-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2020; 10(1): 1-11
doi:10.5923/j.cmd.20201001.01

Outcome of Pin Tract Care in Sudanese Patients Treated with Ilizarov
Azer Abbas, Mohamed Hamid Awadelseid
Departement of Orthopedic Alazhary University, Khartoum, Sudan
Correspondence to: Mohamed Hamid Awadelseid, Departement of Orthopedic Alazhary University, Khartoum, Sudan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

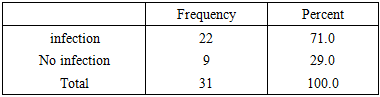
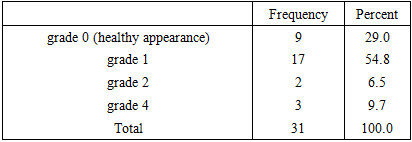
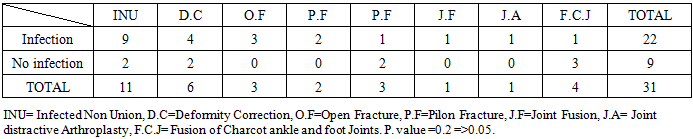
Background: Ilizarov introduced recently in Sudan for treatment of major devastating limbs injuries, correction of complex deformities, lengthening, infected nonunion, joint fusion and some other conditions. The result seems reasonable but Pin tract infection has always been the main drawback for use of these frames. And this fact necessitates defining and evaluates our current protocol and calculates the related incidence rate of pin tract infection. Methods: A descriptive, prospective hospital based study of the outcome of pin tract care for patients who were treated with Ilizarov for different indications in north Khartoum hospital over a period of two years from December 2016 to December 2018, data was collected by questionnaires and analyzed by SPSS. Result: 31 consecutive patients underwent Ilizarov frame application, for different indications, in north Khartoum hospital, involve 19 male and 12 female, the Minimum age was 5 years and maximum age was 60 years (mean age 32.5 years), minimum Ilizarov application period is 5week and maximum Ilizarov application period is 35 week (mean 20 week ) pin tract infection rate is (71%), the infection is superficial (86.36%) in the majority of infected cases involving shanz screws more frequent than smooth wires and located in the metaphysis more than the diaphysis. Conclusion: Ilizarov pintract infection, is a common complication associated with Ilizarov frame application and the incidence rate was 71%, most of infection is superficial and this will not plague the device. our current local protocol is valid in minimizing the incidence of pin tract infection and reducing the magnitude of the problem.
Keywords: Pin tract care, Sudanese patients, Ilizarov
Cite this paper: Azer Abbas, Mohamed Hamid Awadelseid, Outcome of Pin Tract Care in Sudanese Patients Treated with Ilizarov, Clinical Medicine and Diagnostics, Vol. 10 No. 1, 2020, pp. 1-11. doi: 10.5923/j.cmd.20201001.01.
Article Outline
1. Introduction
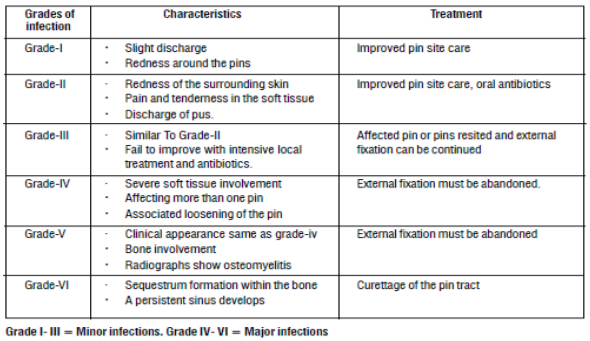
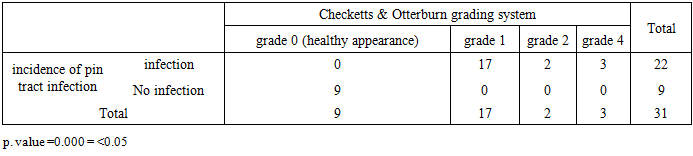
- The Ilizarov recently introduced in Sudan for treatment of devastating injuries, correction of complex deformities, lengthening of long bones, definitive management of infected nonunion, joint fusion when the use of internal devices is prohibited and many other conditions.Ilizarov is an external circular fixator, the structure of the frame include simply the presence of shanze screws, smooth wires and outer rings fixator. The procedure include a percutanouse insertion of shanz screws, Connecting the segments of the bone to the outer rings, while the wires are passed percutaneously through the bone using a drill, and the protruding ends of the wires are attached to metal rings, which encircle the limb, and tensioned to enhance stability. Ilizarov is a very useful tool for many reasons, one of them is the modular design of the apparatus which allows the frame to be custom built for each individual patient, and that is in addition to circular nature of the frame which enhances the stability and evenly distributes the stress across the corticotomy sites and the distraction gap or over the compressed fracture site in cases of fractures or particularly infected non united fractures. Moreover, the structure and strength of the frame allows weight bearing throughout the period of treatment, which is beneficial to the patient, both in terms of day to day mobility and helping to build muscle strength and prevent joint stiffness, additional more unique surgical advantage, is the gain from less invasive technique, when the frame is applied to the limb, in trauma setting, only wires and shanz screws fix the bones to the rings, and no more skin incisions are made, which in turn reduces the risk of bleeding, infection, and damage to the surrounding soft tissues. In spite of all these advantages, pin tract infection has always been the main drawback for use of these frames. As the infection is a common problem around pin sites, and this is why many efforts, were carried out, to define the pin tract infection, categorized them into certain stages according to the degree of the infection, setting a certain criteria for each stage and appropriate line of action, Checketts and Otterburn system is used widely, for this purpose [10] and is adopted in this study, in literature there is general agreement considering the problem common [1,2,3,10], but many answers for any question wondering about how common is the problem and this is why different numbers or figures which considered as incidence rate was set by different limb reconstruction surgery centers, appear so variable, similar diversity is also noticed in operative techniques and postoperative care protocols [12].As different protocols may set a different incidence rates, this study, is trying to determine the incidence rate of pin tract infection, in order to evaluate our current local protocol, which has a certain operative technique, and certain postoperative care.There is global agreement in the literature, that the early symptoms and signs of pin tract infection are, pain or tenderness around the pin in an area that was previously not tender, erythema and white, yellow or green cloudy discharge from the pin site, while fever and malaise come as a late features. [1,3,4,10,12], but other state that at presentation, additional features of bacterial endocarditis may be seen or even features of septic shock if the pin site infection is overlooked [2].Many classification systems was adopted to deal with this condition with concomitant recommended management for each category, the most wide adopted one is the Checketts-Otterburn’s grading system [10] for evaluating, the degree of pin-site infection, during the period of mangment or when the fixator was removed. According to this system. Grade 1 pin-tract infection is characterized by slight discharge and redness around the pins that requires only local treatment. Grade 2 infection is indicated by redness of the surrounding skin, tenderness in the soft tissues and sometimes discharges of pus, Infections of this type resolve with local care and oral antibiotics. Grade 3 infection is similar to grade 2 infection but fails to improve with intensive local treatment and antibiotics. The infection resolves when the involved pin or pins are removed and repositioned, after which it is possible to continue use of the fixator. Grade 4 infection is characterized by severe soft-tissue involvement that affects more than one pin site and fails to respond to local treatment and oral antibiotics. it is necessary to remove the affected pins and to abandon use of the external fixation device. The clinical appearance of Grade 5 infection is the same as that of grade 4 infection, but there is radiographic evidence of osteomyelitis. It is necessary to remove the affected pins and to abandon use of the external fixation device, Grade 6 infection is characterized by the formation of a sequestrum within the bone and the development of apersistent sinus. Additional surgery is required to eradicate the problem. Grades 4, 5, and 6 are indicative of major infection. Whereas, grade 1,2,3 are considered as superficial infection, in other words cellulitis or a localized form of osteitis (table 1).
|
|
2. Patients and Methods
- This is a descriptive, prospective, hospital based study of the outcome of pin tract care following Ilizarov frame application. This study was carried out in North Khartoum Hospital accidence and emergency department, which receives patients, through the whole 24 hours of the day, with 15 beds for short stay, and 45 beds for long stay. all patients were initially seen by trauma team, then referred to orthopedics team which consisted of an orthopedic surgeon, registrars, house officers. All cold cases, were referred from different orthopedics units in the same hospital or from different hospitals directly to outpatient department (referred clinic), which was held once weekly.The study population consisted of all patients who were treated with Ilizarov in tow -years period from December 2016 to December 2018. Patients were included if they had completed treatment and the fixator had been removed. Patients were excluded if the fixator had not been applied at our unit or the records were insufficient with regard to the required data, inclusion criteria’s as follow: All patients who underwent, Ilizarov application in our unit for different indications, for any sex and age groups, for a period not less than 5 week, as definitive treatment, done by the same senior orthopedic surgeon, who was following the same operative techniques, and same post operative care all patients who came on weekly basis for follow up throughout the period of management till she / he underwent removal of the frame in our operating theater, followed for another two weeks for any evidence of residual infection, all patients who meet these criteria’s and signed an informed consent to participate in this study were included. Exclude patients who underwent Ilizarov application outside our unit, or referred to us for revision or not done by the same orthopedic surgeon in our units, or by other operative technique, or did not follow the same postoperative after care, or lost during follow up, or underwent removal outside our operating theater, that in addition to not agreed to participate in this study, they were excluded.After, the objectives were explained, an informed-consent form was signed and patients were admitted to the study, then after that we used total coverage sampling technique in a consecutive fashion.Initial information regarding the personal data, main presented condition, and the main indications for surgery was taken from all Patient who agreed to participate in the study and filled in specific part in the questioners. Iodine 10% soaked squares of gauze were placed around each pin site and a kling bandage was then used as an occlusive dressing around all the pin sites. The dressing was left undisturbed for 48 hours. Thereafter each pin site was cleaned with normal saline initially then with Iodine 10% soaked squares of gauze and light Iodine 10% gauze dressing was applied. All patients were trained to do this kind of dressing, observed and corrected, after they learn the procedure then they discharged. Patients were instructed to clean the pin sites with those methods every two days.The signs and symptoms of a pin site infection were explained to the patient and relative (pain, erythema, tenderness, discharge and systemic manifestations). Patients were evaluated weekly by the authors during the whole period of treatment according to Checketts and Otterburn system investigating and treating pin tract infection, in another word at each visit a record was made of the condition of the pin sites, the location of each infected pin site was noted, and the type of pin that got infection After removal of all pins, pin sites left covered with iodine 10% for another week, then after pin site left uncovered patient followed up for another 2 week to make sure that there was no evidence of residual infection and patients reports satisfaction was recorded. Data was collected by the authors, from admission sheets, postoperative notes discharge cards and direct clinical interviews and filled in questionnaires, which was consisted of the following blocks; personal data, the presented condition, the main indication for Ilizarove, component of the operative technique, Contains of the construct, routine pin care, the frequency of pin care, the type of solution used, Treatment period per weeks, incidence of pin tract infection, the main presented symptom, the grade of pin tract infection according to Checketts and Otterburn system the degree of pin tract infection, the type of pin involved the number of the pins that got infection the location of the pin that involved, the treatment options that responded to, incidence of pin loosening and patients report satisfaction.At the end of the study data was analyzed, figures and tables of frequencies were layout, chi-square test was used, to test the relationship between dependant variables and the independent variable; P value which was less than 0.05 considered as statistical significance value. This analysis was performed using the statistical package for social sciences (SPSS).
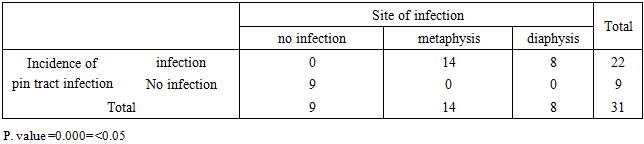
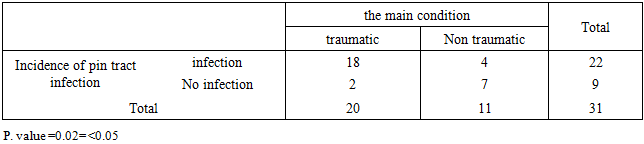
3. Results
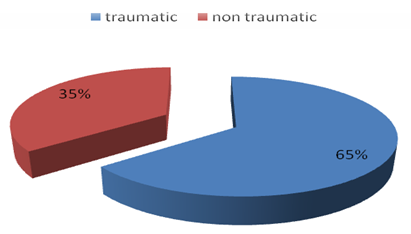
- 31 consecutive patients underwent Ilizarov frame application; they were 19 males and 12 females (figure 1) with mean age of 32.5 years (range 5–60 years) (figure 2). No patient was lost to follow-up, Infection rate was assessed as a percentage of the number of pin sites as well as a percentage of the number patients.
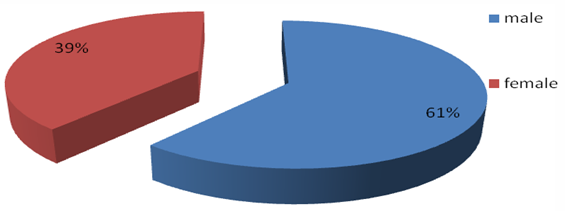 | Figure (1). Sex Distribution |
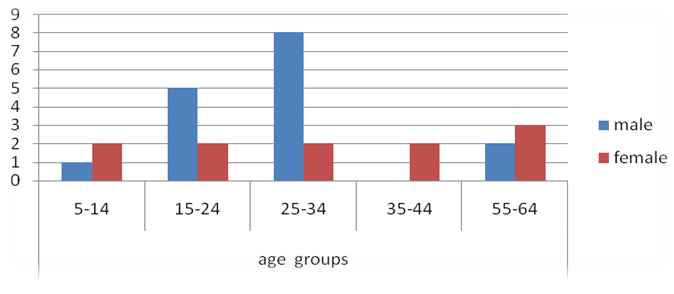 | Figure (2). Age groups and sex distribution |
|
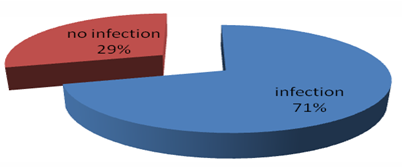 | Figure (3). Incidence of pin tract infection |
|
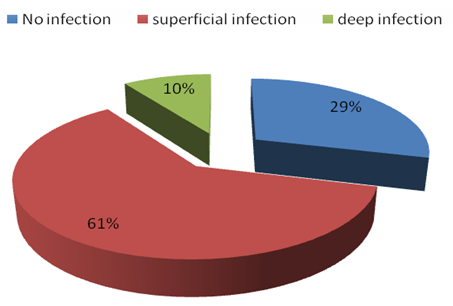 | Figure (4). The degree of the infection versus no infection |
|
|
|
 | Figure (5). The main presented condition |
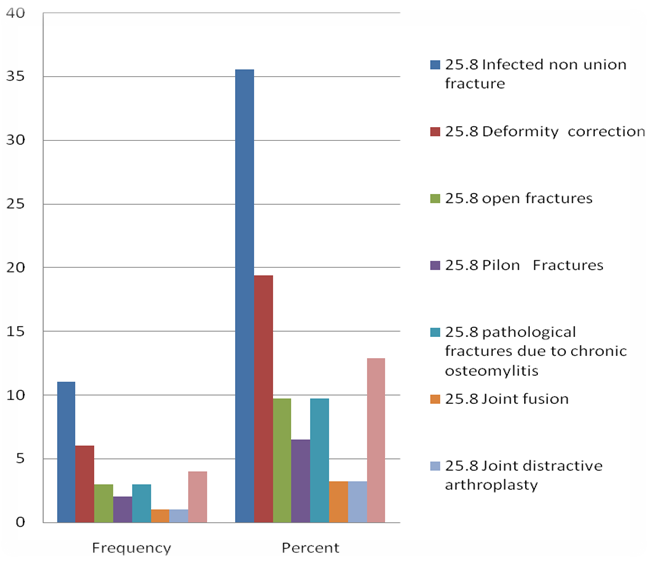 | Figure (6). The indications for the use of ilizarov in this study |
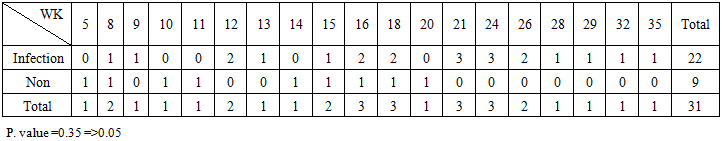 | Table (8). The relationship between; the frequency of pin tract infection and The treatment period (per weeks); Crosstabulation |
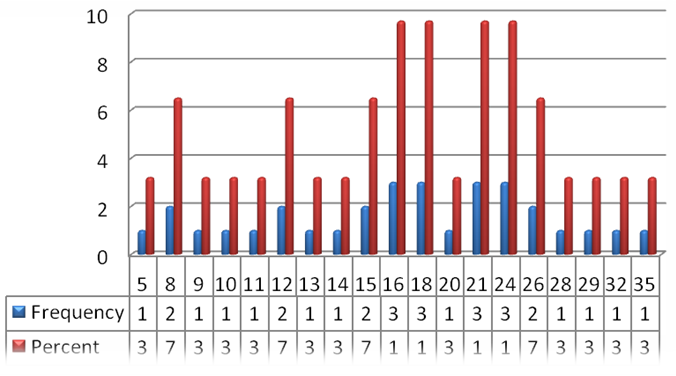 | Figure (7). Durations of treatment period per week |
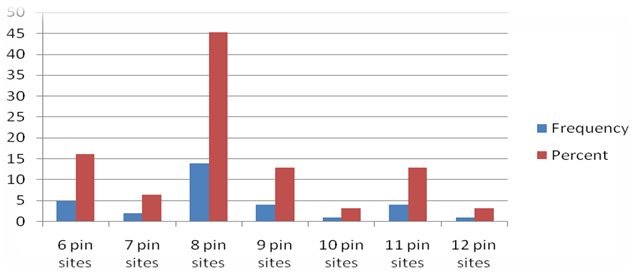 | Figure (8). The numbers and percentage of the pin sites per difrenent frame constructions |
|
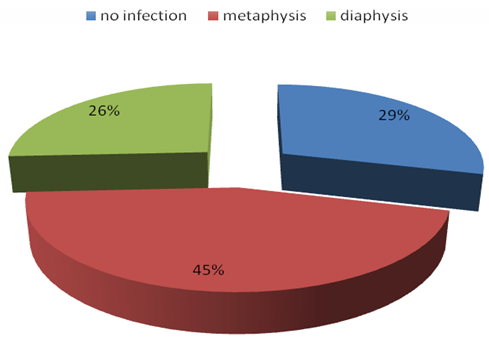 | Figure (9). The site of infection |
|
|
|
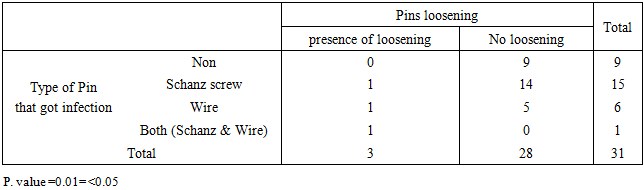
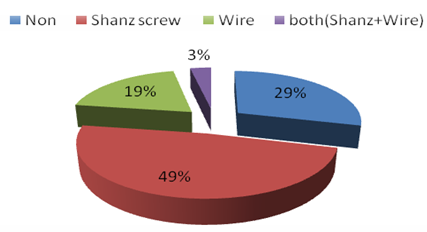 | Figure (10). The type of pins which get infected |
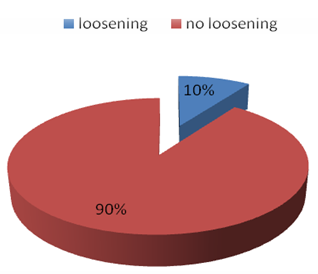 | Figure (11). Incidence of loosening |
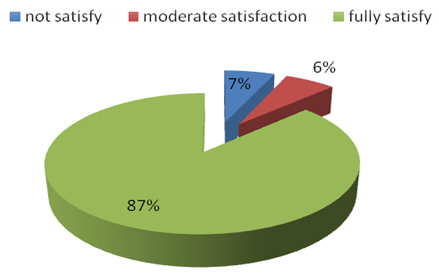 | Figure (12). Patients satisfaction |
4. Discussion
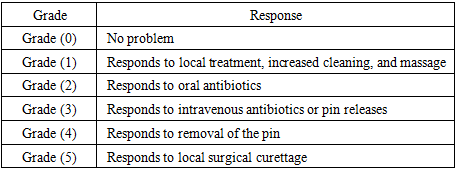
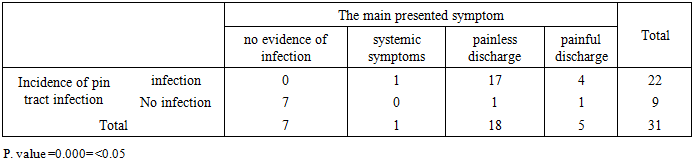
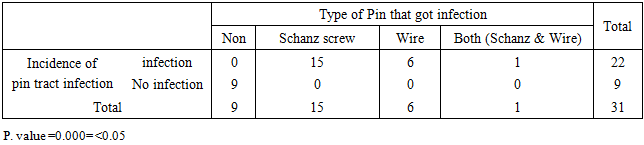
- Pin tract infection is the most common complication associated with Ilizarov frame application; its rate varies. Many different institutions reported many different protocols for preventing and treating pin tract infections. The protocols for the care of pin sites are often derived from the preference of the surgeon, habit, consensus or inappropriate conclusions from the basic principles of wound care. There is little scientific evidence to support one technique over another.But however, the diversity was, there is a global agreement in the literature, that pin tract infection is the main drawback following, Ilizarov frame application, we agreed with, Moroni et al 2002 [16], who stat that pin tract infection is a common complication with the use of Ilizarov frames and the incidence rate range from 11.3 to 100%, Our results compare favorably to published figures with an overall pin tract infection incidence rate of 71% (22 out of 31) was observed in this series.In an effort made to report the degree of the infection and treatment response, Schalamon et al 2007 [4], found that 94% of infections were mild and responded to local frequent dressing only or with antibiotic management. Piza et al 2004 [15], also reported that 75 % of their pin site infections were minor infections when using the Checketts–Otterburn classification. In our study we found that of the 22 patient who got the infection, 19 patients (86.36%) their infection was mildand they were responded to increased frequency of dressing and empirical oral antibiotic management. But we had 3 patients (13.63%) who developed, deep infection and they were responded to removal of the pin, surgical debridement of the pin sites. Valentin et al 2008 [2], found that, the rate of Schanz screw site infection (78%) was significantly (P<.05) higher than that of fine-wire site infection (33%), this study support our result, as we found that, Of the 76 Schanz screws, 17 Schanz screws (22.36%) got infection, while of the 91 wires, 8 wires (8.79%) got infection, so Schanz screw got infected more frequent than wires and the results were statistically significant (p. value 0.000), that in contrast to the opinion of, R. Rose 2009 [24] she found that, Schanz screw infection site was 6.3%; and wire site infection was 18.7%. Total pin site infection was 25% and periarticular pin site infections accounted for 13.6% and diaphyseal infections 1.36%., but also we found part of her result supporting part of our results, as we found that, Most of the infected pins were in the metaphyseal region, rather than diaphyseal region and the results were statistically significant (p. value 0.000), our results is also supported by the work of Ferreira et al 2012 [6], when they found that, soft tissue movement around a wire or pin leads to an increased risk for infection. Valentin etal 2008(2), also reported that pin tract infection has a certain clinical feature, which include,, pain and tenderness around the pin in an area that was previously not painful or tender, erythema, and, white, yellow or green cloudy discharge from the pin site, while fever and malaise come as a late features.In our study, we come across all these symptoms, and we follow the pattern of presentation of pin tract infection, in term of, what the prominent symptom that the patient complain of at presentation, and we found that, the pattern of presentation of the pin tract infection varies, in children less 15 years the main presented symptom, was systemic manifestations, all of them presented because of fever and malaise, and when the pin sites were inspected there was a clear evidence of pin site infection, in contrast this was not the case, in the rest of age groups, the majority of patients (60%) presented with painless pin site discharge without systemic manifestations, while 40% of the patients presented only with painful pin site discharge. Erythema as main concern was not presented at all, and considered as missing value in the analysis. Interestingly wefound these results, have statistically significant value (p. value 0.000).Bhattacharyya et al 2006 [9] found that, there were many classification systems adopted to deal with this condition; according to this and to the observation of Saw et al 2012 [1] when they mentioned that, Checketts and Otterburn's classification is most commonly used to evaluate the pin site infection, in regard to all of the above this classification was adopted in our study, and it was found to be, useful and reliable, in term of detailed description of each grade, and further recommendation of treatment and we found The relationship between, our recognition of pin tract infection and Checketts & Otterburn grading system, was of statistical significant value (P.value 0.000).According to Checketts & Otterburn grading system, we found that, 17 patients had grade one, pin tract infection, and they were responded to increase frequency of dressing, 2 patient had grade two, they were responded to increase frequency of dressing with seven days course of oral antibiotics, the other remaining 3 patients, who developed, deep infection, all of them had grade four, after removal of the infected pin and debridement of pin site, the infection was settle down.We think that, the operative techniques, had much to do with the incidence of pin tract infection, Davies et al 2005 [14] inspect two conflicting operative protocols, the Russian Protocol and the Britain protocol, both of them were widely used and have a recognized good reputation, they found that no one of these two protocols was superior in the outcome than the other, but the risk of pin-tract infection is lower if attention is paid to avoid thermal injury to the skin and bone in addition to avoidance of local formation of hematoma during surgery, in this regard we adhere to the recommendations which were set by Davies et al when they emphasized that any strategy for reducing pin site complications, must begin in the operating theatre.Wire and Schanz screw insertion should be as low energy and a traumatic as possible, with minimum damage to the skin, soft tissue and bone, in this concern, we found that, our operative protocol, was reasonable, as it consisted of, Non-touch handling of wires/Schanz screw, which ensured by the use of normal saline-soaked gauze to handle and manipulate wire /shanz, also we were accustomed to use the normal saline for cooling of drill bit, while pre-drilling before manual insertion shanz screw that in addition to manual advancement of the wires to the soft tissue, after they approached the bone, all of the patients included in this study were operated on, with the light of this protocol, In an effort to prevent or at least minimize this complication, through the door of pin loosening which may initiate or propagate, pin tract infection, and this is, why we agreed, also with Ferreira et al 2012 [6], when he stated that, If all surgical precautions were considered, we would get an optimal bone–pin interface, which can withstand the subjected force upon, with great expectation of formation of rigid bone-metal interface, rather than loose fibrous –metal interface, which can leads to increase motion at the fixator pin–bone interface, producing pin site irritation, loosening and infection.Parameswaran et al 2003 [3] mentioned that, pin tract infection decreases the stability of the pin–bone interface. Conversely, instability of the fixator pin–bone construct can lead to Schanz screws loosening and further infection, Pizà et al 2004 [15], mentioned that, there is a common misconception that pin loosening only results from pin tract infection when in actual fact pin loosening is often an isolated event from failure of surgical technique, resulting in pin tract infection. In our study we found that Of the 31 patients, 28 patients (90.3%) did not experience any pin loosening, while 3 patients (9.7%) did, and the infection was detected in all of these loose pins, and we found that, the relationship between the pin that got the infection, and the pin that got loosening, of statistical significance value (P. value 0.01).Many construct materials, and coating substances were suggested, assuming that they might offer an additional defending mechanisms, against the incidence of pin tract infection, this idea was very obvious, in the work done by Zheng et al 2009 [11] when they compared two forms of titanium-copper alloys (1% CU & 5% CU), with stainless steel and found that there was a dramatic decrease of pin tract infection, in titanium-copper alloys, as compared to stainless steel, but the main limitation of this study, been an animal models study and even the type of alloys which were suggested not present out the doors of these labs, in our study we used stainless steel, as many did, because of its availability and its mechanical properties in term of has an acceptable material stiffness, which proved enough optimal environment for bone healing, and in this regard we follow the recommendations of Ferreira et al 2012 [6] when they found that, the forces transmitted through the fixator device and the limb, is a function of the geometrical and mechanical properties of the fixator as well as the properties of the surrounding tissues and the fracture pattern, so the global stability is one of the major factors that can affect the incidence of pin tract infection, and not too far from this area (stability), the recommendations of Saithna et al 2010 [13], when they stated that, hydroxyapatite- coating pins, appears to be an effective method of reducing the incidence of pin loosening and infection and it was highly recommended, in leg lengthening reconstructive limb surgery, but we did not used hydroxyapatite- coating pins, partly because these type of pins are not available, in our areas that in addition to; the fact which recommend meticulous surgical techniques as mainstay, for stability, Our results regarding the associated incidence rate of pin loosening was of compared favorably to published figures with an overall pin loosening of 9.7%..To date, there is a lack of evidence available to demonstrate whether dressing should or should not be used in routine pin site care. The Cochrane review (Lethaby et al., 2008) [23]; supports this, suggesting that there are no studies that specifically focus on whether or not to use dressing. There were a handful of studies which involve dressings but these usually set out to measure the entire pin site care regime rather than this specific aspect. A study of note would be, (Davies et al. 2005) [14] Which suggested that pin site dressing should be used at all time, along with other several operative actions. Egol et al. (2006) [21] end their controversial paper with this statement: ‘we do not recommend additional wound care beyond the use of dry sterile dressing for pin-tract care after external fixation for the treatment of distal radial fractures’; but this study, however, was not a direct comparison between dressed pin sites and those which, left open to the environment. In review of earlier British Consensus, Timms et al. (2011) [12], advocated the use of dressing and advised that, a dressing that applies a small amount of pressure should be used, to prevent tenting of the skin along the pin and must kept continuously in place, while Carlo Camathias et al 2012 [28] conclude that routine pin tract care is unnecessary, in our unit we do agree still with, Davies et al, and Timms et al, and all patients involved in our study did dressing in regular basis, throughout the period of treatment, and our philosophy behind that, we think that, pin tract care is not a nonsense routine habit, but it is our mean to treat grade one and a good partner in treatment of grade two pin tract infection with oral antibiotic, that in addition to, some patient might got any type of (subclinical) superficial infection, and when they were already done the care, they were actually participated actively in the treatment of their ongoing infection before it got complicated and upgraded.The appropriate times to commence pin tract care, ranging from 24 h to 10 days, (Davies et al. 2005) [14], mentioned that, it was daily in, the British protocol and every seven to ten days in, the Russian protocol, (W-Dahl et al 2003) [22] found that, No difference between daily and weekly pin tract care in a randomized study of 50 patients. for us, we found, every 2days dressing, more reasonable and compliance for the patient, our patients report satisfaction, about the, nature and frequency of pin tract care record the following; 87% fully satisfaction, 7% non satisfy, and 6% moderate satisfaction.Various cleaning solutions are advocated in the literature, including, sterile water, normal saline, hydrogen peroxide, silver sulphadiazine, Povidone-iodine, isopropyl alcohol and chlorhexidine, [1,2,3,5,6,9,12,20], we are accustomed to train our patient to use normal saline as initial dressing solution, followed by formal dressing with 10% Povidone-iodine as a main cleaning solution, because, iodine has a wide range of bactericidal, antifungal, and some antiviral effect, while many studies had a serious concern of iodine, mainly about, its irritation effect to the skin, its corrosive effect to stainless steel pins, and cytotoxicity at cellular level of bone and soft tissue, as mentioned by Trigueiro et al 1983 [43], we found the work of Hiroyuki et al 2012 [20] of great value, when they explained that, iodine is a trace metal that already present in the body, as it is an essential component of the thyroid hormone, it is biologically safe because it can be excreted by the kidneys, if it was enter the circulation, and they also proved that it has no clinical cytotoxic effect, as implant treated with iodine, in arthroplasty field, showed an excellent bone ingrowth and ongrowth, around hip and tumor prostheses on radiographs that in addition to, relative sustainable bioavailability, as the amount of iodine on the external fixation pins remained about 20–30%, after one year later, in our study we did not had any patients in this series, presented with any sort of skin dermatitis, or any cytotoxic effect, in term of bone non union, or chronic non healed pin sites, even those who were treated because of pin site infection, they were responded well to the dressing with 10% Povidone-iodine itself.
5. Conclusions
- Pin tract infection, is a common complication associated with Ilizarov frame application and the incidence rate was 71%. Most of infection is superficial, and this will not plague the device. Shanz screws get infected more than wires and the infection was more frequently seen in metaphysal regions. Our current protocol is valid in minimizing the incidence of pin tract infection.
6. Recommendations
- The findings of this study were initially confirmed by, this prospectivestudy, but further confirmation is needed in the field of blind randomized controlled clinical trial, that enrolling, different operative protocols, different care methods, different type of solutions, and different care frequencies.This study layout the overall incidence rate of pin tract infection in series of patients who underwent Ilizarov for different indications but figuring out the incidence rate of pin tract infection in series of patients with specific condition are of great importance. Treatment of the literature diversity, regarding the issues of pin tract care and incidence rate can be initiated by conducting an international multi-center studies and meta-analysis, to determine the optimum, that in order to speak one languishes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML