is associated with significantly increased risk for hyperlipidaemia.
Keywords: Schizophrenia, Antipsychotic medications, Lipid profile, Nigeria
Cite this paper: Henry E. Jombo, Gabriel O. Ayoade, Amadi Collins, Unyime Aniekpon Fabian, Enoobong K. Nkanga, Nkemakolam F. Ndionuka, Lipid Profile in Persons with Schizophrenia on Antipsychotic Medications in Uyo, South-South Nigeria, Clinical Medicine and Diagnostics, Vol. 11 No. 1, 2021, pp. 8-13. doi: 10.5923/j.cmd.20211101.03.
Article Outline
1. Introduction
- Schizophrenia is a severe mental disorder characterized by significant impairment in family, social and occupational functioning and a chronic progressive nature requiring maintenance treatment. [1] The use of antipsychotic medications, in conjunction with other psychosocial interventions is the cornerstone in the management of many psychotic conditions and they are primarily indicated to treat acute exacerbations of schizophrenia and to prevent relapses. [2]Over the last decade, the use of second generation (atypical) antipsychotics in the treatment of schizophrenia has increased greatly over the first generation (conventional) medications especially in the rich industrialized countries. Antipsychotic drugs have been associated with metabolic side effects including a triad of adverse effects which are significant weight gain, glucose intolerance and hyperlipidemia. [3-6] The net effect of these metabolic side-effects is an increased risk for cerebrovascular disease (CVD) events in a population that is already at increased risk for death from cardiovascular (CV) complications. Patients with schizophrenia have a life expectancy 20% shorter than that of the general population. Approximately 2/3rd increase in mortality is attributed to co-morbid medical illness such as obesity, Type 2 diabetes mellitus and cardiovascular diseases with lifestyle factors and treatment factors playing additive roles. [7-9]Recent studies have shown that antipsychotic drugs cause elevation of serum triglycerides (TG) and total cholesterol (TC), but with greater effects on TG concentrations. High serum TG seemed to be the primary significant dyslipidaemia associated with antipsychotic medication use. Elevated TC could also be found. Previous studies have also reported that while certain demographic and lifestyle factors may be important they are not consistent risk factors for dyslipidaemia among users of antipsychotic medications. More specific risk factors for dyslipidaemia may include period of antipsychotic medication use and dosage. [4]Due to long term use of these drugs for maintenance therapy, their metabolic side effects should be considered. Thus, there is the need for routine monitoring of the lipid profile to minimize the additional risk of hyperlipidemia and to guide to the choice of antipsychotic therapy.This study was conducted to determine the prevalence of dyslipidaemia in patients with schizophrenia and the relationship between antipsychotic medications use and dyslipidaemia and related factors.
2. Materials and Methods
2.1. Location of the Study
- This cross-sectional study was conducted at University of Uyo Teaching Hospital from June 2019 to December 2019. The hospital is located in Uyo, the capital city of Akwa Ibom State, Nigeria. The hospital is a 500 bed capacity federal tertiary healthcare centre in the South-South geopolitical zone of Nigeria. The hospital also receives patients from Cross-River, Rivers, Abia states and from other neighboring states. The diagnosis of schizophrenia was made according to the tenth edition of the International Classification of Diseases and health-related disorders (ICD -10) criteria. (10) Clinically generated data for each subject enrolled were matched to the ICD -10 criteria.
2.2. Subjects
- The sample size was calculated using a public domain software available on-line (www.statpages.org) [11] using a prevalence of dyslipidaemia following antipsychotic treatment as determined from previous Nigerian study (56%) [12]. The sample consisted of 92 participants consisting of 52 cases and 40 age and gender matched controls. A subject is enrolled if he/she met the following inclusion criteria: a diagnosis of schizophrenia as confirmed by a consultant psychiatrist using the ICD 10 criteria, who has been receiving anti-psychotic medications for at least one year prior to study entry, adults above the age of 18years, with no history of any underlying medical condition associated with hyperlipidaemia; no history of any medication which is associated with glucose intolerance/insulin resistance eg hydrochlorthalidone, beta blockers, glucocorticoids, phenytoin, nicotinic acid, cyclosporine, pentamidine, and narcotics. The exclusion criteria were: refusal to give consent, acute or chronic medical conditions including history of diabetes mellitus, malignancy, epilepsy, endocrine diseases such as thyroid and adrenal diseases, pregnancy, contraceptives, narcotic, corticosteroid or spironolactone therapy, sedative hypnotic withdrawal, beta-blockers, thiazide diuretics etc.
2.3. Procedure
- Approval for the study was obtained from the Research and Ethical Committee of the University of Uyo Teaching Hospital. Informed consent was obtained from patients or their accompanying family members. Patients who met the inclusion criteria were consecutively recruited into the study after a comprehensive psychiatric evaluation and diagnosis by resident doctors in psychiatry. The Mini International Neuropsychiatric Interview (MINI) English Version 5.0.0 was administered to confirm the diagnosis of schizophrenia in the participants. The MINI was designed as a brief structured interview for the major Axis 1 diagnosis in the Diagnostic and Statistical Manual (DSM-IV) and ICD-10. [13]
2.4. Measures
2.4.1. Socio-Demographic Characteristics
- A socio-demographic questionnaire designed by the authors was used to obtain information Measures evaluated includes socio-demographic details (age of the patient and family member, gender, educational status, marital status, religion) illness related variables (total duration of illness).
2.4.2. Medication Profile
- The medication profile of each individual patient was obtained through chart review of the medication record files domiciled in the hospital. Data recorded include: The number of antipsychotic medicines on the patients’ current treatment regimen. Exposure to antipsychotic medication was measured as 1.class of antipsychotics used 2, duration of antipsychotic use 3, doses of medication used. All the antipsychotics used by the test subjects were converted to their chlorpromazine equivalent doses.
2.4.3. Body Mass Index
- The height of the subjects was measured (to the nearest 0.1 cm) using an improvised wooden stadiometer mounted on a vertical wall with the respondent standing erect against the wall on a horizontal floor without shoes. The head was placed so as to ensure that the external auditory meatus and the angle of the eye were on a horizontal line. The Weight of the participants was measured in kilograms to the nearest 0.5kg using a Hanna-calibrated bathroom scale. Each subject was weighed wearing light clothing without shoes or stocking. BMI was computed as the weight (kg) / (height [m])2 (ie kg/m2) [14]. The BMI was classified according to World Health Organization(WHO) classification which defines normal as <25.0 mg/m2, overweight as BMI of 25.0 kg/m2 – 29.9 kg/m2 and obesity as a BMI of > 30.0 kg/m2. [15]
2.4.4. Analysis of Blood Samples
- A blood sample for triglycerides, cholesterol, low-density lipoproteins (LDL) and high-density lipoproteins (HDL) assay was obtained in the morning after 12 hours of fasting through the antecubital vein. The total cholesterol was assayed using the enzymatic method (CHOD-PAP). Triglycerides were assayed using enzymatic methods (GPO-PAP). HDL-C was assayed with direct enzymatic method. They were all analyzed on automated chemistry platform (Selectra ProM, ELITech Group). LDL was calculated using the Frieldewald formula. [16] Body mass index (BMI) was computed using the formula of weight (kg)/height (m)2. Dyslipidaemia was defined as an abnormality of any of the lipid profile components, that is, elevated total cholesterol (TC) ≥ 5.2 mmol/l, low density lipoprotein cholesterol ≤ 3.4 mmol/l, triglycerides (TG) ≥ 1.7 mmol/l, and high density lipoprotein (HDL) < 1.04 mmol/l. [17]Data Analysis: Descriptive statistics such as frequencies, mean and standard deviation were computed for socio-demographic and clinical characteristics of the participants and other variables as appropriate. Relevant inferential statistics such as t-test and Pearson’s correlation was used to determine the relationship between outcome and independent variables. The statistical package for social sciences (SPSS) version 20 was used for analysis. Significance was computed at p < 0.05.
3. Result
- Ninety two participants, comprising 52-test subjects and 40-controls were included in the study. The mean age of the test subjects was 28.42 ± 10.8 years. More than half of them were males (62.4%). The majority of the participants (82.3%) were unmarried and about 78.3% of them had formal education to at least secondary school level and 76.8% of them were unemployed. The mean duration of illness was 8.33±8.1 years and the mean duration of use of antipsychotic drugs 5.01±3.4 years. Mean weight gain of participants after one year of antipsychotic medications use was 10.84±5.3kg. See table 1
|
3.1. Distribution of the Medication-Related Variables
- About 24.2% of subjects were on conventional antipsychotics and the three commonly prescribed first generation antipsychotics were: haloperidol (37.2%) trifluperazine (25.7%) chlorpromazine (22.5%). The remaining 14.6% were on long acting injectables like Fluphenazine decanoate or Flupenthixol decanoate.About 30.4% of the subjects were on atypical antipsychotics. The most commonly prescribed serotonin dopamine antagonists (SDAs) were olanzapine (43.4%), risperidone (50.2%), quetiapine (3.1%) aripiprazole (2.5%) clozapine (0.8%). About 45.4% of the subjects were on polytherapy regimen and common combinations were: any class of antipsychotics like combination of two conventional antipsychotics or conventional antipsychotics and atypical and any class of antipsychotics and long acting injectables. The dosing frequency of 55% of the subjects was at least twice per day and 27% of participants were on once daily dose regimen. The mean daily dosage per day in milligram for subjects on chlorpromazine was 320 mg/day. The subjects on haloperidol had 10.40 mg/day mean value while those prescribed trifluperazine 9.50 mg/day. The mean chlorpromazine equivalent dosage was 346.32mg and 190.0mg for those on haloperidol and trifluperazine respectively.The mean daily dosage for olanzepine was 15.25±3.5. mg/day. Subjects on risperidone received a mean daily dosage of 3.55±0.9 mg/day The chlorpromazine equivalent dosage for patients on olanzapine and risperidone was 305.0mg and 355mg respectively.
3.2. Antipsychotic Medications and Weight Gain
- The mean weight gain of the test subjects in 1year and 5 years of antipsychotic medication use was 6.12±5.3 and 11.92±6.17 mg respectively. Weight gain during the period of treatment was determined from the difference between the weight at presentation for treatment and the weight after 1 and 5 years of treatment respectively. By BMI values, 2.1% were underweight, 25.6% of subjects had normal weight, 53.8% were overweight and 18.5% subjects were obese. The BMI of the cases were significantly different from the controls (t=4.17, p < 0.001). There was also a weak correlation between weight gain and the period of antipsychotic use (r=0.43, p = 0.03).
3.3. Antipsychotic Medications and Dyslipidaemia
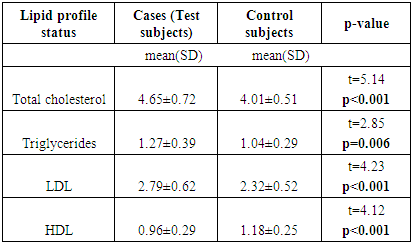
- The prevalence of dyslipidaemia among the test subjects in this study was 26.9% compared to 7.5% in the controls. The atypical antipsychotics were as likely as the conventional antipsychotics to cause significant increases in the blood level of cholesterol, triglycerides, LDL.Among the twenty (39.4%) cases that received atypical antipsychotics, 5 (20.0%) developed dyslipidaemia. From the 13 (29.2%) that received conventional antipsychotics, 3 (23.1%) developed dyslipidaemia. Among the 19 (36.4) that received combined atypical and conventional drugs 6(31.6%) developed dyslipidaemia. The total cholesterol (TC), TG and LDL-C in patients receiving antipsychotics were significantly higher than in controls (t=5.14, p < 0.001). The mean value of triglyceride (TG) for cases was significantly higher than the mean value of the control subjects (t=2.85, p < 0.006). The mean value of high density lipoproteins (HDL) was significantly lower than the controls (t=4.12, p < 0.001).
|
3.4. Dyslipidemia and Associated Factors
- Triglyceride levels was associated with duration of treatment (t=2.08, p=0.04) and BMI level (t=1.86, p=0.03). The age of participants, gender, duration of illness, ages of onset of illness were not significantly related to the risk of developing hypertriglyceridemia. The blood cholesterol level, LDL level and HDL level did not show statistically significant increases in terms of age (p=0.2), gender (p=0.12) and duration of illness (p=0.07).
4. Discussion
- This study investigated abnormalities in lipid profile following antipsychotic medication use. Elevated total cholesterol (TC) and serum triglyceride (TG) levels has been associated with an increased risk for CV events, such as myocardial infarction and stroke and is unhealthy for a population already at an increased risk for death from cardiovascular (CV) complications from factors such as smoking, sedentary lifestyles, diabetes mellitus [18-21].Treatments with antipsychotic medications in our study were associated with significant dyslipidaemia when compared with healthy controls. For all antipsychotic users in our sample, there were statistically significant differences in the mean values of all lipid parameters between the cases and the controls. The atypical antipsychotics were as likely as the conventional antipsychotics to cause significant increases in blood cholesterol, LDL, and triglycerides. This result is consistent with previous studies from Nigeria which have reported similar findings. Worldwide, recent studies have also been consistent in reporting increased risk of hyperlipidaemia in antipsychotic medicated populations compared to the general patient population [4,17,22-23]. Studies on the differential impact of atypical antipsychotics and conventional antipsychotics on lipid profile have reported a more significant impact of the atypical antipsychotics compared to the conventional antipsychotics and also, some atypical antipsychotics are reported to be associated with more weight gain and dyslipidaemia than others [24-27]. In this study, all antipsychotic medications use whether individually or in combination use caused significant increase in lipid parameters like serum total cholesterol, serum triglycerides, and serum total lipids while causing significant decrease in HDL fraction. Also, we found significantly higher mean values of lipid parameters in persons using both conventional and atypical antipsychotics together compared to those on either conventional or atypical antipsychotics. This is consistent with previous study that have reported similar finding [25]. The prevalence of dyslipidaemia in this study was 26.9%. Dyslipidaemia in our sample was significantly higher than in the healthy controls. This may not be totally unrelated to the degree of antipsychotic medication induced weight gain observed in this study. A high proportion of the participants, about half of the subjects in this study had remarkable increases in weight gain which was related to the duration of antipsychotic medication use. After about one year of all antipsychotic medication use, the mean weight gain among study participants was 10.84±5.3kg representing 11.5% gain in weight over a one period of antipsychotic medications use.. Also, life-style issues that may include redundancy and sedentary living noted among participants, given that 76.8% of participants are unemployed, may be contributory.The prevalence of dyslipidaemia in our sample is in disagreement with a previous Nigerian studies which have reported much higher prevalence rate of 56% [12]. Dyslipidaemia in our sample is consistent with the study result of Meyer and Koro [4]. The differences in reported prevalences of dyslipidaemia may partly reflect differences in study design, definition and estimation of blood lipids and characteristics of the study population. The role of weight gain in the etiology of dyslipidaemia in subjects on antipsychotic medications has been reported in previous studies [28-30]. In the present study, a high proportion of the participants had significant gain in weight with about 73.1% in the overweight and obese category. Subjects with a relatively high average BMI values were significantly more likely to have dyslipidaemia than those with relatively low average BMI. Studies have reported that medications most associated with dyslipidaemia are also those that induced the greatest amount of weight gain. Obesity therefore is an established risk factor for developing dyslipidaemia [28,29]. About 73.3% of our sample had BMI score in the overweight and obese range. According to a study by Moreno C, three months after starting treatment with second generation antipsychotics more than 70% of patients had significant weight gain. A previous study has reported that dyslipidaemia may be related to the duration of antipsychotic use [4]. In this study, the mean duration of antipsychotic use was 5.01±2.5 years, the duration of antipsychotic use in our sample may be a contributory factor in the prevalence of dyslipidaemia in the present study.Clinically, it is important to monitor weight gain and metabolic adverse event and to switch to antipsychotic agents with lower risk potential for hyperglycemia, dyslipidemia, and/or substantial weight gain in the course of treatment [31]. The high number of adult patients with schizophrenia treated with these antipsychotic agents has resulted in public health concerns and the compelling need for long term monitoring of patients on these medications. This study has some limitations. First the small sample size and the cross-sectional nature of the study cannot confirm causality between the factors studied, therefore, the value must be limited to the descriptive and its exploratory nature. The result may not be generalizable giving that antipsychotic medications are widely used in other mental illness and also given that schizophrenia may in itself be a risk factor for the development of an adverse metabolic complications.
5. Conclusions
- Patients on antipsychotic medication for schizophrenia or other illnesses should be considered a high-risk group for dyslipidaemia. Current use of conventional or atypical antipsychotics is associated with an increased risk of dyslipidaemia which seems to vary with medication.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML