| [1] | Ko HK, Hsu WH, Hsieh CC, Lien TC, Lee TS, Kou YR. High expression of high‐mobility group box 1 in the blood and lungs is associated with the development of chronic obstructive pulmonary disease in smokers. Respirology. 2014; 19(2): 253-61. |
| [2] | Wang H, Yang T, Li D, Wu Y, Zhang X, Pang C, Zhang J, Ying B, Wang T, Wen F. Elevated circulating PAI-1 levels are related to lung function decline, systemic inflammation, and small airway obstruction in chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease. 2016;11:2369. |
| [3] | Gopal P, Reynaert NL, Scheijen JL, Schalkwijk CG, Franssen FM, Wouters EF, Rutten EP. Association of plasma sRAGE, but not esRAGE with lung function impairment in COPD. Respiratory research. 2014; 15(1): 24. |
| [4] | Barnes PJ, Shapiro SD, Pauwels RA. Chronic obstructive pulmonary disease: molecular and cellularmechanisms. European Respiratory Journal. 2003; 22(4): 672-88. |
| [5] | Mroz RM, Noparlik J, Chyczewska E, Braszko JJ, Holownia A. Molecular basis of chronic inflammation in lung diseases: new therapeutic approach. Journal of Physiology and Pharmacology. 2007 Nov 1; 58(5): 453-60. |
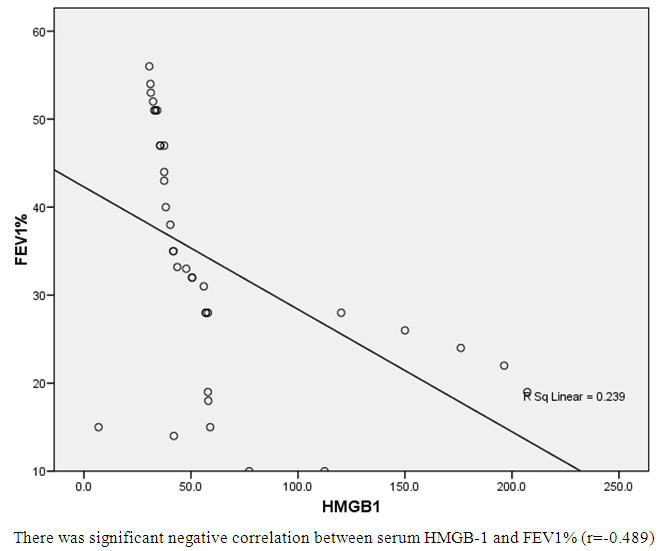
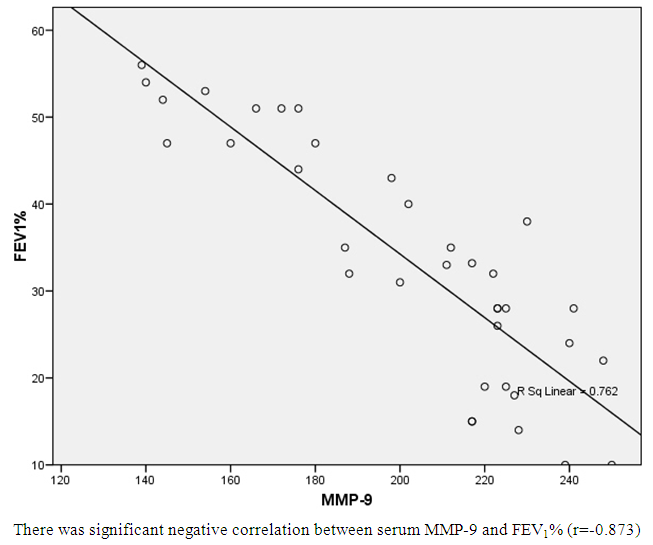
| [6] | Fattouh M, Alkady O. Inflammatory biomarkers in chronic obstructive pulmonary disease. Egyptian Journal of Chest Diseases and Tuberculosis. 2014; 63(4): 799-804. |
| [7] | Eagan TM, Ueland T, Wagner PD, Hardie JA, Mollnes TE, Damås JK, Aukrust P, Bakke PS. Systemic inflammatory markers in COPD: results from the Bergen COPD Cohort Study. European respiratory journal. 2010 Mar 1; 35(3): 540-8. |
| [8] | Hacievliyagil SS, Mutlu LC, Temel I. Airway inflammatory markers in chronic obstructive pulmonary disease patients and healthy smokers. Nigerian journal of clinical practice. 2013; 16(1): 76-81. |
| [9] | Mannino DM, Tal-Singer R, Lomas DA, Vestbo J, Barr RG, Tetzlaff K, Lowings M, Rennard SI, Snyder J, Goldman M, Martin UJ. Plasma fibrinogen as a biomarker for mortality and hospitalized exacerbations in people with COPD. Chronic obstructive pulmonary diseases (Miami, Fla.). 2015; 2(1): 23. |
| [10] | Seemungal TA, Lun JC, Davis G, Neblett C, Chinyepi N, Dookhan C, Drakes S, Mandeville E, Nana F, Setlhake S, King CP. Plasma homocysteine is elevated in COPD patients and is related to COPD severity. International journal of chronic obstructive pulmonary disease. 2007; 2(3): 313. |
| [11] | Chen Q, Guan X, Zuo X, Wang J, Yin W. The role of high mobility group box 1 (HMGB1) in the pathogenesis of kidney diseases. Acta Pharmaceutica Sinica B. 2016; 6(3): 183-8. |
| [12] | Tang D, Kang R, Zeh III HJ, Lotze MT. High-mobility group box 1, oxidative stress, and disease. Antioxidants & redox signaling. 2011; 14(7): 1315-35. |
| [13] | Fang WH, Yao YM, Shi ZG, Yu Y, Wu Y, Lu LR, Sheng ZY. The significance of changes in high mobility group-1 protein mRNA expression in rats after thermal injury. Shock. 2002; 17(4): 329-33. |
| [14] | Ulloa L, Batliwalla FM, Andersson U, Gregersen PK, Tracey KJ. High mobility group box chromosomal protein 1 as a nuclear protein, cytokine, and potential therapeutic target in arthritis. Arthritis & Rheumatology. 2003; 48(4): 876-81. |
| [15] | Sun S, Zhang W, Cui Z, Chen Q, Xie P, Zhou C, Liu B, Peng X, Zhang Y. High mobility group box-1 and its clinical value in breast cancer. OncoTargets and therapy. 2015; 8: 413. |
| [16] | Ueno H, Matsuda T, Hashimoto S, Amaya F, Kitamura Y, Tanaka M, Kobayashi A, Maruyama I, Yamada S, Hasegawa N, Soejima J. Contributions of high mobility group box protein in experimental and clinical acute lung injury. American journal of respiratory and critical care medicine. 2004; 170(12): 1310-6. |
| [17] | Hou C, Zhao H, Liu L, Li W, Zhou X, Lv Y, Shen X, Liang Z, Cai S, Zou F. High mobility group protein B1 (HMGB1) in Asthma: comparison of patients with chronic obstructive pulmonary disease and healthy controls. Molecular Medicine. 2011; 17(7): 807-15. |
| [18] | Gangemi S, Casciaro M, Trapani G, Quartuccio S, Navarra M, Pioggia G, Imbalzano E. Association between HMGB1 and COPD: a systematic review. Mediators of inflammation. 2015; 2015. |
| [19] | Feng L, Xue D, Chen E, Zhang W, Gao X, Yu J, Feng Y, Pan Z. HMGB1 promotes the secretion of multiple cytokines and potentiates the osteogenic differentiation of mesenchymal stem cells through the Ras/MAPK signaling pathway. Experimental and Therapeutic Medicine. 2016; 12(6): 3941-7. |
| [20] | Konjevic G, Gopčević K, V Jovic, Inic M and Jurisic V. Activity of MMP-2 and MMP-9 in sera of breast cancer patients. Stankovic S,. Pathol Res Pract. 2010 Jun 15; 206 (4): 241-7. |
| [21] | Radenkovic S, Konjevic G, Jurisic V, Karadzic K, M Nikitovic, Gopčević K. Values of MMP-2 and MMP-9 in the tumor tissue of basal-like breast cancer patients. Cell Biochem Biophys. 2014 Jan; 68 (1): 143-52. |
| [22] | Piesiak P, Brzecka A, Kosacka M, Passowicz-Muszyńska E, Dyła T, Jankowska R. Concentrations of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinases-1 in serum of patients with chronic obstructive pulmonary disease. Polski merkuriusz lekarski: organ Polskiego Towarzystwa Lekarskiego. 2011; 31(185): 270-3. |
| [23] | Dilek F, Ozceker D, Ozkaya E, Tamay Z, Yazici M, Kesgin S, Kocyigit A, Guler N. Plasma levels of matrix metalloproteinase-9 in children with chronic spontaneous urticaria. Allergy, asthma & immunology research. 2016; 8(6): 522-6. |
| [24] | Sang QX, Muroski ME, Roycik MD, Newcomer RG, Van den Steen PE, Opdenakker G, Monroe HR, Sahab ZJ. Matrix metalloproteinase-9/gelatinase B is a putative therapeutic target of chronic obstructive pulmonary disease and multiple sclerosis. Current pharmaceutical biotechnology. 2008; 9(1): 34-46. |
| [25] | Omachi TA, Eisner MD, Rames A, Markovtsova L, Blanc PD. Matrix metalloproteinase-9 predicts pulmonary status declines in α 1-antitrypsin deficiency. Respiratory research. 2011; 12(1): 35. |
| [26] | Culpitt SV, Rogers DF, Traves SL, Barnes PJ, Donnelly LE. Sputum matrix metalloproteases: comparison between chronic obstructive pulmonary disease and asthma. Respiratory medicine. 2005; 99(6): 703-10. |
| [27] | Vernooy JH, Lindeman JH, Jacobs JA, Hanemaaijer R, Wouters EF. Increased activity of matrix metalloproteinase-8 and matrix metalloproteinase-9 in induced sputum from patients with COPD. CHEST Journal. 2004;126(6):1802-10. |
| [28] | Louhelainen N, Stark H, Mazur W, Rytilä P, Djukanovic R, Kinnula VL. Elevation of sputum matrix metalloproteinase-9 persists up to 6 months after smoking cessation: a research study. BMC pulmonary medicine. 2010;10(1):13. |
| [29] | Pouwels SD, Nawijn MC, Bathoorn E, Riezebos-Brilman A, van Oosterhout AJ, Kerstjens HA, Heijink IH. Increased serum levels of LL37, HMGB1 and S100A9 during exacerbation in COPD patients. European Respiratory Journal. 2015; 45(5): 1482-5. |
| [30] | Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. Available from: http://goldcopd.org/. |
| [31] | Spruit MA, Singh SJ. Maintenance programs after pulmonary rehabilitation: how may we advance this field?. CHEST Journal. 2013; 144(4): 1091-3. |
| [32] | Stenton C. The MRC breathlessness scale. Occupational Medicine. 2008; 58(3): 226-7. |
| [33] | ATS Statement: Guidelines for the Six-Minute Walk Test: Am J Respir Crit Care Med 2002;166:111–117. |
| [34] | Celli BR, MacNee WA, Agusti AA, Anzueto A, Berg B, Buist AS, Calverley PM, Chavannes N, Dillard T, Fahy B, Fein A. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. European Respiratory Journal. 2004; 23(6): 932-46. |
| [35] | Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Enright P, van der Grinten CM, Gustafsson P, Jensen R. General considerations for lung function testing. European Respiratory Journal. 2005; 26(1): 153-61. |
| [36] | Hermans C, Bernard A. Pneumoproteinaemia: a new perspective in the assessment of lung disorders. European Respiratory Journal. 1998; 11(4): 801-3. |
| [37] | Hermans C, Bernard A. Lung epithelium–specific proteins: characteristics and potential applications as markers. American journal of respiratory and critical care medicine. 1999; 159(2): 646-78. |
| [38] | Entezari M, Javdan M, Antoine DJ, Morrow DM, Sitapara RA, Patel V, Wang M, Sharma L, Gorasiya S, Zur M, Wu W. Inhibition of extracellular HMGB1 attenuates hyperoxia-induced inflammatory acute lung injury. Redox biology. 2014; 2:314-22. |
| [39] | Musumeci D, Roviello GN, Montesarchio D. An overview on HMGB1 inhibitors as potential therapeutic agents in HMGB1-related pathologies. Pharmacology & therapeutics. 2014; 141(3): 347-57. |
| [40] | Russell RE, Culpitt SV, DeMatos C, Donnelly L, Smith M, Wiggins J, Barnes PJ. Release and activity of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 by alveolar macrophages from patients with chronic obstructive pulmonary disease. American journal of respiratory cell and molecular biology. 2002; 26(5): 602-9. |
| [41] | Shang GH, Jia CQ, Tian H, Xiao W, Li Y, Wang AH, Dong L, Lin DJ. Serum high mobility group box protein 1 as a clinical marker for non-small cell lung cancer. Respiratory medicine. 2009; 103(12): 1949-53. |
| [42] | Zhang Y, Li S, Wang G, Han D, Xie X, Wu Y, Xu J, Lu J, Li F, Li M. Changes of HMGB1 and sRAGE during the recovery of COPD exacerbation. Journal of thoracic disease. 2014; 6(6): 734-41. |
| [43] | Cheng Z, Kang Y, Wu QG, Dai LL, Song YN, Xia J, Si JM, Chen CY. Levels of HMGB1 in induced sputum from patients with asthma and chronic obstructive pulmonary disease. Zhonghua yi xue za zhi. 2011; 91(42): 2981-4. |
| [44] | Iwamoto H, Gao J, Pulkkinen V, Toljamo T, Nieminen P, Mazur W. Soluble receptor for advanced glycation end-products and progression of airway disease. BMC pulmonary medicine. 2014; 14(1): 68. |
| [45] | Ferhani N, Letuve S, Kozhich A, Thibaudeau O, Grandsaigne M, Maret M, Dombret MC, Sims GP, Kolbeck R, Coyle AJ, Aubier M. Expression of high-mobility group box 1 and of receptor for advanced glycation end products in chronic obstructive pulmonary disease. American journal of respiratory and critical care medicine. 2010; 181(9): 917-27. |
| [46] | Di Stefano A, Caramori G, Barczyk A, Vicari C, Brun P, Zanini A, Cappello F, Garofano E, Padovani A, Contoli M, Casolari P. Innate immunity but not NLRP3 inflammasome activation correlates with severity of stable COPD. Thorax. 2014; 69(6): 516-24. |
| [47] | Bezerra FS, Valença SS, Pires KM, Lanzetti M, Pimenta WA, Schmidt AC, Porto LC, Zin WA. Long-term exposure to cigarette smoke impairs lung function and increases HMGB-1 expression in mice. Respiratory physiology & neurobiology. 2011; 177(2): 120-6. |
| [48] | Kanazawa H, Tochino Y, Asai K, Ichimaru Y, Watanabe T, Hirata K. Validity of HMGB1 measurement in epithelial lining fluid in patients with COPD. European journal of clinical investigation. 2012; 42(4): 419-26. |
| [49] | Vignola AM, Riccobono L, Mirabella A et al.(1998): Sputum metalloproteinase-9/tissue metalloproteinase-1 ratio correlates with airflow obstruction in asthma and chronic bronchitis. American Journal of Respiratory and Critical Care Medicine. 1998; 158(6): 1945-50. |
| [50] | Brajer B, Batura-Gabryel H, Nowicka A, Kuznar-Kaminska B, Szczepanik A. Concentration of matrix metalloproteinase-9 in serum of patients with chronic obstructive pulmonary disease and a degree of airway obstruction and disease progression. J Physiol Pharmacol. 2008; 59(Suppl 6): 145-52. |
| [51] | Xin XF, Zhao M, Li ZL, Song Y, Shi Y. Metalloproteinase-9/tissue inhibitor of metalloproteinase-1 in induced sputum in patients with asthma and chronic obstructive pulmonary disease and their relationship to airway inflammation and airflow limitation. Zhonghua jie he he hu xi za zhi= Zhonghua jiehe he huxi zazhi= Chinese journal of tuberculosis and respiratory diseases. 2007; 30(3): 192-6. |
| [52] | Beeh KM, Beier J, Kornmann O, Buhl R. Sputum matrix metalloproteinase-9, tissue inhibitor of metalloprotinease-1, and their molar ratio in patients with chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis and healthy subjects. Respiratory medicine. 2003; 97(6): 634-9. |
| [53] | Mercer P, Shute J, Bhowmik A, Donaldson G, Wedzicha J, Warner J. MMP-9, TIMP-1 and inflammatory cells in sputum from COPD patients during exacerbation. Respiratory Research. 2005; 6(1):151. |
| [54] | Esa SA, RawyAM, EL-Behissy MM, Kamel MH and El-Hwaitty HM. Study of the level of sputum matrix metalloproteinase-9 (MMP-9) and tissue inhibitor metalloproteinase-1 (TIMP-1) in COPD patients; Egypt. J. Chest Dis. Tuberc., 4 (63) (2014), pp. 861–867. |
| [55] | Linder R, Rönmark E, Pourazar J, Behndig A, Blomberg A, Lindberg A. Serum metalloproteinase-9 is related to COPD severity and symptoms - cross-sectional data from a population based cohort-study. Respir Res.( 2015 ) 21; 16:28. |
| [56] | Kang MJ, Oh YM, Lee JC, Kim DG, Park MJ, Lee MG, Hyun IG, Han SK, Shim YS, Jung KS. Lung matrix metalloproteinase-9 correlates with cigarette smoking and obstruction of airflow. Journal of Korean medical science. 2003; 18(6): 821. |
| [57] | Mao JT, Tashkin DP, Belloni PN, Baileyhealy I, Baratelli F, Roth MD. All-trans retinoic acid modulates the balance of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 in patients with emphysema. CHEST Journal. 2003; 124(5): 1724-32. |
| [58] | Olafsdottir IS, Janson C, Lind L, Hulthe J, Gunnbjörnsdóttir M, Sundström J. Serum levels of matrix metalloproteinase‐9, tissue inhibitors of metalloproteinase‐1 and their ratio are associated with impaired lung function in the elderly: A population‐based study. Respirology. 2010;15(3):530-5. |
| [59] | Abd El-Fatah, M. F., Ghazy, M. A., Mostafa, M. S., El-Attar, M. M., & Osman, A. (2015). Identification of MMP-9 as a biomarker for detecting progression of chronic obstructive pulmonary disease. Biochemistry and Cell Biology, 93(6), 541-547. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML