-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2017; 7(2): 48-56
doi:10.5923/j.cmd.20170702.03

Depression and Anxiety and Their Correlates in Patients with Diabetes Mellitus in Al-Jouf Region, Saudi Arabia
Abdulrahman Alduraywish1, Diaa Abdel Fattah2, 3, Ahmed Abd-Eltawab4, 5, Mohammed Al-Ruwili6, Arif Alhassan7, Nafe Alnafe8, Fayez Alruwailly9
1Department of Internal Medicine, College of Medicine, Al-Jouf University, Saudi Arabia
2Department of Psychiatry, College of Medicine, Al-Jouf University, Saudi Arabia
3Department of Psychiatry, College of Medicine, Minia University, Egypt
4Department of Physiology, College of Medicine, Al-Jouf University, Saudi Arabia
5Department of Physiology, College of Medicine, Beni-Suef University, Egypt
6Diabetic center, Al-Jouf Region, Saudi Arabia
7Diabetic Center, King Abdulaziz Specialist Hospital, Ministry of Health, Al-Jouf Region, Saudi Arabia
8Department of Internal Medicine, Domat Aljandal Hospital, Al-Jouf Region, Saudi Arabia
9Diabetic Center in King Abdulaziz Specialist Hospital in Aljouf Region, Saudi Arabia
Correspondence to: Diaa Abdel Fattah, Department of Psychiatry, College of Medicine, Al-Jouf University, Saudi Arabia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

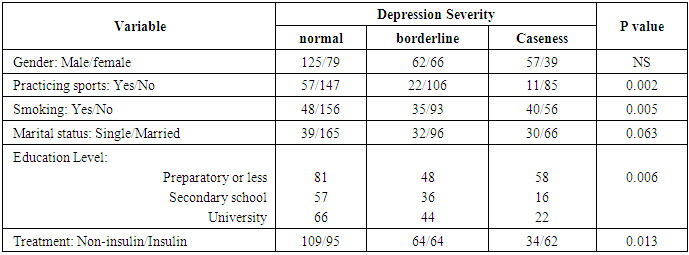
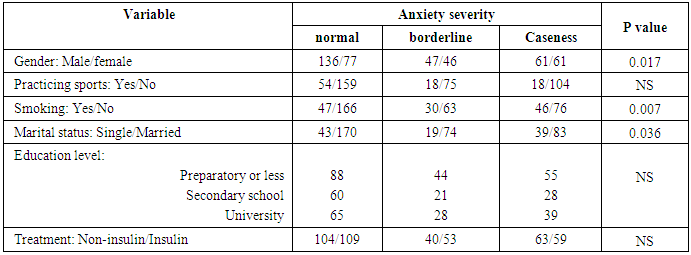
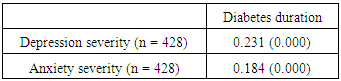
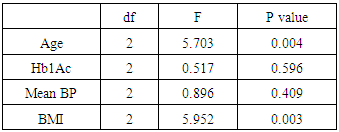
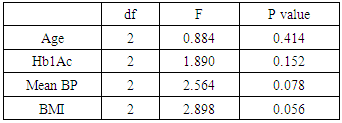
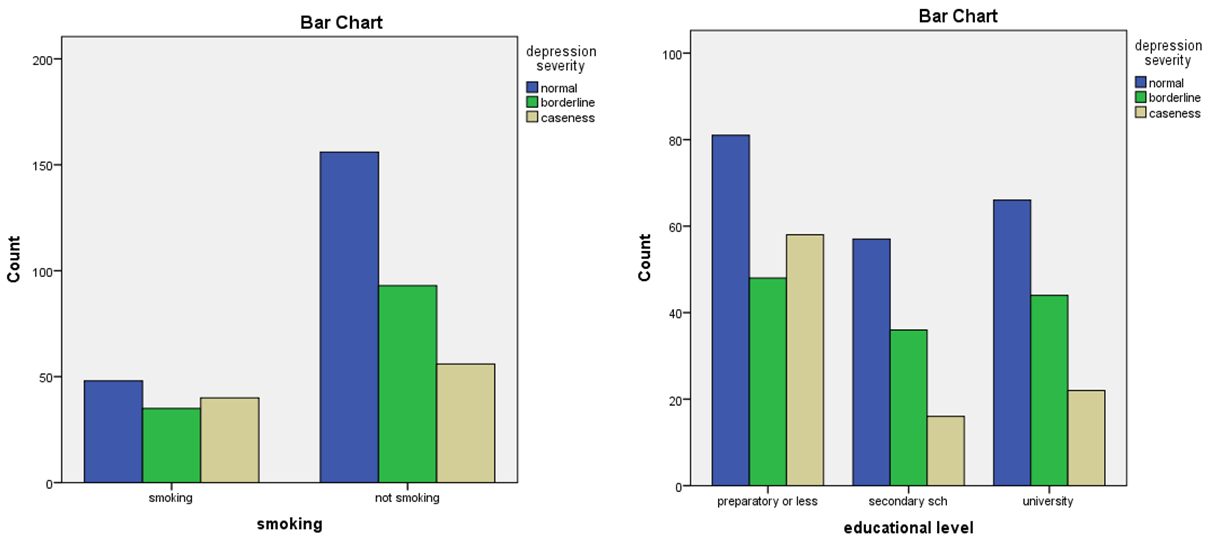
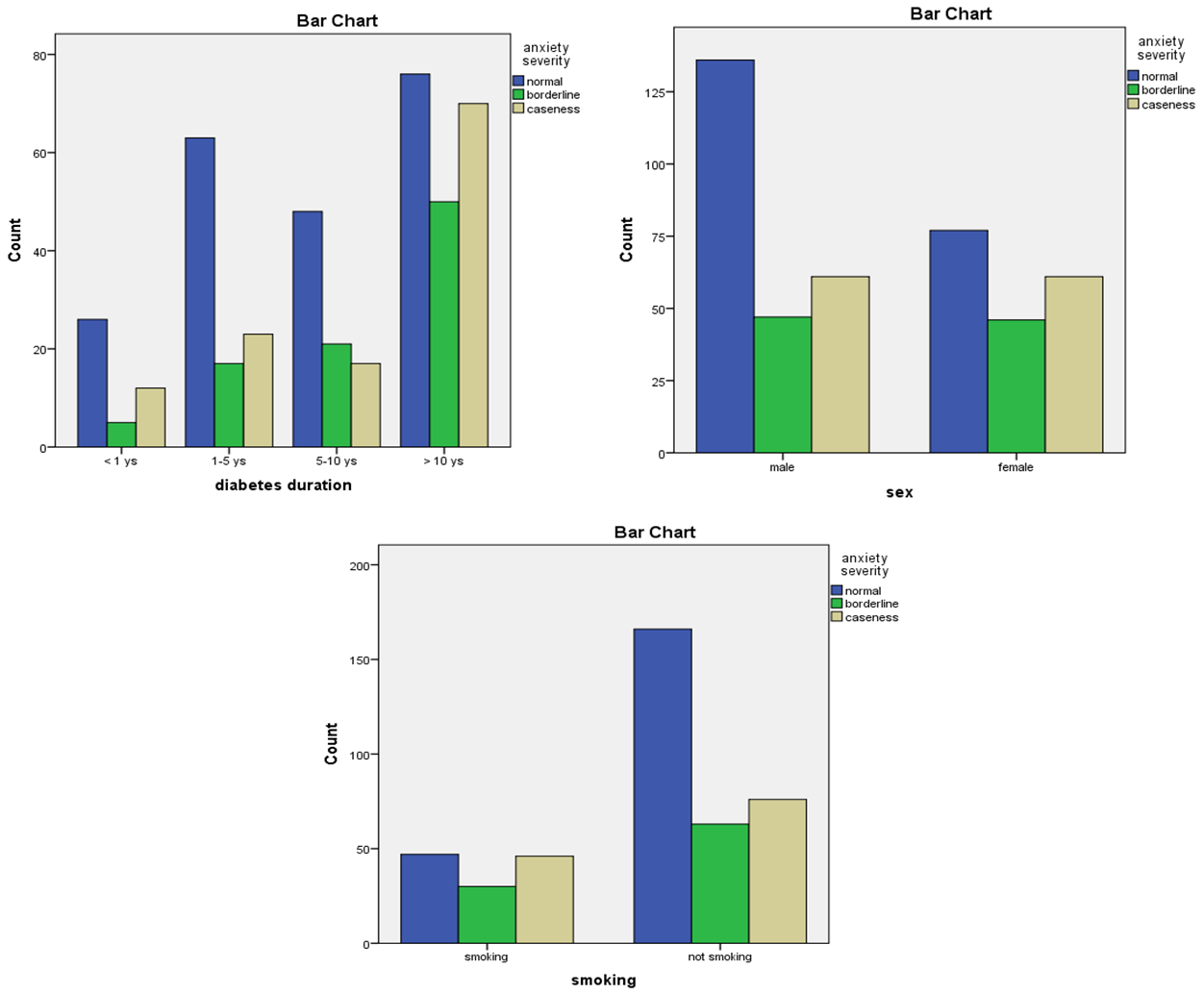
Background: The aim of the study was to study the prevalence of depression and anxiety symptoms in patients with type one and two diabetes mellitus and their correlation with specific socio-demographic and clinical factors. Methods: 428 diabetic patients participated in the present cross-sectional study. Their demographic and clinical parameters were collected. The self-administered questionnaire HADS was used to determine level of depression and anxiety. Results: We found that 22.4% of the sample experienced significant depressive symptoms and 28.5% experienced significant anxiety symptoms. It was found that: Not practicing sports (p = 0.002), smoking (p = 0.005), having lower level of education (p = 0.006) and insulin treatment (p = 0.013) were significantly associated with depression. On the other hand, female gender (p = 0.017), smoking (p = 0.007) and being unmarried (p = 0.036) were significantly associated with anxiety. Correlation showed that depression was significantly associated with BMI (p = 0.003) and age of the patients (p = 0.004). It was found that both anxiety and depression positively correlated significantly with duration of diabetes (p ≤ 0.001). Neither depression nor anxiety was associated with HBA1c levels or with mean blood pressure. Conclusion: Depression and anxiety symptoms were high among patients with type I and II diabetes mellitus. Depression was strongly related to age, lower level of education, smoking, not practicing sports, duration of diabetes, insulin treatment and BMI. Anxiety was strongly related to female gender, smoking, duration of diabetes and being unmarried.
Keywords: Diabetes, Depression, Anxiety, Saudi Arabia
Cite this paper: Abdulrahman Alduraywish, Diaa Abdel Fattah, Ahmed Abd-Eltawab, Mohammed Al-Ruwili, Arif Alhassan, Nafe Alnafe, Fayez Alruwailly, Depression and Anxiety and Their Correlates in Patients with Diabetes Mellitus in Al-Jouf Region, Saudi Arabia, Clinical Medicine and Diagnostics, Vol. 7 No. 2, 2017, pp. 48-56. doi: 10.5923/j.cmd.20170702.03.
1. Introduction
- Worldwide and in Saudi Arabia in particular, diabetes mellitus (DM) is one of the most common chronic diseases. In the country, it is close to be an epidemic [1]. This is due to high caloric intake, obesity and physical inactivity along with genetic predisposition [2, 3]. Unfortunately, the disease prevalence is on the rise locally and worldwide [4-7]. Regarding the International Diabetes Federation, 5 countries of the Gulf region have the highest prevalence rates of diabetes in the world [8]. The prevalence of diabetes in the Kingdom of Saudi Arabia is 23.7% [9]. Diabetes also resulted in the deaths of about 1,256 million in the world in 2008 with most of the deaths in developing countries [10]. Unipolar depression represented 3rd leading cause of disability adjusted life years (DALYS) in 2004 and also unipolar depression is regarded to be the main cause of disease burden by 2030 [10]. Depression and diabetes are usually associated together [11, 12]. Diabetic patients have two fold increases in depression and anxiety symptoms as the general population [13-16]. A study, found that the prevalence and the incidence of anxiety in diabetic patients was significantly increased than the general population - with the higher prevalence related to female gender [17]. Furthermore, depression associating DM affects 10 - 30% of diabetic patients [18]. In Mexico, prevalence of depression in diabetic patients ranged from 46 - 63% [19-21]. In Malaysia, the prevalence of depression was 11.5%, anxiety was 30.5%, and stress 12.5% in patients with type II DM [10]. In Nepal, 54% of the participants experienced depression [22]. In New Delhi, 18% of the sample reported high level of depressive symptoms and more than quarter of diabetic women reported high level of anxiety symptoms [23]. In Morocco, the prevalence of depression in diabetic patients was 33.1% without gender difference and depression was found to be increased in unmarried vs. married patients [24]. In Palestine, prevalence of depression in diabetic patients reached 40.2% [25]. In Arab Emirates, 12.5% of patients reported a high score on a measure that indicates mental health problems [26]. Since the emergence of depression and anxiety and their maintenance is affected by cultural and societal factors [27], studies in different ethnic groups are important. The present cross-sectional study was approved by the Ethical Committees at the College of Medicine, Aljouf University, and Ministry of Health, Sakaka, Al-Jouf, Saudi Arabia and we aimed to study the prevalence of depression and anxiety in diabetic patients and to study their association with some socio-demographic characteristics and clinical parameters in a sample of Saudi diabetic patients from Al-Jouf region.
2. Methods
- Setting:The present cross-sectional study was approved by the Ethical Committees at the College of Medicine, Aljouf University, and Ministry of Health, Sakaka, Al-Jouf, Saudi Arabia. Data were collected during February - May, 2016 at the diabetic centers of king Abdulaziz specialist hospital, Domat Al-Jandal General Hospital and Prince Muteb General Hospital in the northern Al-Jouf region in Saudi Arabia. The region has a 100,212 km2 area and the number of population was 440,009 at the 2010 Census. Participants:Before data were collected, individuals were briefed about the purpose of the survey and the way of completing the questionnaires. They were given the assurance of anonymity and that their content was absolutely confidential. In addition they were informed that the results would be used in the service of science evolution. The sample was collected according to the rules of random sampling. Patients with a history of neurological disorders, such as, stroke, and history of psychiatric disorders, including consequences of recent death and separation were excluded from the study. Also, Patients with infectious episodes that might cause an imbalance in their diabete and Patients with gestational diabetes were also excluded. A total number of 428 patients were included with either type I or type II diabetes. Intervention: The socio-demographic characteristics and clinical parameters of the enrolled Saudi diabetic patients were obtained from the data collection form delivered to patients to be filled partly by the patient and partly by the attending physician. The form included items such as: age, job status, practicing sports, smoking habits, duration since first diagnosed with diabetes, type of treatment of diabetes, education level and marital status. Also, clinical parameters obtained included level of HBA1c, mean blood pressure and body mass index (BMI).Glycated hemoglobin (HbA1c) was assessed using whole blood by affinity column using GLYCO-Tek method (Helena Laboratories). Mean arterial pressure that describes the average blood pressure was calculated as: Mean arterial pressure = diastolic pressure + 1/3 (systolic pressure - diastolic pressure) [28]. BMI was calculated from weight and height of patients. This index has been chosen and implemented for sample evaluation in regard to obesity [29].Depression and anxiety were determined using the hospital anxiety and depression scale questionnaire (HADS) [30]. The questionnaire was afforded in the local simple Arabic language that was validated before [31, 32]. HADS questionnaire contains 14 items with answers in four grades. It consists of 7 questions regarding anxiety and 7 for depression. The answer results ranged from 0 to 3 and maximum sum was 21 for each scale. HADS detects the score of symptoms within the last 10 days. The questionnaire is designed to avoid false positive results in patients with somatic disorders [33, 34]. Scores of 11 or more on either subscale are considered as significant “case” of psychological illness and a score of 8-10 as borderline, while a score of 7 or less is considered normal [35, 36]. Among the 450 questionnaires distributed, 428 were valid for the study. Statistical methods: Data was entered manually into a database and cleaned before analyses. The Statistical Package for the Social Science (SPSS) version 20 software was used for both descriptive and inferential analysis. Items that were not answered by respondents were considered as missing. Univariate statistics such as mean values, standard deviations, frequencies and proportion percentages were derived for continuous and categorical variables respectively. Bivariate analyses was used to measure the strength of association between the variables in the study. All tests were two-tailed with significance defined as p < 0.05. Also, the association between parameters was investigated using Spearman correlation coefficient. The significance was set as p<0.05.
3. Results
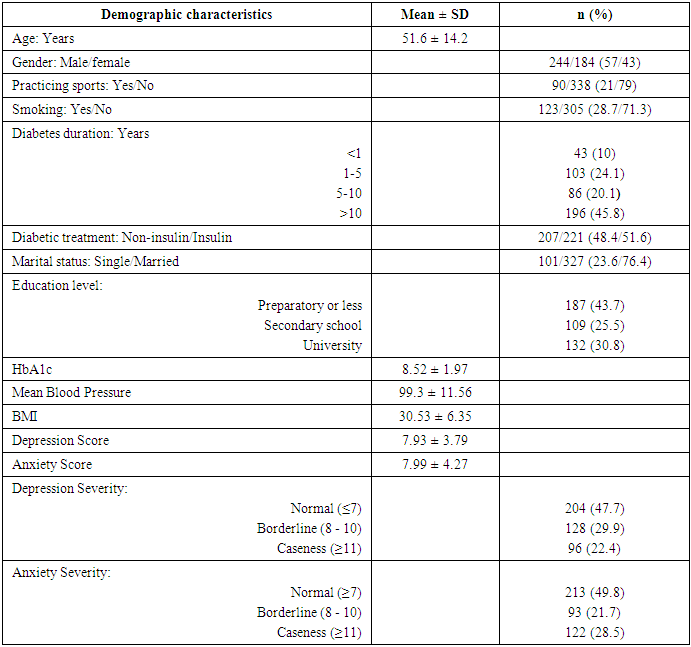
- 428 patients with type I and type II diabetes were studied from which 57% were men and 43% were women. 76.4% were married and 23.6% unmarried. 21% practiced some sort of sports and 79% didn’t. Patients with duration of diabetes of more than 10 years were 45.8%, those with 5 - 10 years duration were 20.1%, those with from 1 - 5 years were 24.1%, and 10% of patients had <1 year disease duration. The patients treated with insulin constituted 51.6% and the remaining 48.4% were on non-insulin treatment. Regarding the educational level, 43.7% were educated to preparatory school level or lower, 25.5% to secondary school level and 30.8% had university education. The mean age of respondents was 52 (51.6 ± 14.2) and their HbA1c was 9 (8.5 ± 1.97). Their mean blood pressure was 100 (99.3 ± 11.56). Their BMI was 31 (30.5 ± 6.35). Furthermore, the mean depression and anxiety scores were 8 (7.9 ± 3.79) and 8 (7.99 ± 4.27), respectively. We found that 22.4% of the sample experienced significant depressive symptoms (caseness, score ≥ 11) and 28.5% experienced significant anxiety symptoms (score ≥ 11) (Table 1).
|
|
 | Figure 1. Association of the prevalence of depression with each of education level and smoking among the participating diabetic patients |
 | Figure 2. Association of the prevalence of anxiety with each of disease duration, gender and smoking among the participating diabetic patients |
|
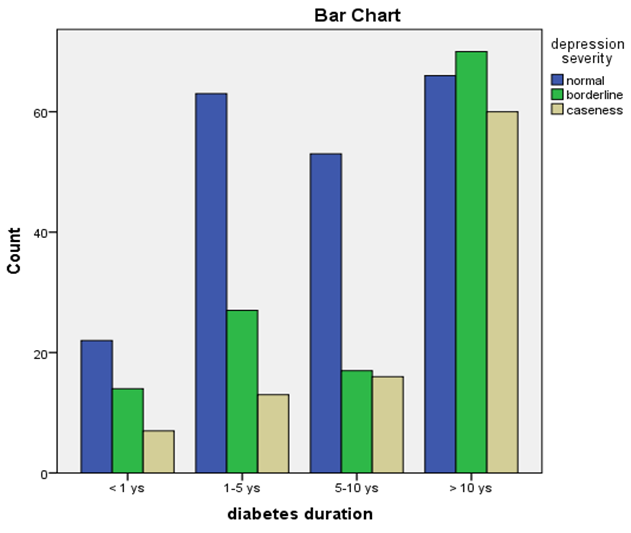 | Figure 3. Association of the prevalence of depression with duration of diabetes among the participating diabetic patients |
|
|
|
4. Discussion
- Anxiety and depression are common psychiatric disorders and they often affect people with chronic and debilitating illnesses such as DM [37, 38]. Our study showed that the prevalence of depression reached 22.4% and that of anxiety was 28.5%. Das-Munshi et al, in a cross sectional study reported that prevalence of any mental disorder was 21.6% in diabetic group versus 16.3% in non diabetic group and it was found that the prevalence of major depression in diabetic patients was mostly around 12% while milder types of depression was reported to be 15-35% [39]. Other studies had found higher depression rates among diabetic patients [40, 41]. Other studies in Saudi Arabia found that the prevalence of depression to be 37% for type 1 and 37.9% for type 2 diabetes in one study in Riyadh and 49.6% for type 2 diabetes in another study [42, 43]. Furthermore, one study reported that patients with diabetes mellitus were 1.4-3 times as likely to suffer from comorbid depression compared to non diabetic control [44]. However, a number of studies found lower prevalence of depression than ours such as a 15.8% in rural America [45], 12.5% at Emirates [26], and 10.2% at Germany [46]. The prevalence of anxiety was more than that of depression and this was comparable to the findings present in current literature in which anxiety was frequently higher than depression [39, 40, 47, 48]. Our results showed that gender was significantly related to anxiety symptoms with 33% of women having anxiety compared to 25% of men. Similarly, many studies showed that women to were more prone to anxiety symptoms [49, 50, 17]. Being unmarried was significantly associated with anxiety. It is well known that being married is related to less liability to develop psychiatric disorders including depression and anxiety [51-53]. It was found that depression was significantly related to the age of the patients and with lower educational level. This was in accordance with the findings of a study on Mexican Americans that found that depressed diabetic patients to be of older age and to have lower education [54]. Lower education may affect income and be a source of stress leading to diabetes and making it a chronic disease [54] and consequently lead to depression.There was no relation between depression or anxiety and the glycemic control index HbA1c. This is in consistence with a study in a Japanese hospital comprising 3305 participants that failed to reveal a relation between depression and HbA1c [55]. Furthermore, a study showed that changes in depressive symptoms were not related to changes in HbA1c or glucose levels in either type I or type II diabetic patients [56]. One explanation for these results is that glycemic control may be affected by other confounding factors that have an influence on mental health function [57]. Regarding anxiety and HbA1c, it was found that a weak correlation only was present between anxiety and HbA1c [58]. A study in Malaysia, found that the anxiety symptoms was not significantly related to glycemic control [57]. There was significant relation between depression and anxiety and diabetes duration. This was in accordance with other studies that found a relation with duration of diabetes [39, 59]. Increased duration of diabetes leads to increased diabetic complications and consequently leads to increased psychological disorders [40]. Depression was significantly related to BMI and was significantly related to not practicing sports. This is similar to a study on Mexican Americans [54] and with a study done in Palestine [25]. A study, suggested that obesity is usually accompanied by low self esteem leading to social and psychological problems [60] and obesity is the main factor leading to occurrence of type II diabetes mellitus [61-63]. However, no significant relation was found between anxiety and BMI and according to one study, a moderate degree level of evidence is present for a positive relation between anxiety and obesity [64]. Regarding significant relation between insulin treatment and depression, this was in agreement with a number of studies that found that insulin treatment was related to depressive symptoms [65, 66, 50].Our study showed significant relation between depression and anxiety and smoking. Anxiety is often associated with smoking [67] and nicotine dependence [68, 69]. Accordingly, some studies showed a high prevalence of anxiety symptoms among diabetic smokers than non-smokers [70, 71]. Also, symptoms of anxiety and depression have been strongly related to risky health behaviors such as smoking, alcohol intake and low physical activity [67, 72, 39]. This may have led to the significant association between depression and anxiety and smoking in our study. Our study showed no relation between depression or anxiety and mean blood pressure. Similarly, a study of 110 African-American patients with diabetes reported no association of depression with blood pressure, over a 3-year period [73]. Another study found no relation between depression and systolic blood pressure in diabetic patients [74].Our study is the first study that study anxiety and depression in diabetic patients in Al-Jouf region of Saudi Arabia. However, there are limitations in our study. Firstly, it is a cross-sectional study that doesn’t allow for cause and effect relationship to be extracted. Secondly, HADS questionnaire is a screening instrument and is not designed of specific psychiatric disorders. Also, there was a possibility for a recall bias by the participants and this was overcome by limiting the recall period to 7 days before the filling of the questionnaire. The information regarding age, type of treatment, and duration of diabetes was matched against the medical records where applicable. As part of the complete management plan and care for diabetic patients, we advise that the screening for depression and anxiety should be done regularly for diabetic patients and vulnerable subjects should have special attention and appropriate intervention leading to better overall outcome.
5. Conclusions
- Our study illustrates that the prevalence of depression was 22.4% and that of anxiety reached 28.5%. Depression was significantly associated with not practicing sports, smoking, lower educational level, insulin treatment, BMI and age of the patients. Depression also significantly correlated with diabetes duration.Anxiety was significantly associated with female gender, smoking and being unmarried. Anxiety also significantly correlated with diabetes duration. Our results may help primary care physicians and direct their attention towards a high risk group of patients with diabetes mellitus for screening of depression and anxiety.
ACKNOWLEDGEMENTS
- The authors would like to thank the nursing and technical staff of King Abdulaziz Hospital and Domat Aljandal Hospital for providing cooperation, support and assistance in gathering data.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML