-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2018; 8(3): 53-58
doi:10.5923/j.cmd.20180803.03

Does Intravenous Contrast Used in Computed Tomography Affect the Bone Mineral Density?
Naglaa Mostafa Elsayed1, 2, Mashael A. Esmail1, Elham K. Abdulsattar1
1Diagnostic Radiology Department, Faculty of Applied Medical Sciences, KAU, Jeddah, Saudi Arabia
2Diagnostic Radiology Department, Faculty of Medicine, Cairo University, Cairo, Egypt
Correspondence to: Naglaa Mostafa Elsayed, Diagnostic Radiology Department, Faculty of Applied Medical Sciences, KAU, Jeddah, Saudi Arabia.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

For providing information about bone mineral density (BMD) in computed tomography (CT), there is no specific technique to calculate it. BMD can be measured from the same routine abdominal examination of CT, for reducing the radiation exposure for the patient. The way of measuring BMD value is by using the region of interest (ROI) in the lumbar vertebral body (L1-L3) for demonstrating the Hounsfield unit (HU). Measuring BMD by quantitative computer tomography (QCT) is more accurate than the traditionally known dual energy x-ray absorption (DEXA). BMD is assessed to detect early osteoporosis to avoid any possible complications, the most important of them is bone fractures. Aim of work: The purpose of this study is to define how much the intravenous iodinated contrast used in CT can affect the reading of (BMD). Patients and methods: A retrospective study was carried out to assess BMD in the lumbar spine before and after injecting contrast media in the three phases; arterial, venous and portovenous, by using ROI during abdominal CT. The study population consisted of 200 participants (102 females and 98 males); ranging in age from 5 to 88 years; with the mean age 55 ± 17 years. Results: Normal BMD was seen in 167 patients, while 33 patients showed osteoporosis. Comparing the BMD in the pre and post contrast injection phases, significant increase in the BMD reading was detected in the portovenous phase in all patients with p value < 0.01. There was an inverse correlation of the changes that noted in the BMD with age, meaning the older the patient, the less the increase in the BMD reading. This was noticed mainly in the venous phase. Conclusion: This research proves that the BMD reading increases after IV contrast injection in the CT study of the abdomen in the three post contrast phases, but more in the portovenous phase. This should be taken into consideration before diagnosing normal or abnormal bone density depending on BMD reading in these phases.
Keywords: Computed Tomography, BMD, Osteoporosis, Iodinated Contrast
Cite this paper: Naglaa Mostafa Elsayed, Mashael A. Esmail, Elham K. Abdulsattar, Does Intravenous Contrast Used in Computed Tomography Affect the Bone Mineral Density?, Clinical Medicine and Diagnostics, Vol. 8 No. 3, 2018, pp. 53-58. doi: 10.5923/j.cmd.20180803.03.
Article Outline
1. Introduction
- Osteoporosis is the most common form of metabolic bone disease. About 200 million people are affected all over the world. It is defined as a reduction in the bone density that may cause bone fractures with minimal traumas [1, 2].About 50% of women and 20% of men are affected by osteoporosis. It is four times more common in females than in males, but males tend to have more osteoporosis-related complications than females. Men are less affected because they have more peak bone density in adulthood which declines in the menopause in females. [3, 4, 5]. Patient with an increase in age is more vulnerable to have an osteoporosis with expected decrease in the BMD [6, 7].Bone mineral density can assess the osteoporosis so it can be detected prior to the occurrence of any fractures. The quantitative computer tomography (QCT) is the standard technique used for estimating BMD from lumbar vertebrae and the proximal femur [8].The QCT has grown and become an established standard technique for assessing skeletal condition, response to therapy for osteoporosis and metabolic bone disease. Quantitative computer tomography technology uses higher radiation dose than DEXA but it is the most sensitive technique available to assess osteoporosis. However, DEXA is still used for the diagnosis of osteoporosis. Quantitative computer tomography is a unique type of modern noninvasive technique of measuring BMD. It can measure true three-dimensional BMD instead of the area (two-dimensional) and it can measure the cortical, trabecular or integral (cortical plus trabecular) bone in any part of the body. It is more accurate in patients with extreme obesity or low body mass index [9,10].The purpose of this research is to study the possible effect of intravenous contrast media on the BMD of the lumbar vertebrae by using CT. It depends on the measurement of the HU on routine abdominal examination before and after contrast media injection.
2. Subjects and Methods
2.1. Study Plan
- A retrospective study was done to assess the difference between BMD reading before and after IV contrast media injection. An ethical approval was obtained from the research ethics committee, and a written consent was taken from all participants.
2.2. Subjects
- The study population consisted of 200 participants (102 females and 98 males); ranging in age from 5 to 88 years, with the mean age 55 ± 17 years. Data was collected from the PACS system of King Abdul-Aziz University Hospital (KAUH), CT department.Exclusion criteria: patients with apparent lumbar spine deformity or malignancy or history of damaging trauma to the lumbar spine in addition to neonates were excluded.
2.3. Methods
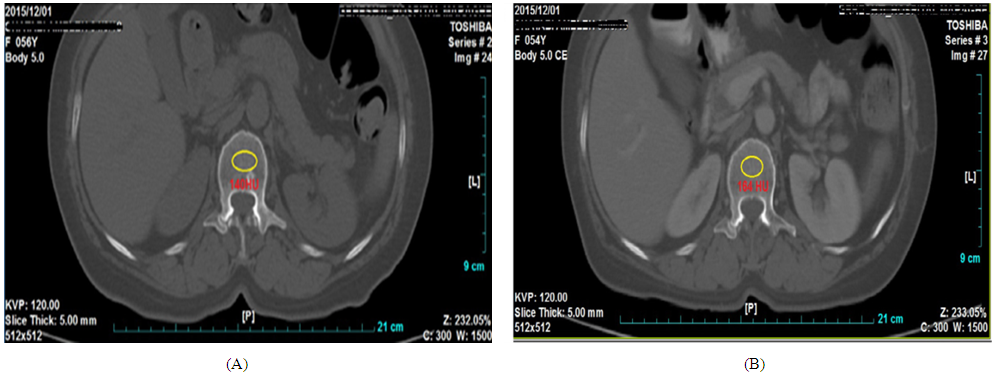
- CT examinations were accomplished with (Siemens, multiple-detector computed tomography (MDCT). The parameters used were; 160 (mA) milliampere, 120 (Kvp) kilovoltage peak, 5mm slice thickness and two-dimensional axial image). The concentration of the iodinated contrast media was 320 mg/ml, and every patient received 1.5 ml contrast / kilogram of body weight. The average BMD was taken from the lumbar vertebrae L1, L2 and L3 before and after contrast injection in the arterial, portal and venous phases. The ROI was used to measure the BMD as shown in figure 1. The trabecular BMD was classified into normal and osteoporosis depending on Felsenberg classification, based on the following HU values:• Osteoporosis < 80 mg/cc• Osteopenia < 120 mg/cc• Normal BMD > 120 mg/cc• Very high fracture risk < 50 mg/cc. [11]
2.4. Statistical Analysis
- The program used in this study was statistical Package for Social Science (SPSS 17.0) for Windows. Paired values for pre and post contrast values were compared by paired t-test. Correlations between difference of pre and post contrast values and other continuous parameters were done using Pearson correlation. In all tests, p value was considered significant if less than 0.05.
3. Results
- The research sample included 200 patients; 102 females and 98 males with the mean age 55 +/- 17 years. The largest percentage of patients (40.5%) was seen in the age group (40: 60 years), while the lowest percentage was in the age groups < 20, and > 80 years (3.5% each). Twenty-six % of our participants had hypertension and 25 % were diabetics.Normal BMD was seen in 167 patients (83 females and 84 males) (figure 2), while 33 patients showed osteoporosis (19 females ranging in age from 33 – 85 years, and 14 males ranging in age from 52 to 88 years), with the average measured BMD was < 120 mg/cc (figure 3).By comparing the pre and post contrast injection in the three phases, we found significant increase in the BMD reading in the three phases, but more evident in the porto venous phase in all patients with p value < 0.01(Figures 4, 5 and 6).We also noticed inverse correlation of the changes that noted in the BMD with age, meaning that the older the patient's age, the less the increase in the BMD reading. This was noticed mainly in the venous phase (Tables 1, 2). This correlation is also noticed in the female participants more than in males.
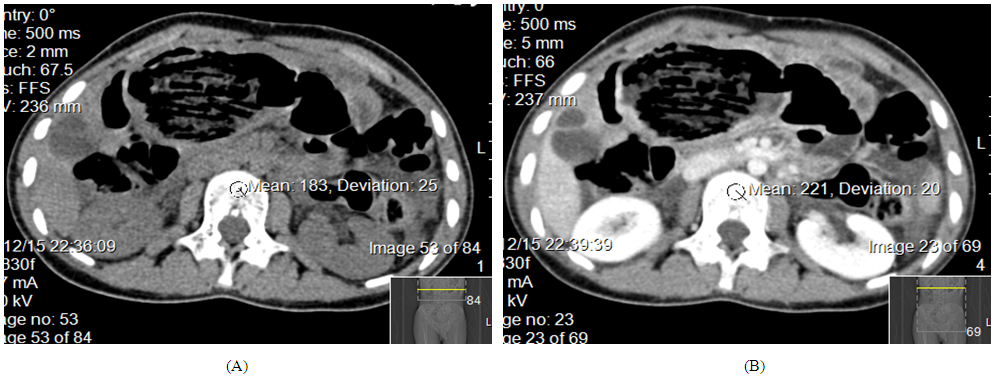 | Figure 2. CT abdomen, axial, precontrast image (A) showing HU values = 183 which increased to 221 in post contrast image of the same patient (B) denoting normal BMD |
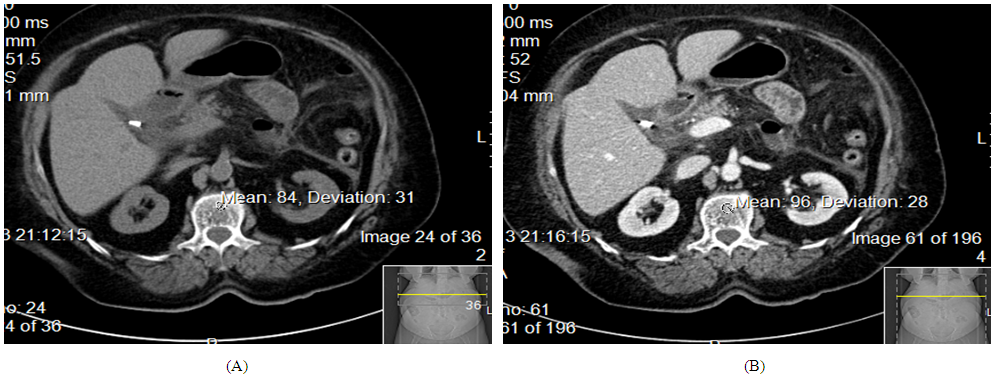 | Figure 3. CT abdomen, axial cuts, precontrast image (A) showing HN unit = 84 denoting osteoporosis with mild increase in the HN unit reading after contrast injection (B) of the same patient = 96 |
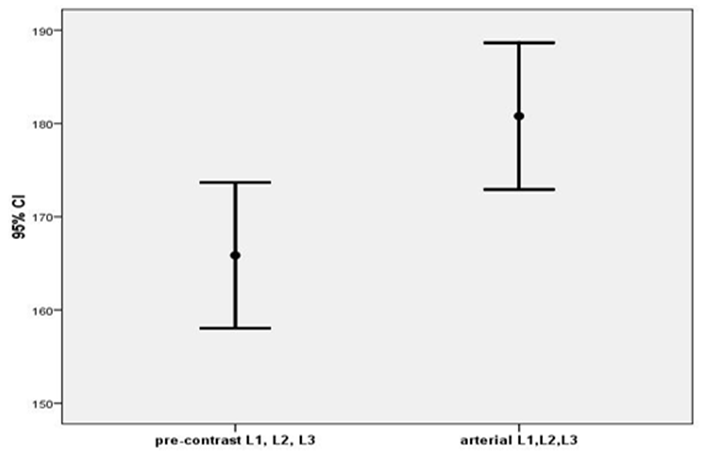 | Figure 4. Comparison between BMD in pre-contrast and arterial phase in all patients shows increase BMD in the arterial phase with the p value < 0.01 |
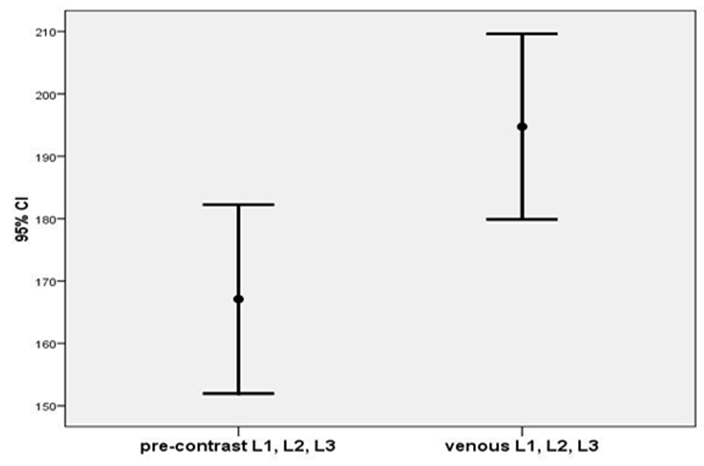 | Figure 5. Comparison between BMD in pre-contrast and venous phase in all patients shows increase BMD in the venous phase with the p value < 0.01 |
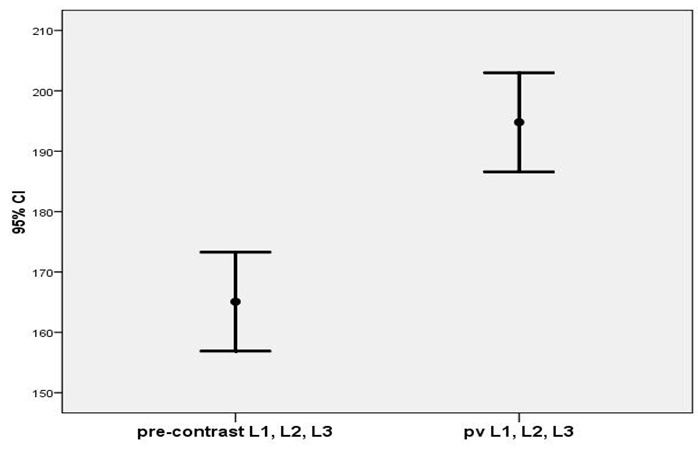 | Figure 6. Comparison between BMD in pre-contrast and portovenous phase in all patients shows significant increase BMD in the portovenous phase with the p value < 0.01 |
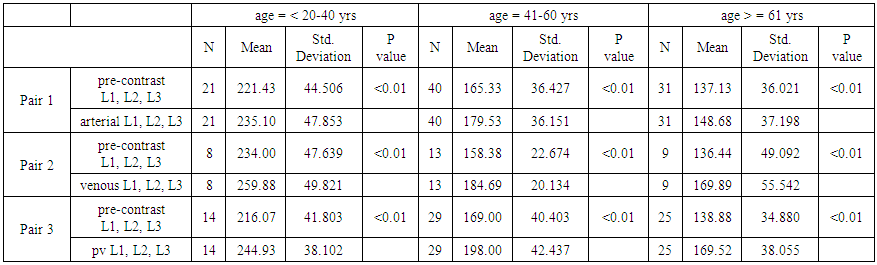 | Table 1. Comparison of pre and post values in males in different age groups |
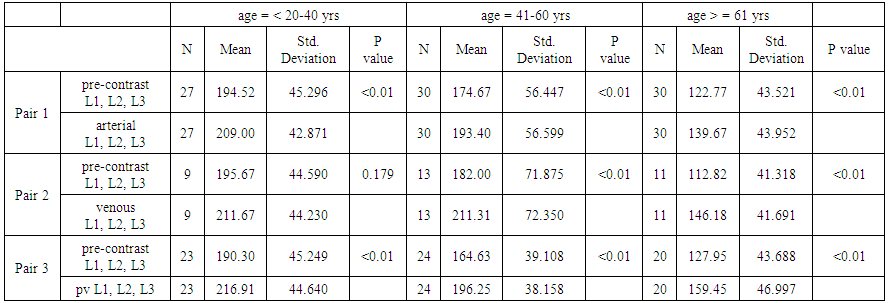 | Table 2. Comparison of pre and post values in females in different age groups |
4. Discussion
- As far as we could search, most previous studies studied the effect of IV contrast injection in either the arterial, venous or portovenous phases [9, 12, 13]. In the current study, BMD reading was compared before and after contrast injection in all phases. We proved increase BMD when measured after IV contrast injection in the three phases, more evident in the portovenous phase. This is matching with the results of Pirayesh Islamian et al, 2016 who stated that "BMD is increased after intravenous contrast injection in the portovenous phase with p-value of <0.05" [9]. In contrast, the results of Jørgensen Hanne et al study, 2016 proved no significant differences in the BMD reading before and after contrast media administration when measured in the vertebral levels L1 to L4 with the p value = 0.21) [12].As the age of patients increases, the difference between pre and post contrast BMD reading decreases. This was also noticed in other studies [14]. In addition, the current research shows the impact of contrast in the venous phase decreases with age mainly in the female participants. This is supported by the same results of Pirayesh Islamian, 2016 who proved that enhanced images in both female and male was decreased with increasing age [9]. As increasing the patient's age will increase the risk of osteoporosis [15, 16]. Also, osteoporosis in more evident in females mainly after the age of menopause [15, 17, 18, 19]. In this study, 33 patients have osteoporosis, which is more evident in younger females than males. It affects females between the age of 33 – 85 years, and males from the age of 52 to 88 years.
5. Conclusions
- This research proves that the BMD reading increases after IV contrast injection during CT study of the abdomen in the three post contrast phases, but more in the portovenous phase. This should be taken into consideration before diagnosing normal or abnormal bone density depending on BMD reading in CT of the abdomen.
ACKNOWLEDGMENTS
- We would like to thank Dr. Mamdouh Kotob, consultant radiologist at KAUH for his valuable cooperation during the research study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML