Azer Abbas1, Mohamed Hamid Awadelseid2
1Departement of Orthopedic Alazhary University, Khartoum, Sudan
2Departement of Orthopedic Excellence Trauma Centre, Khartoum, Sudan
Correspondence to: Mohamed Hamid Awadelseid, Departement of Orthopedic Excellence Trauma Centre, Khartoum, Sudan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: Unstable pelvic fractures are commonly as a result of high energy trauma. and the management of unstable pelvic fracture is difficult and need multidisciplinary team. all the unstable patterns carry a high risk of severe hemorrhage and are life-threatening. open reduction and internal fixation of displaced pelvic fracture has become more accepted as clinical experience and certain technologies had improved, and it is considered the most stable form of stabilization. Sacroiliac(SI) disruption reflects a massive, disruptive energy force with concurrent soft tissue injury. Management of SI joint disruption is dependent on the degree of instability. The SI joint fracture dislocation can be fixed after the reduction by different methods one of them is fixation with plate. Specific objectives: To determine the clinical and functional outcome of plate fixation of the sacroiliac joint dislocation or fracture dislocation. Patients and methods: This is a cross sectional hospital based study done on patients withsacroiliac joint dislocation and fracture dislocation in Khartoum north teaching hospital over period of three years from November 2016 to October 2019. Results: The total number of patient was 20 with 21 joints the age ranged from 15 years to60 years the mean is 35 + 15 years Stander deviation. The outcome at 6 months according to post-operative reduction on x-ray; there were 6 patients (30%) with excellent reduction the results were 5(25%) excellent and 1(5%) good. There were 13 patients (65%) with good reduction the results were 10(50%) excellent and 3(15%) good. There was one patient with fair reduction the result was (5%) excellent. (P-value 0.03). Conclusion: These injuries are the result of high-energy trauma, which places patients atrisk of multiple life-threatening injuries. The fixation of SI joint with plate is an effective, safe procedure and hasgood results and can use as an alternative to SI screw.Early surgery for unstable pelvic fracture and early rehabilitation give thebest results Functional outcomes of unstable pelvic fracture following surgical treatment are extremely encouraging. The age of the patients significantly influence the outcomes. p-value 0.02. Tile‟ type C showed the best outcome with plate fixation of SI joint. p-value 0.04 the associated injury influence the outcome at 3 months (p-value 0.03) and 6 months (p-value 0.06) not influence the outcome.
Keywords:
Sacroiliac Joint, Sudanese patients, Plate fixation
Cite this paper: Azer Abbas, Mohamed Hamid Awadelseid, Outcome of Sacroiliac Joint Plate Fixation in Sudanese Patients, Clinical Medicine and Diagnostics, Vol. 10 No. 1, 2020, pp. 12-19. doi: 10.5923/j.cmd.20201001.02.
1. Introduction
Pelvic fractures are mostly caused in young and middle-aged males by high energy as Yang et al stated [1]. Fractures of the pelvis account for less than 5 per cent of all skeletal injuries, but they are particularly important because of the high incidence of associated soft tissue injuries and the risks of severe blood loss, shock, sepsis and adult respiratory distress syndrome (ARDS). Like other serious injuries, they demand a combined approach by experts in various field as Ertel et al stated [2].Unstable pelvic fractures are commonly as a result of high energy trauma and the management of unstable pelvic fracture is difficult and need multidisciplinary team. all the unstable patterns carry a high risk of severe hemorrhage and are life-threatening as Dalal et al stated [3].Pelvic fractures with disruption of the important weight-bearing sacroiliac area can lead to impaired gait due to malunion or pelvic obliquity, back or buttock pain arising from the sacroiliac joint, and permanent neurologic damage as Simpson et al stated [4].Open reduction and internal fixation of displaced pelvic fracture has become more accepted as clinical experience and certain technologies had improved, and it is considered the most stable form of stabilization as Madhat stated [5]. Early rigid fixation and anatomical reduction of the pelvic ring are recommended to reduce mortality and allow early ambulation as Tile stated [6].Sacroiliac disruption reflects a massive, disruptive energy force with concurrent soft tissue injury as Leighton et al stated [7].The crescent fracture consists of a posterior iliac wing fracture with extension into the sacroiliac joint and a dislocation of the inferior half of the sacroiliac joint.The posterior superior iliac spine remains firmly attached to the sacrum by the strong posterior ligaments as Borrelli et al stated [8,9].Management of SI joint disruption is dependent on the degree of instability as mention at Rocked and Green [10].The SI joint fracture dislocation can be fixed after the reduction by different methods one of them is fixation with plate. The fixation of pelvis and acetabular fracture introduced lately in Sudan, but there is little data in the local literature about the outcome of fixation of such fractures. The purpose of this study is to determine the outcome of the plate fixation of the sacroiliac joint in unstable pelvic fractures.
2. Patients and Methods
Patients with sacroiliac joint dislocation and fracture dislocation in Khartoum north teaching hospital, conducted over period of three years from November 2016 to October 2019, total patients coverage during the study period.All patients presented with dislocation or fracture dislocation of sacroiliac joint treated surgically with plating. The plain X-ray shows Widening of the sacroiliac and the Computed tomography shows sacroiliac joint anatomy and fracture pattern. The follow up period was 6 months to one year.Data Collection:Data collected using questionnaire and from hospital records and the patients. All the patients assessed at day zero, three clinically for postoperative complications. The post-operative reduction assessed radiologically using digital X-ray, the reduction is excellent if the gap less than 5 mm, good if the gap 6-10 mm, fair if the gap 11-15 mm and poor if more than 15 mm. At two weeks the patient assessed for pain using visual analogue scale of pain. At three and six months the patients assessed clinically using Majeed score, this functional scoring system consisted of several questions in seven items. These items included pain, work, sitting, sexual intercourse, walking aids, gait and walking distance.Each score represented a number of points, which make up the total score ranging from 0 to 100, if the score more than 85 described excellent, if the score 70-84 described good, if the score 55-69 described fair and if less than 55 describe poor.Data analysis:The study analyzed using statistical package for social science (SPSS) from IBM Company. Version 20. Frequency -chi square set point (pvalue < 0.05).Ethical consideration:Verbal consent will be obtained from the patient, ethical clearance from the ethical committee of Sudan Medical Specialization Board (SMSB).Surgical technique:For anterior exposure of the sacroiliac joint, the patient placed supine with the injured side tilted up with a roll for easier access and manipulation. The limb draped free so it may be manipulated into flexion to relax the iliopsoas muscle. The incision parallels the iliac wing; beginning at the anterior superior iliac spine, extending posteriorly we must take care to protect the lateral femoral cutaneous nerve because injury to this nerve may cause a painful neuroma. The external oblique insertion on the ilium lifted up, and the iliacus elevated from the inner cortex of the iliac wing. As the dissection coursed medially, the sacroiliac joint hump reached. One to two centimeters medial to this joint lies the fifth lumbar nerve root. The fifth lumbar-nerve root limited medial dissection and can be damaged by dissection or retraction. We achieved reduction by bring the ilium into place, a shanz pin placed in the ilium can be used to aid manipulation or can use the plate in reduction of posterior displacement. The sacroiliac joint held in place temporarily with kirshner wires or a staple. For the internal fixation one or two recon plates 3.5 used for fixation with 3.5 cancellous screws.All the patients operated by the same surgeon and same approach most of them within 2 weeks, assessed early post-operative, 2 weeks postoperative, 3months post-operative and 6 months post-operative.MAIN OUTCOME MEASUREMENTS:Pelvic fracture classification, Tile classification.Functional outcomes, the Majeed Outcome Score.
3. Results
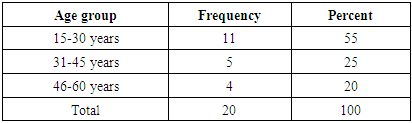
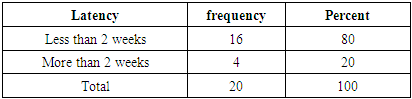
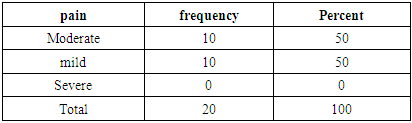
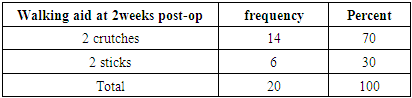
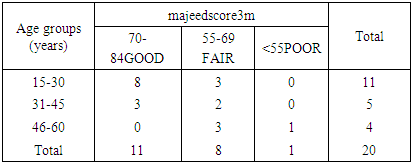
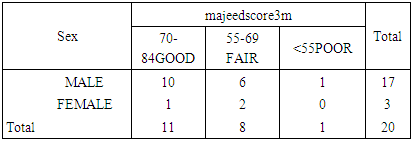
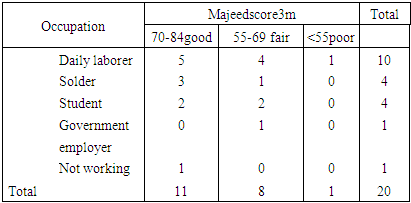
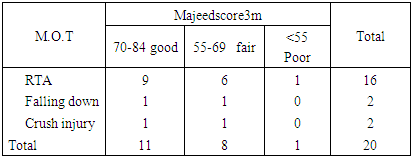
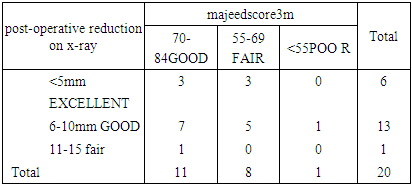
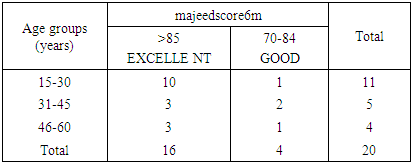
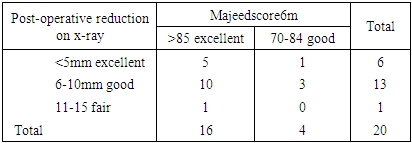
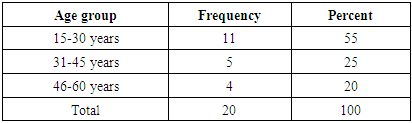
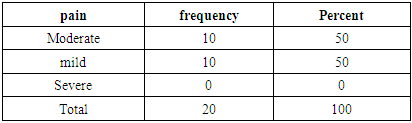
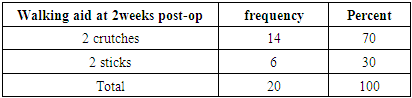
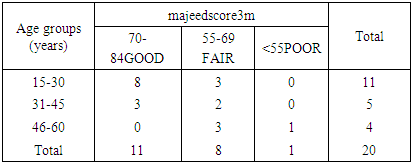
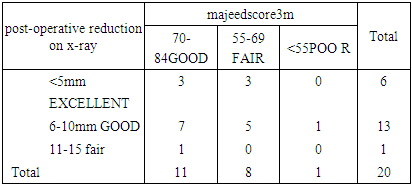
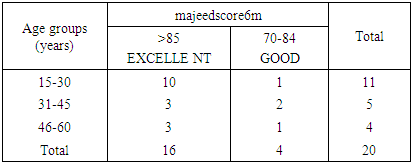
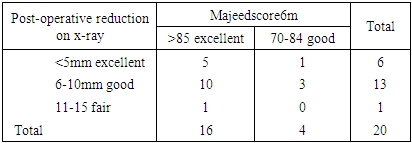
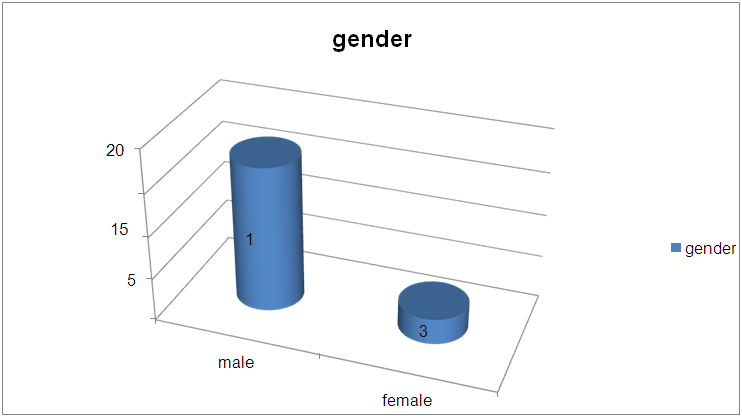
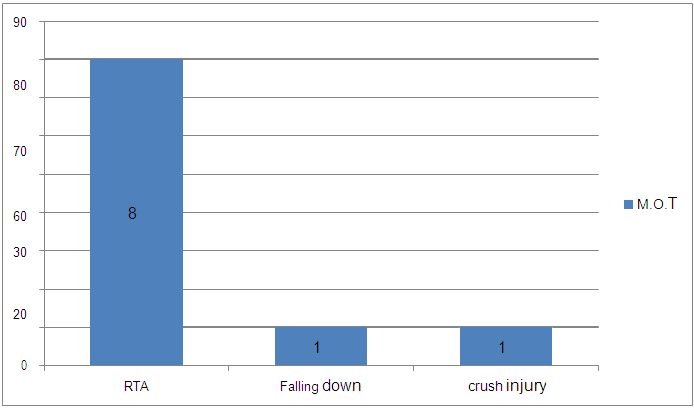
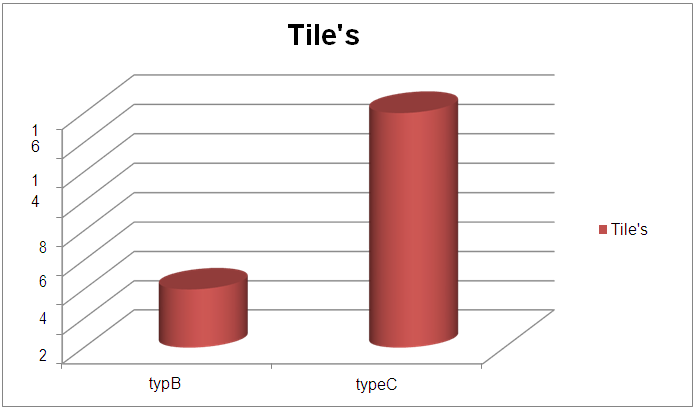
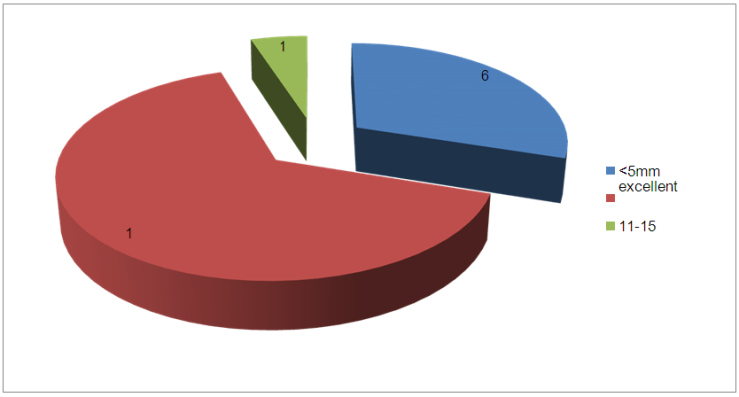
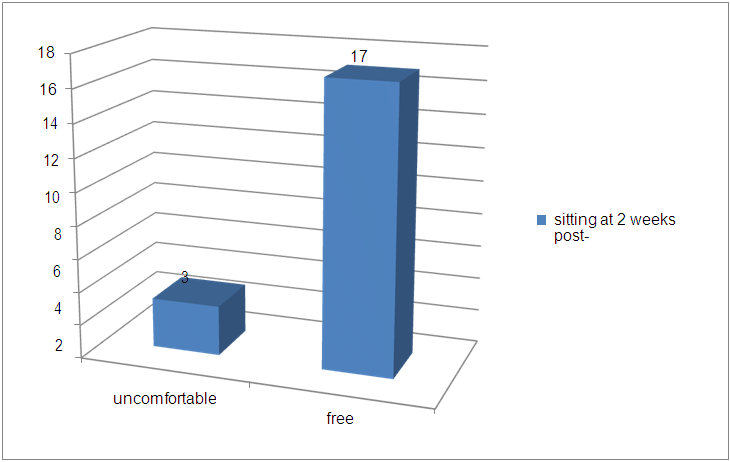
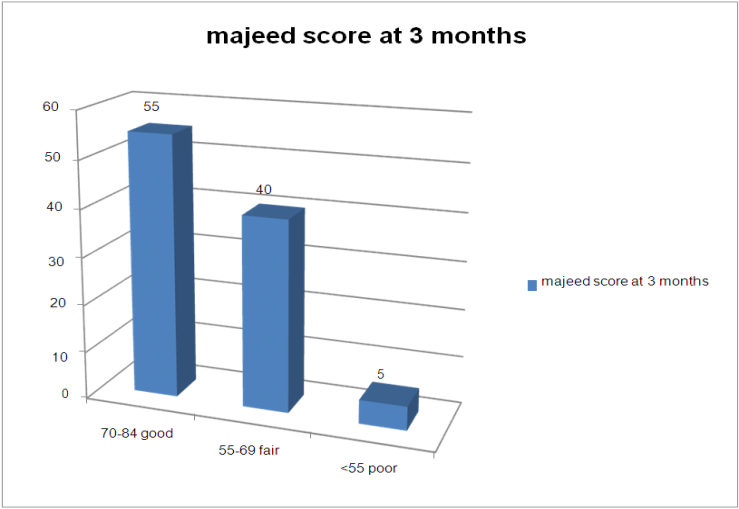
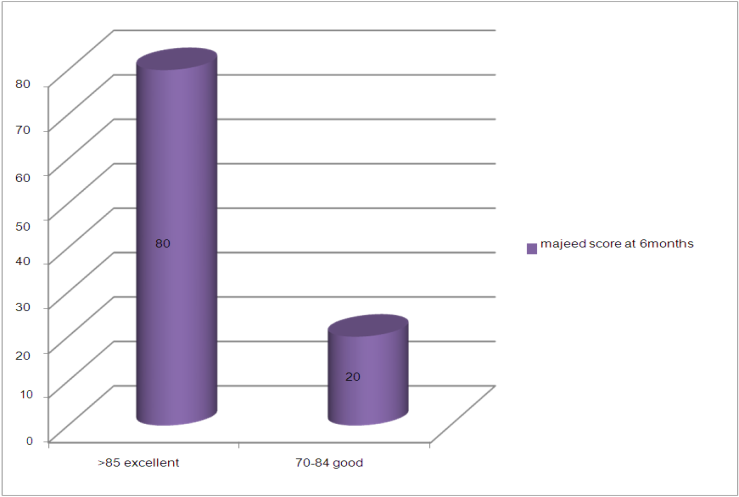
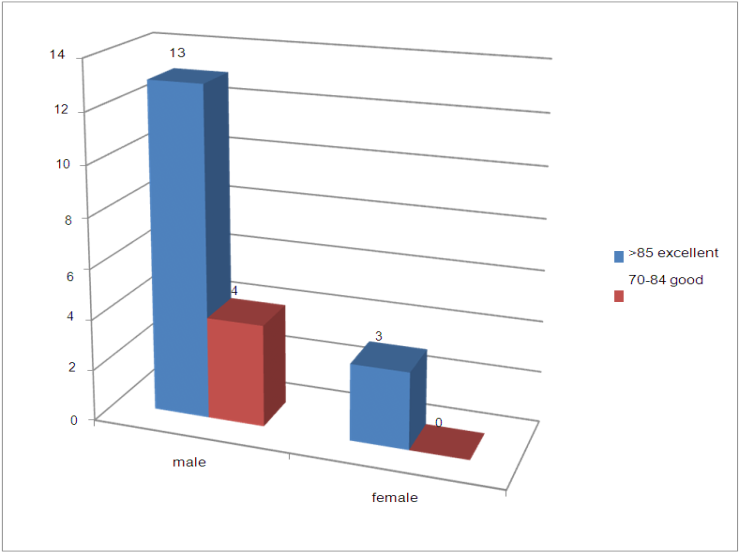
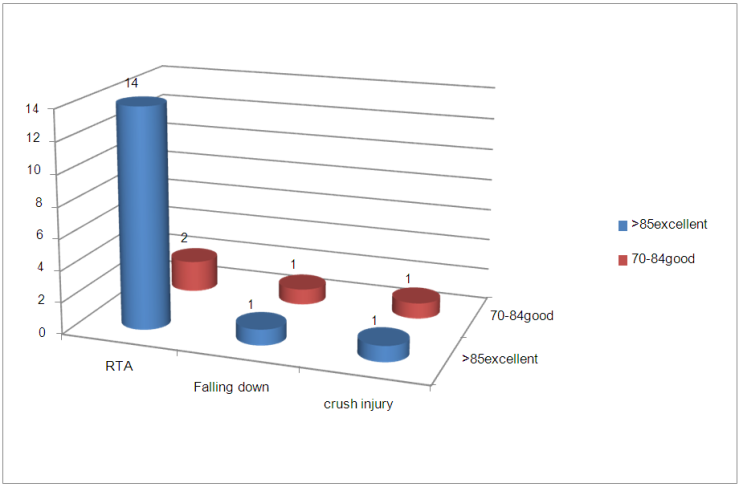
The total number of patient was 20 with 21 joints the age ranged from 15 years to 60 years the mean is 35 + 15 years Stander deviation. 11 (55%) patient were from the age group 15-30 years, 5 patients (25%) were from age group 31-45 years, 4 patients (20%) were from age group 46-60 years and no patient less than 15 years or more than 60 years.Concerning gender; 17 patients (85%) were male and 3 patients (15%) were female. Ten patients (50%) were single and 10 patients (50%) were married.The follow up period was 6 months to one year, all the patients included.About the occupation; 10 patient (50%) were daily laborer, 4 patients (20%) were solder, 4 patients (20%) were student, 1patient (5%) was government employer and 1 patient (5%) not working.According to mode of trauma; 16 patients (80%) were victim of R.T.A, 2 patients (10%) fell down and 2 patients (10%) were victim of crush injury.The interval between the date of injury and date of operation; 16 patients (80%) were operated within 2 weeks and 4 patients (20%) were operated within more than 2 weeks.Concerning the Tile‟s classification; 4patients (20%) were type B and 16 patients (80%) were type C. Thirty percent of patients were associated with other injuries, as follows: 1(5%) with lower limb 2(10%) associated with head injury, 2(10%) associated with abdominal injury, 1(5%) associated with acetabular fracture and 14(70%) not associated with other injury.The post-operative complication such as neurovascular injuries, deep vein thrombosis weren‟t detected in all patients. concerning the post-operative reduction using digital X-ray; in 6 patients (30%) the reduction was excellent (<5mm), in 13 patients (65%) of patient the reduction was good (5-10mm) and in one patient (5%) the reduction was fair (11-15mm).At 2 weeks post-operative:Ten patients (50%) were complaining of moderate pain and 10 patients (50%) were complaining of mild pain using pain scale. Three patients (15%) sat uncomfortably and 17 patients (85%) sat freely. Fourteen patients (70%) used 2 crutches during walking and 6 patients (30%) used 2 sticks during walking.At 3 months post-operative:The pain; one patient (5%) was feeling pain with moderate activity and reduced by rest, 18 patients (90%) were feeling mild pain with normal activity and one patient had no pain. Twelve patients (60%) had no regular work and 8 patients (40%) practice slight work. Three patients (15%) were sitting uncomfortably and 17patients (85%) were sitting freely. Sexual intercourse was uncomfortable for 1 patient (5%) and free for the rest of the patients. Three patients (15%) used crutches during walking, 8 patients (40%) used 2 stick, 8 patients (40%) used one stick and one patient (5%) didn‟t use stick during walking. The gait unaided pattern; was small steps in one patient (5%), gross limp in 2 patients (10%) , moderate limp in 4 patients (20%), slight limp in 8 patients (40%)and normal in 5 patients (25%). The walking distance was very limited time and distance in 3 patients (15%), limited with stick difficult without in 2 patients (10%), one hour with stick limited without in 6 patients (30%) and one hour without stick in 9 patients (45%).Majeed score was good (70-84) in 11 patients (55%), fair (55-69) in 8 patients (40%) and was poor (<55) in one patient (5%). The outcome at 3 months according to age group; there were 11(age group 15-30) the result were 8(40%) good and 3(30%) fair. There were 5 (age group 31-45) the result were 3(15%) good and 2(10%) fair. There were 4 (age group 46-60) the results were 3(15%) good and 1(5%) fair. (p-value 0.04)The outcome at 3 months according to sex; in the male the result were 10(50%) good, 6(30%) fair and 1(5%) poor. In the female the results were 1(5%) good and 2(10%) fair. (P-value 0.03)The outcome at 3 months according to occupation; there were 10 patients daily laborer the results were 5(25%) good, 4(20%) fair sand 1(5%) poor. 4 patients were solder the results were 3(15%) good and 1(5%) fair. There were 4 students the results were 2(10%) good and 2(10%) fair. There was 1 government employer with (5%) fair result and 1(5%) not working with good result. (P-value 0.08)- The outcome at 3 months according to mode of truma 16 patients (80%) were victim of road traffic accident the results were 9(45%) good, 6 (30%) fair and 1(5%) poor. There were 2 fell down the results were 1(5%) good and 1(5%) fair. There were 2 victim ofcrush injury the results were 1(5%) good and 1(5%) fair. (p-value 0.06)The outcome at 3 months according to interval between the date of injury and date surgery; there were 16 patients (80%) operated on within 2 weeks the results were 9(45%) good, 6(30%) fair and 1(5%) poor. And 4 patients operated on more than 2weeks the result were 2(10%) good and 2(10%) fair. (p-value 0.001)The outcome at 3 months according to Tile‟s type; there were 4 patients (20%) with type B the results were 2(10%) good, 1(5%) fair and 1(5%) poor. There were 16 patients (80%) with type C the result were 9(45%) good and 7(35%) fair. (p-value 0.07)The outcome at 3 months according to associated injury; 14 patients (70%) were not associated with other injury the results were 7(35%) good and 7(35%) fair.There was one had lower limb fracture the result was good. There were 2 with head injury the results were 1(5%) fair and 1(5%) poor. There were 2 patients (10%) with abdominal injury the results were 2(10%) good. There was 1 patient (5%) with acetabular fracture the result was good. (p-value 0.03)The outcome at 3 months according to post-operative reduction on x-ray; there were 6 patients (30%) with excellent reduction the results were 3(15%) good and 3(15%) fair. There were 13 patients (65%) with good reduction the results were 7(35%) good, 5(25%) fair and 1(5%) poor. There was one with fair reduction the result was (5%) good. (p-value 0.001)At 6 month post-operative:Four patients (20%) were complaining of mild pain with activity and 16 patients (80%) were complaining of slight pain or no pain. Three patients (15%) with no regular work, 3 patients (15%) with slight work, 6 patient (30%) with same job with reduced performance and 8 patients (40%) with same job and performance.All the patients were sitting freely. All the patients practice sex freely. Five (25%) used one stick and 15 (75%) didn‟t use stick. The gait unaided pattern; there was 1 patient (5%) with moderate limp, 4 patients (20%) with slight limp and 15 patients (75%) with normal gait. According to walking distance; there was 1 patient (5%) limited with stick, 1 patient (5%) one hour with stick limited without, 2 patients (10%) one hour without pain and 16 patients (80%) normal for age and general condition. One (5%) developed implant failure anterior plate brakeage.Majeed score was excellent in 16 patients (80%) and good in 4 patients (20%). No shorting or restriction of movement of hip joint. All the patients were fully satisfied.The outcome at 6 months according to age group; there were 11 patients (55%) (age group 15-30) the result were 10 (50%) excellent and 1(5%) good, There were 5 patients (25%) (age group 31-45) the result were 3(15%) excellent and 2(10%) good. There were 4 patients (20%) (age group 46-60) the results were 3(15%) excellent and 1(5%) good. (p-value 0.02)The outcome at 6 months according to sex; in the male (85%) the results were 13(65%) excellent and 4(20%) good. In the female (15%) the results were 3(15%) excellent. (p-value 0.03)Table 1. Distribution of study population according to age group; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation Age group Frequency Percent
 |
| |
|
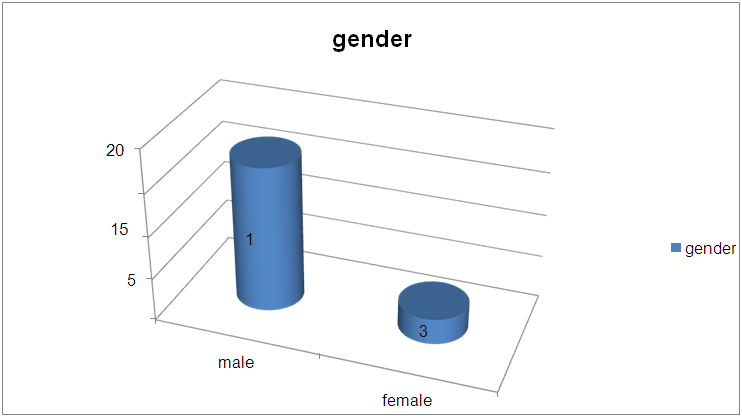 | Figure 1. Distribution of study population according to gender; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
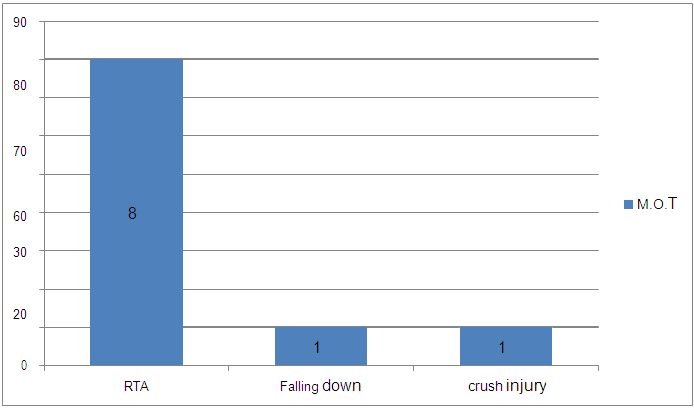 | Figure 2. The distribution of study population according to M.O.T; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
Table 2. Delay of the surgery; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
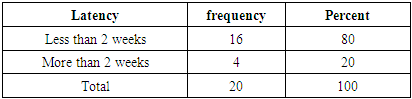 |
| |
|
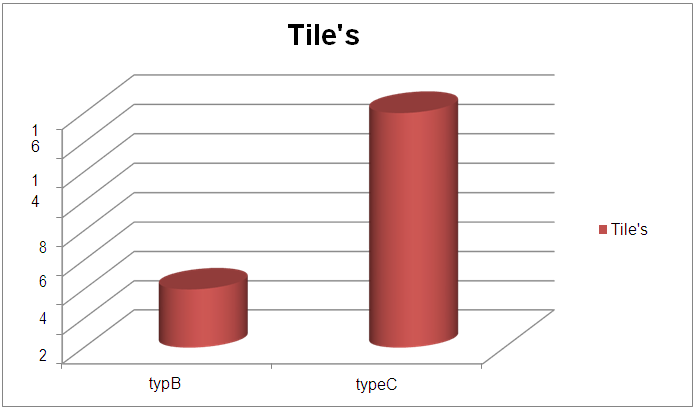 | Figure 3. The distribution of study population according to Tile‟s classification; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
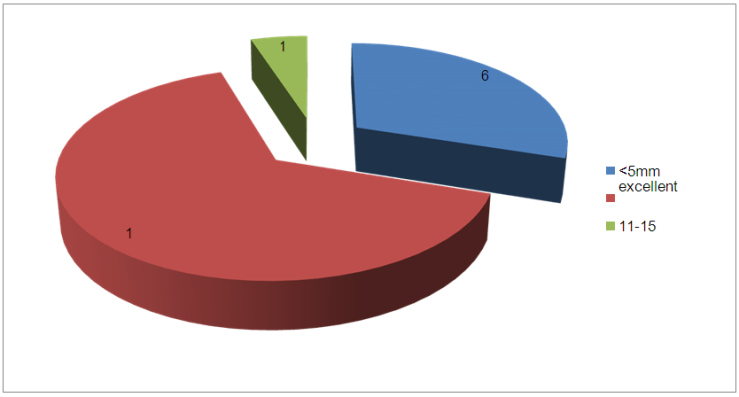 | Figure 4. The Pattern of post-operative reduction; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
Table 3. Severity of pain at 2 weeks post-operative; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
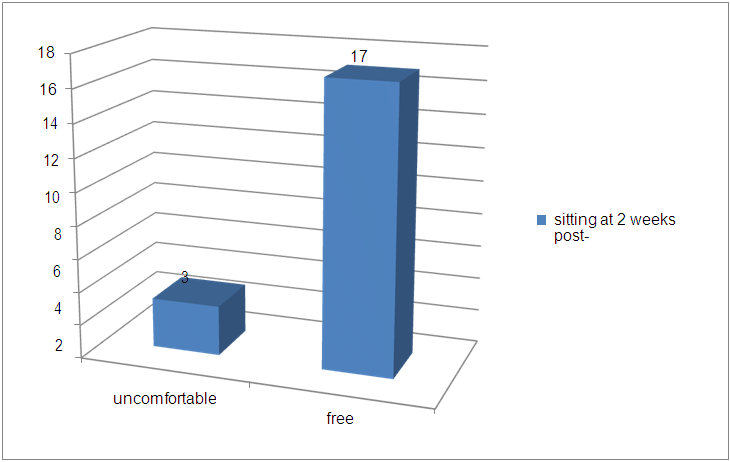 | Figure 5. The sitting at 2 weeks post-operative; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
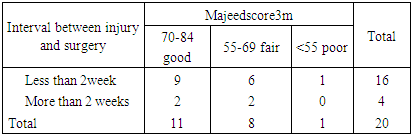
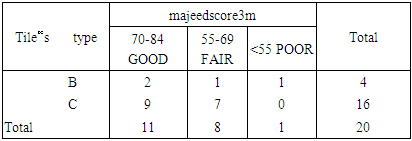
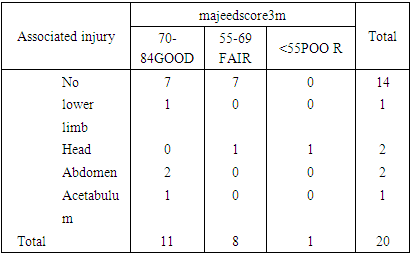
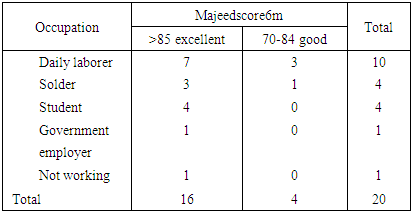
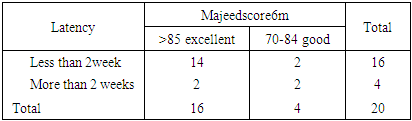
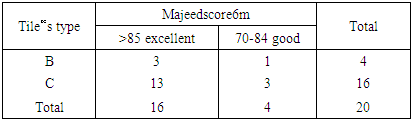
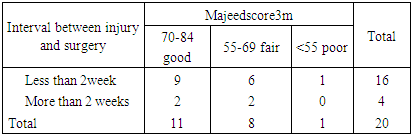
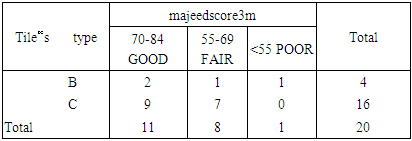
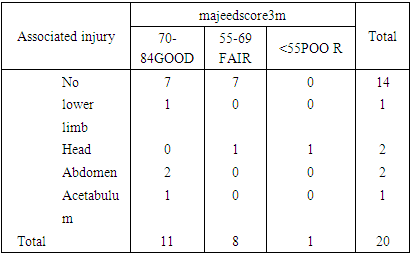
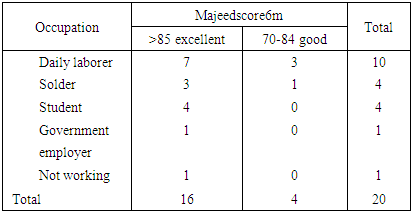
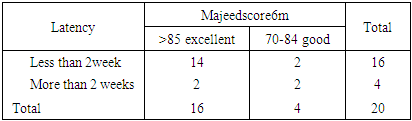
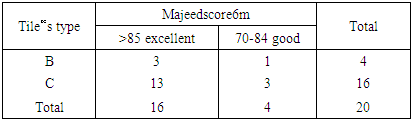
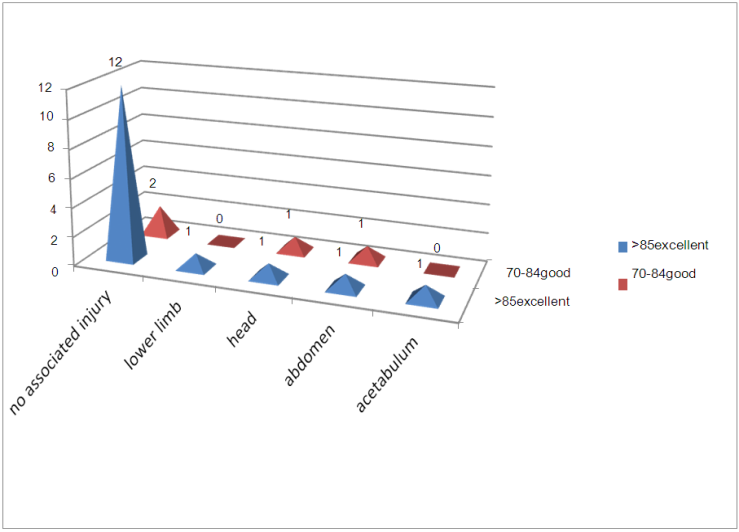
The outcome at 6 months according to occupation; 10 patients (50%) were daily laborer the results were 7(35%) excellent and 3(15%) good. 4 patients (20%) were solder the results were 3(15%) excellent and 1(5%) good. There were 4 students the results were 4 excellent. There was 1 government employer with (5%) excellent result and 1 not working with (5%) excellent result. (p-value 0.06)The outcome at 6 months according to mode of truma16 patients (80%) were victims of road traffic accident the results were 14(70%) excellent and 2(10%) good. 2 patients (10%) fell down the results were 1(5%) excellent and 1(5%) good. 2 patients (10%) were victims of crush injury the results were 1(50%) excellent and 1(50%) good. (pvalue 0.09)The outcome at 6 months according to interval between the date of injury and date surgery; there were 16 patients (80%) operated on within 2 weeks the results were 14(70%) excellent and 2(10%) good. And 4 patients (20%) operated on more than 2 weeks the results were 2 (10%) excellent and 2(10%) good. (p-value 0.02)The outcome at 6 months according to Tile‟s type; there were 4 patients (20%) with type B the results were 3(15%) excellent and 1(5%) good. There were 16(80%) with type C the result were 13(65%) excellent and 3(15%) good. (p-value 0.04)The outcome at 6 months according to associated injury; there were 14 patients (70%) not associated with other injury the results were 12(60%) excellent and 2(10%) good. There was one patient (5%) had lower limb fracture the result was excellent. There were 2 patients (10%) with head injury the results were 1(5%) excellent and 1(5%) good. There were 2 patients with abdominal injury the results were 1(5%) excellent 1(5%) good. There was 1 with acetabular fracture the result was (5%) excellent. (p-value 0.06)Table 4. Use of walking aid at 2 weeks post-operative; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
Table 5. The outcome at 3 months according to age group; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
Table 6. The outcome at 3 months according to sex; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
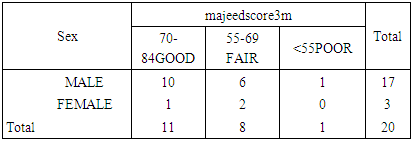 |
| |
|
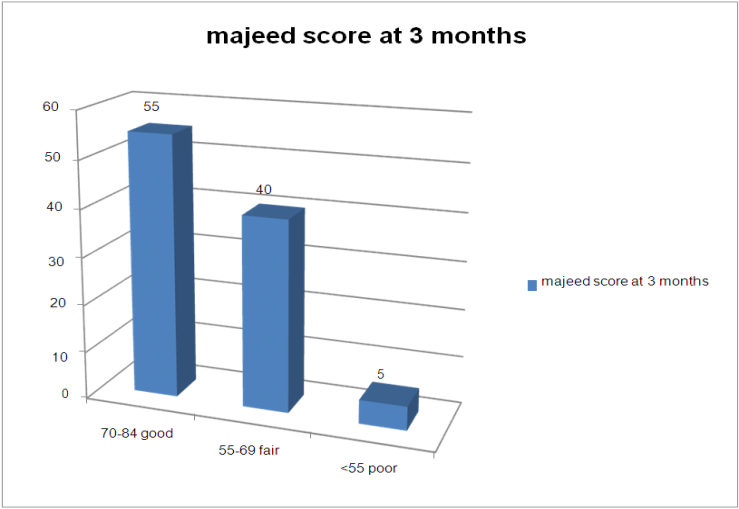 | Figuer 6. Majeed score at 3 months post-operative; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
Table 7. The outcome at 3 months according to occupation; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
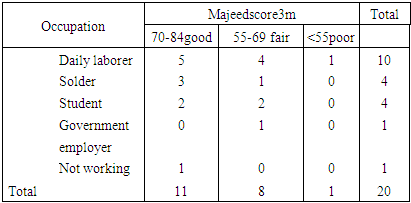 |
| |
|
Table 8. The outcome at 3 months according to M.O.T; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
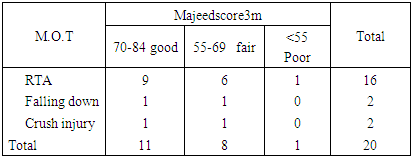 |
| |
|
Table 9. The outcome at 3 months according to interval between the injury and surgery; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
Table 10. The outcome at 3 months according to Tile‟s type; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
Table 11. The outcome at 3 months according to associated injuries; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
Table 12. The outcome at 3 months according to post-operative reduction on x-ray; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
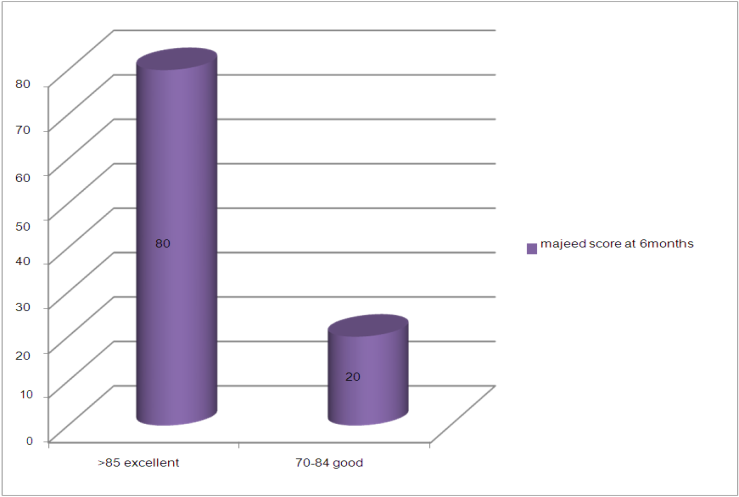 | Figure 7. Majeed score at 6 months post-operative; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
Table 13. The outcome at 6 months according to occupation; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
Table 14. The outcome at 6 months according to age group; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
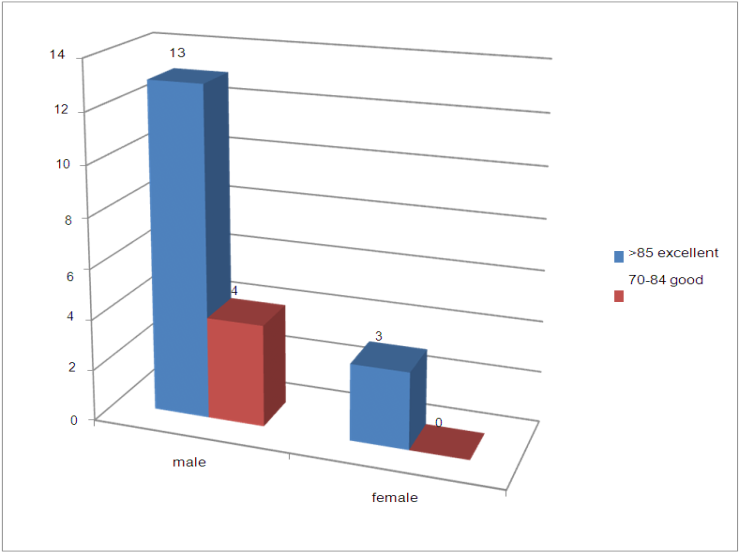 | Figure 8. The outcome at 6 months according to sex; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
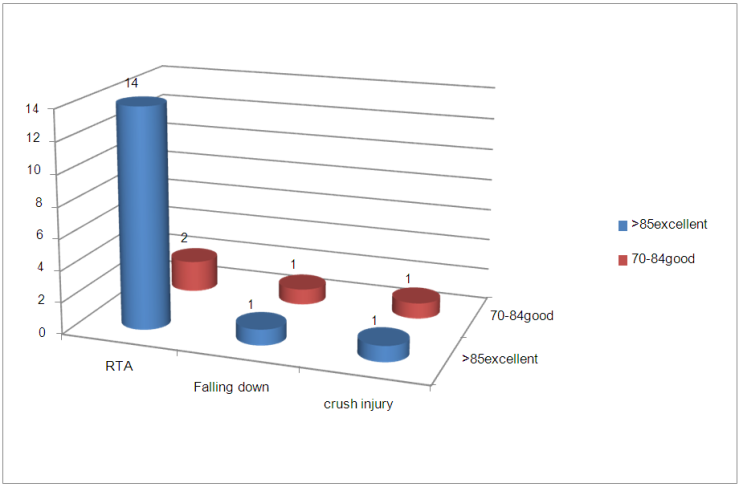 | Figure 9. The outcome at 6 months according to M.O.T; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
Table 15. The outcome at 6 months according to interval between the injury and surgery; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
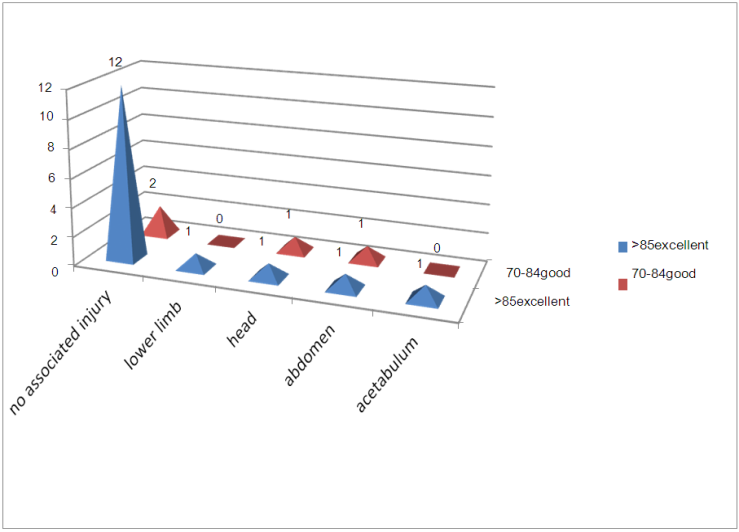
The outcome at 6 months according to post-operative reduction on x-ray; there were 6 patients (30%) with excellent reduction the results were 5(25%) excellent and 1(5%) good. There were 13 patients (65%) with good reduction the results were 10(50%) excellent and 3(15%) good. There was one patient with fair reduction the result was (5%) excellent. (P-value 0.03)Table 16. The outcome at 6 months according to Tile‟s type; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
 | Figure 10. The outcome at 6 months according to associated injuries; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation |
Table 17. The outcome at 6 months according to post operative reduction on x-ray; Outcome of plate fixation of the sacroiliac joint dislocation and fracture dislocation
 |
| |
|
4. Discussion
In our study the sample size was 20 patients (21 joints). The mean of age is 35 years with maximum number of patients in the age group 15-30(11-55%) were studied. This group represents the more active and productive classes of population. In this study the age group 15-30 has the best outcome (72% good) at 3 months post-operative and (90.9% excellent) at 6 months post-operative compared to other age groups because their post-operative reduction was excellent and good in 90.9%, most of them 90.9% had no associated injury and 90.9% operated within 2 weeks. 17 patients were male and most of them were daily laborer. The male gender has better result than female at 3 months and 6 months.In contrast to K. Mardanpour, et al. [13] said age and sex did not influence on clinical outcome.The majority of the sacroiliac injuries in this study were due to R.T.A (80%), the same result was shown by M Elmanawy et al [12].Early post-operative (within 2weeks post-operative) there were no complication on all the patients while K. Mardanpour, et. al. [16] reported Malposition (2.6%), Deep wound infection (10.5%), Lateral cutaneous nerve of thigh injury 10.5%. and M Elmanawy et al [15] reported 40% complications included posterior pelvic pain in one (10%) patient, superficial infection in one (10%) patient, foot drop in one (10%) patient, and pelvic tilt in one (10%) patient.In this study the Majeed score at 3 months post-operative was good in 11 (55%) patients, fair in 8 (40) patients and was poor in one (5%) patient, while at 6 months post-operative the Majeed score was excellent in 16 (80%) and good in 4 (20%). and this correspond with as Cao QY1 et al [11] result.The Daily laborer had the best result at 3 months post-operative (P-value 0.08) and at 6 month post-operative (p-value 0.06) this was due their post-operative reduction was 100% good, 75% of them had no associated injury and operated within 2 weeks compared to other occupations. In my knowledge no literature explains this.The victims of R.T.A had the best result at 3 months (p-value 0.06) and at 6 months (p-value 0.09 ) and this due to their post-operative reduction was excellent 76 and good in 93.7%, most of them (68.7%) had no associated injury and most of them (87.5%) operated within 2 weeks. And this statistically not significant. In my knowledge no literature explains this.The interval between the injury and operation significantly affect the outcome in this study, 16 (80%) operated in less than 2 weeks the outcome at 3 months was good in 9 patients (p-value 0.001) and at 6 months was excellent in 14 patients (pvalue 0.02) and this agreed with M Elmanawy et al [12]. and this statistically and clinically significant.Tile‟s type C had the best result at 3 months (p-value 0.07) and at 6 months (p-value 0.04) and this result was due to the majority (93.7%) of them had excellent and good post-operative reduction, (81.2%) had no associated injury and (87.5%) were operated within 2 weeks in contrast to K. Mardanpour, et al. [13] the result in type B were better than type C.The study revealed that the associated injury influence the outcome at 3 months (p-value 0.03) and 6 months(p-value 0.06) not influence the outcome but may delay the initiation of rehabilitation, and this due to early operation.In this study the post-operative reduction significantly influences the outcome at 3 months (p-value 0.001) and 6 months (P-value 0.03). And this statistically and clinically significant. This agreed with K. Mardanpour, et al. [13].The results progress with the time, most of the patients at 3 months postoperative scored good result and at 6 months post-operative scored excellent results and this agreed with Cao QY1 et al [14] results and K. Mardanpour, et al. [13] results.
5. Conclusions
These injuries are the result of high-energy trauma, which places patients at risk of multiple life-threatening injuries.The fixation of SI joint with plate is an effective, safe procedure and has good results and can use as an alternative to SI screw.Early surgery for unstable pelvic fracture and early rehabilitation give the best results.Functional outcomes of unstable pelvic fracture following surgical treatment are extremely encouraging.The age of the patients significantly influence the outcomes. p-value 0.02Tile‟ type C showed the best outcome with plate fixation of SI joint. p-value 0.04The associated injury influence the outcome at 3 months (p-value 0.03) and 6 months (p-value 0.06) not influence the outcome.
6. Recommendations
We recommend early surgery for unstable pelvic fracture and early rehabilitation.Open plating of SI joint is safe and effective can used when difficulty of closed reduction of SI joint dislocation and when there is poor imaging facilities in the theater.We need more studies to increase the number of patients and for prolong period of follow up.
References
| [1] | Yang J1, Cheng L, Li K. Epidemiological investigation of pelvic fracture in 9 third-tier hospitals in 5 cities in Hunan. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2014 Mar; 39(3): 301-6. doi: 10.11817/j.issn.1672-7347.2014.03.013. |
| [2] | Ertel W, Keel M, Eid K, et al. Control of severe haemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. J Orthop Trauma 2001; 15: 468–74. |
| [3] | Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma. J Trauma 1989; 29: 981–1000. |
| [4] | Simpson LA, Waddell JP, Leighton RK, Kellam JF, Tile M. Anterior approach and stabilization of the disrupted sacroiliac joint. J Trauma. 1987 Dec; 27(12): 1332-9. |
| [5] | Internal fixation for unstable pelvic fracture Madhat Mohammed Mahdi] Bas J Surg, September, 17, 2011, 58. |
| [6] | Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988; 70: 1–12. |
| [7] | Leighton RK, Waddell JP. Techniques for reduction and posterior fixation through the anterior approach. Clin Orthop Relat Res. 1996 Aug; (329): 115-20. |
| [8] | Borrelli J, Koval KJ, Helfet DL. The crescent fracture: a posterior fracture dislocation of the sacroiliac joint. J Orthop Trauma 1996; 10: 165–70. |
| [9] | Borrelli J Jr, Koval KJ, Helfet DL. Operative stabilization of fracture dislocations of the sacroiliac joint. Clin Orthop Relat Res. 1996 Aug; (329): 141-6. |
| [10] | Rockwood and Green's Fractures in Adults, 6th ed. |
| [11] | Cao QY1, Wang MY, Wu XB, Zhu SW, Wu HH; Trans-sacroiliac joint with plate via the anterior approach in management of posterior pelvic injuries. Zhonghua Yi Xue Za Zhi. 2008 Apr 1; 88(13): 898-900. |
| [12] | M Elmanawy, Samir A Elshoura, Salah A Youssef, Fathy H Salama MD. Treatment of sacroiliac joint disruption with anterior stabilization. The Egyptian Orthopaedic Journal. 2015; 50(1): 45-50. |
| [13] | Kaykhosro Mardanpour, Mahtab Rahbar. The functional outcome of surgically treated unstable pelvic ring fractures by open reduction, internal fixation. Molecular Pathology Research Center, Kermanshah University of Medical Sciences, Kermanshah, Iran Received: 15 Nov 2010 Revised: 15 Jan 2011. Accepted: 6 Feb 2011. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML