-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2016; 6(3): 70-76
doi:10.5923/j.cmd.20160603.05

Associating Disseminated Intravascular Coagulation with Clinical and Laboratory Evaluations of Pediatric Patients with Acute Gastroenteritis admitted at Gharyan Central and Teaching Hospital, Libya
Aisha A. Sehari1, Badridden F. A. Abufayed2, June II A. Kiblasan2, Florbeth U. Madamba2
1Faculty of Medicine, University of Tripoli, Tripoli, Libya
2Faculty of Nursing, Al Jabal Al Gharbi University, Gharyan, Libya
Correspondence to: June II A. Kiblasan, Faculty of Nursing, Al Jabal Al Gharbi University, Gharyan, Libya.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Globally, acute gastroenteritis is an ailment that is very common among children during their first 3 years of life at which they will most likely experience about 1 to 3 acute diarrheal illnesses that can generate complication such as dehydration and disseminated intravascular coagulation. The diagnosis itself and its accompanying complications can be easily identified though proper clinical and laboratory evaluation. The purpose of this study was to identify evidences of disseminated intravascular coagulation (DIC) and correlate with other clinical or laboratory tests related to other complications of acute gastroenteritis (AGE) such as dehydration and some metabolic imbalances. Almost all of pediatrics patient who are severely dehydrated, suffering from hypernatremia and with hyperammonemia are with evidences of DIC. Moreover, some of the variables found to be significantly associated with positive and strong relationship while some are not.
Keywords: Disseminated Intravascular Coagulation, Laboratory and Clinical Evaluation, Pediatric Patients, Dehydration, Acute Gastroenteritis
Cite this paper: Aisha A. Sehari, Badridden F. A. Abufayed, June II A. Kiblasan, Florbeth U. Madamba, Associating Disseminated Intravascular Coagulation with Clinical and Laboratory Evaluations of Pediatric Patients with Acute Gastroenteritis admitted at Gharyan Central and Teaching Hospital, Libya, Clinical Medicine and Diagnostics, Vol. 6 No. 3, 2016, pp. 70-76. doi: 10.5923/j.cmd.20160603.05.
Article Outline
1. Introduction
- Diagnosing a disease or illness is done through different process as per health care professional’s advice to which laboratory diagnostics is one of it. But doing such diagnosis is quite difficult without a specialized physician. There are times that confusion occurs most especially if there are other accompanying findings that are not related to the physician’s impression regarding to the health status of the patient. This is one of which a physician usually decides to associate such other findings to the primary illness. Diarrheal disease is one of the common health problem experienced during childhood most especially during infancy to toddlerhood. Worldwide, children younger than 5 years have an estimated 1.7 billion episodes of diarrhea in a year, leading to 124 million clinic visits, 9 million hospitalizations, and 1.34 million deaths, with more than 98% of these deaths occurring in the developing world. [1-4] This kind of health problems by most of the pediatrics are usually admitted in the hospital and diagnosed with acute gastroenteritis and is important to be monitored for it accounts huge number of deaths each year in young children mostly in developing communities. Although the prevalence of acute gastroenteritis (AGE) in children has changed little over the past 4 decades, mortality has declined sharply, from 4.6 million in the 1970s to 3 million in the 1980s and 2.5 million in the 1990s at which its reduction was the increasing international support for the use of oral rehydration solution (ORS) as the treatment of choice for acute diarrhea, with the proportion of diarrheal episodes treated with ORS rising from 15% in 1984 to 40% in 1993. [5] Evaluating a child with diarrhea and/or vomiting has to concentrate on several important points and observations to assess severity and determine its etiology and pathogen. Information on the number, volume, and/or fluidity of stools and emesis should be obtained. [6] However, this can be rather cumbersome if the number of episodes is large since recording the volume of each stool and emesis is unrealistic and not very helpful clinically, once the number of episodes exceeds 5 to 10. Complications of Acute Gastroenteritis are responsible for about four million deaths each year largely amongst children less than two years old. Death occurred mainly due to the gross defects in diagnosis and management of complications [7, 8] such as dehydration, Hypokalemia, Metabolic Acidosis, Seizure, and DIC. Dehydration is probably caused by loss of water and electrolytes in the liquid stool and vomitus while hypokalemia is common due to large potassium losses in the stools and shifting of potassium from intracellular to extracellular compartment due to acidosis. Furthermore, metabolic acidosis is due to loss of large amount of bicarbonate in stools, excessive lactic acid production when patient is in a state of shock, formation of inorganic acid in bowel from incomplete breakdown of carbohydrates and retention of hydrogen ions in the circulation due to hypoperfusion of the kidneys. Seizure is commonly related to increase or decrease of sodium level while gastrointestinal and nutritional complications are secondary to carbohydrates malabsorption or intolerance and malnutrition. On the other hand, DIC is supposed to be precipitated by acidosis, hemoconcentration and possibly by the endothelial damage (vasculitits). There may be widespread thrombosis affecting especially the lungs and kidneys. Clinically, DIC presents with bleeding tendencies together with anemia and the presences of large necrotic areas of skin and subcutaneous tissues. [9, 10]In Libya, since the era of oral hydration recommended by WHO, the incidence of acute diarrheal morbidity is 668.4 per 1000 infant and mortality is 18.45 per 1000 infants that has declined to a satisfactory level in only few Libyan areas. [11] Dehydration, which may be associated with electrolyte imbalance, metabolic acidosis and even shock are the most frequent and dangerous complication. These factors (single or combined) may predispose to the risk of disseminated intravascular coagulopathy (DIC) [12] which is always encountered as the secondary serious complication that accompany and/or follow some medical and surgical problem. [13] The major clinical feature of DIC is bleeding, often of serious magnitude and abrupt onset, a variable element of shock that is frequently out of proportion to apparent blood loss, and symptoms of hypoperfusion of various vascular beds resulting to death if not be detected and treated. Knowing that DIC is one of the dangerous complications of AGE, this study came up with a purpose to find the association of disseminated intravascular coagulation with dehydration based on the results of clinical and laboratory evaluations.
2. Methodology
- Mixed method was utilized in this retrospective study. Qualitatively, observational case design was employed though it is crucial to use as methodology but in this research, the object of study is a case. Stake stated that “As a form of research, case study is defined by interest in individual cases, not by the methods of inquiry used”. [14] Furthermore, a case study is an approach to research that focuses on gaining an in-depth understanding of a particular entity or event at a specific time that was the real scenario of this study. Therefore, as Willig asserted, case studies are not characterized by the methods used to collect and analyze data, but rather its focus on a particular unit of analysis: a case [15]. Moreover, intrinsic or purposeful sampling was applied from June to December 2015 and the respondents are pediatric patients with diagnosis of acute gastroenteritis admitted at Gharyan Central Teaching Hospital following two criterions to be qualified as respondents of this craft that include: age range of more than a month up to two years old, complaint of acute diarrhea for 2 – 3 days duration with or without vomiting, degree of dehydration should be either moderate or severe grades, and clinically suggested of having a manifestation of DIC complications such as coffee ground vomitus, bleeding at the puncture sites, severe pallor and other. On the other hand, pediatric patients with overt signs of severe protein calorie malnutrition and history or signs of congenital bleeding defect such as hemophilia, purpura and alike are among who are excluded in this study. All cases were subjected to clinical and laboratory evaluation. Clinical evaluation includes the detailed history taking and a full clinical examination stressing on intake of drugs that may affect the platelets functions, degree of dehydration, hemorrhagic manifestations, presence of malnutrition, severe infection and place of living. Figure 1 showed how the degree of dehydration was evaluated.
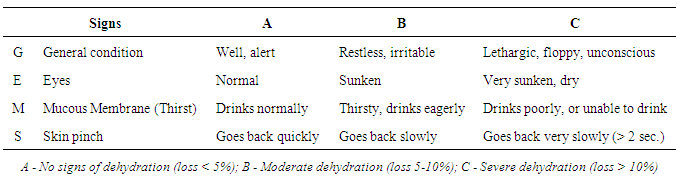 | Figure 1. Basis on evaluating the degree of dehydration |
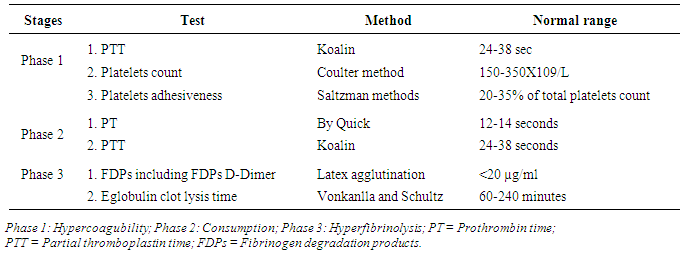 | Figure 2. Basis on evaluating for the presence of DIC |
3. Results
3.1. Report on Clinical and Laboratory Evaluations of Patients with AGE
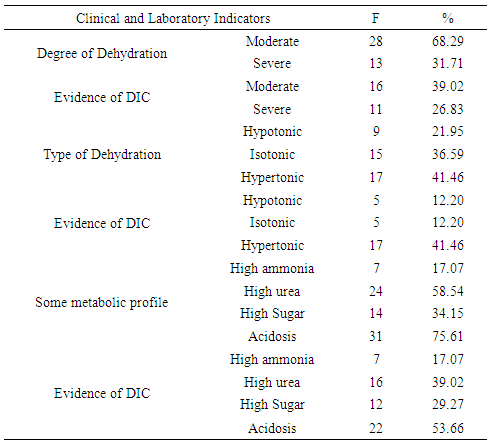
- This study accommodated all admissions in the pediatric ward of Gharyan Central Teaching hospital diagnosed with AGE. The authors identified the respondents based on the criterions shown in figure 1 and 2. Table 1 showed the distribution of samples according to degree of dehydration, type of dehydration, some metabolic profile and its evidences of having DIC. There were 41 total admissions in the pediatric department from June to December 2015 diagnosed with AGE.
|
3.2. Relationship between Laboratory Evaluations
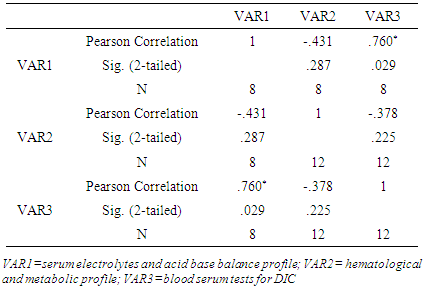
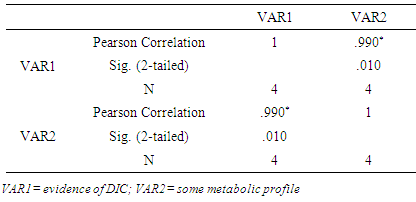
- It is one of the purposes of this study to know if laboratory evaluations have associations among them. To wit, PPMCC was utilized. Table 2 presented if the blood serum tests for DIC, serum electrolytes and acid base profile, and metabolic profile are related. Statistically, there is significant correlation between VAR1 and VAR3 [r = .760; n =8, 12; p =.029] while there is no significant correlations between VAR1 and VAR2 [r = -.431; n =8, 12; p =.287], and VAR2 and VAR3 [r = -.378; n =12, 12; p =.225].
|
|
|
|
4. Discussion
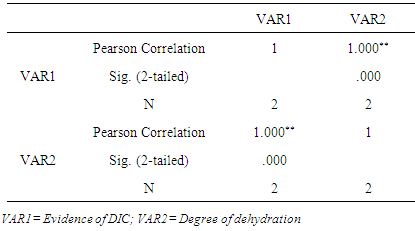
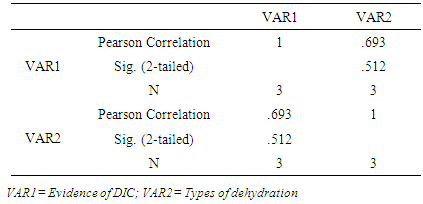
- Laboratory and clinical evaluations are necessary to consider in terms of diagnosing a disease and rolling out its accompanying complications to which its association is something that is vital for it guides a professional health worker in treating the disease as well as eradicating the clinical manifestations. In this study, the authors’ interest were triggered to find out possible accompanying complications of AGE aside from dehydration as the commonest and known and how does it is associated. Moreover, why is it that there are increasing mortality rate due to this case for younger children? Diarrheal illnesses in younger children causes 3 million physician visits where 10% require hospitalization at which the most frequent cause of death is gastroenteritis and its consequences of dehydration and acidosis; other causes of death in a hospitalized patient are with infections, hypoglycaemia, hypokalaemia, and electrolyte abnormalities. [16] Worldwide, dehydration secondary to diarrheal illness is the leading cause of infant and child mortality. Acute diarrhea remains one of the most important health issues worldwide, with high morbidity and mortality rates, accounting for more than two million deaths annually [17, 18]. Further, this is one of the common infectious diseases in developing countries, mostly affecting children younger than five years old. Whereas most cases of acute diarrhea are with dehydration. With the optimal treatment consisting solely of oral rehydration and nutritional support, practitioners in ambulatories or emergency rooms, especially in developing countries, are frequently faced with life-threatening presentations, characterized by signs of severe dehydration, toxemia, marked leucocytosis with high percentages of immature forms, high grade fever, severe welfare depression, tenesmus, gross fecal blood loss and dissemination of infection. Generally, younger children are at the highest risk for dehydration due to larger body water content, renal immaturity, and inability to meet their own needs independently and older children show signs of dehydration sooner than infants due to lower levels of extracellular fluid (ECF). This is the reason why this study concentrated on younger children as the respondents. It is important to look into the effect of dehydration as this scenario is referring to negative fluid balance as the result of either from fluid shift that more likely occurs in patient with sepsis where the decrease in total body water causes reductions in both the intracellular and extracellular fluid volume. Clinical manifestations of dehydration are most closely related to intravascular volume depletion. As dehydration progress, hypovolemic shock ultimately ensues resulting to end organ failure and death.One of the common causes of dehydration is gastroenteritis which is considered as the primary and life threatening. If both vomiting and diarrhea are present, dehydration may rapidly progress. [19, 20] Moreover, dehydration can simulate toxemia and mislead the clinical assessment of severity. As a consequence, volumetric expansion, electrolyte corrections and nutritional support should always be performed before any other therapeutic measure. A few cases, however, may require antimicrobial therapy, because of the severity of the clinical picture or a patient’s increased potential to develop complications, such as dissemination of the disease, sepsis or disseminated intravascular coagulation. Disseminated intravascular clotting or coagulation (DIC) has been reported in gastroenteritis [21]. DIC is a pathological process characterized by the overstimulation of the clotting cascade leading to microthrombi in the small blood vessels [22]. DIC occurs as a complication of another underlying condition including gastroenteritis. DIC describes a constellation of clinical and laboratory abnormalities resulting from a combination of accelerated fibrinogenesis and fibrinolysis. DIC can serve as the final common pathway for a variety of disorders that activate the coagulation system and lead to the systemic circulation of thrombin and plasmin [23] that is estimated to be present in as many as 1% of hospitalized patients. [24] DIC is not itself a specific illness; rather, it is a complication or an effect of the progression of other illnesses. It is always secondary to an underlying disorder and is associated with a number of clinical conditions, generally involving activation of systemic inflammation. Laboratory findings include thrombocytopenia, prolongation of the prothrombin time and activated partial thromboplastin time; elevated fibrin split products, and reduction in the amount of clotting factors, particularly fibrinogen. The peripheral blood smear may reveal microangiopathic changes in the RBCs such as schistocytes.In children, DIC is most often associated with overwhelming sepsis, particularly with gram-negative bacteria. The proposed mechanism is endotoxemia, which leads to cytokinemediated activation of the extrinsic coagulation system, a platelet-release reaction, and endothelial sloughing with subsequent activation of the intrinsic clotting cascade [25]. In our cases, bacterial sepsis possibly caused DIC as damaged colonic mucosa can result in transient bacteremia, which leads to gram-negative sepsis and that the small intestine is a relatively sterile environment, but we cannot find a blood culture result of the patients so this can be a recommended to be clarified.Our patients had classic laboratory findings of DIC. With the given pathophysiology and that in a case of acute gastroenteritis, what really triggers DIC? Shock of any etiology can give rise to DIC. Hypovolemic shock due to severe dehydration with hyperammonemia, hyperglycemia and hypernatremia is the potential cause of DIC in our patients based on the laboratory and clinical evaluation. The process likely begins either with endothelial damage, which activates the intrinsic coagulation pathway, or with a platelet-release reaction and subsequent activation of the procoagulant system. It is likely that DIC was a consequence of hypovolemic shock and its associated metabolic derangements. On the other hand, Pearson product-moment correlation coefficient was employed to validate if there is an association or relationship between the variables of this study. The first group of variables that was validated is the blood serum tests for DIC; serum electrolytes and acid base profile; and hematological and metabolic profile. The level of significance (2-Tailed) value of serum electrolyte and acid base balance profile, and blood serum tests for DIC is .029 which shows that there is statistically significant correlation between the two variables. This means that, increases or decreases in one variable do significantly relate to increase or decrease of the other. Moreover, the Pearson’s r (.760) value is close to 1 and it is (+), this strengthens the finding at which the relationship is positive and strong. Thus, once the value of serum electrolyte and acid base balance profile increases, the value of blood serum tests for DIC also increases and vice versa. Furthermore, it has been found that there is no statistical association or correlation between the serum electrolytes and acid base balance profile; and hematological and metabolic profile as per level of significance (2-tailed) value of .287 and Pearson’s r (-.431). The increase or decrease of the first variable do not significantly relate to increase or decrease of the other at which the relationship of the two variables is weak and negative. This means that, if the laboratory value of serum electrolytes and acid base balance profile increases; the laboratory value of hematological and metabolic profile decreases and vice versa. So the values of the two different laboratory tests go oppositely. This finding is just the same with that of the hematological and metabolic profile; and blood serum tests for DIC at its level of significance (2-Tailed) .225 and Pearson’s r (-.387).On the other hand, there is a statistically significant correlation between the laboratory evaluations for evidences of DIC and types of dehydration at the level of significance (2-Tailed) value of .000 and Pearson’s r (1.000). The result shows that the relationship is strong with positive association. Therefore, as the laboratory values of evidences of DIC increases, the dehydration also ascend to higher degree and vice versa. Looking into consideration the number of cases of patients with DIC according to the degree of dehydration, there is higher number that almost all with severe degree of dehydration has evidences of DIC than in with the moderate degree of dehydration. Moreover, there is no statistically significant correlation between evidences of DIC and type of dehydration as revealed by the computed value as per level of significance (2-Tailed) .512 at which an increase or decrease in the value of evidences of DIC do not significantly relate to increase or decrease in the value of laboratory tests for the type of dehydration but changes in the value of the first variable is correlated to the changes of the second variable as per computed value of Pearson’s r (.693). Lastly, there is a statistically significant correlation between the evidences of DIC and some metabolic profile at level of significance (2-Tailed) .010. This means that, the increase or decrease in the value of the first variable is significantly related to the increase or decrease of the other. Furthermore, the association is strong and positive as revealed by Pearson’s r (.990) which means that, changes in the values of laboratory tests for the evidences of DIC are strongly correlated with the changes in the values of the laboratory tests for some metabolic profile in a sense that as the values of first variable increases, the values of the second variable do the same. Similarly, as the first variable decreases in value, the second variable also decreases in value.
5. Conclusions
- Diagnosing a disease and identification of accompanying complications is a vital role of being a health care professional. Based on observations and in-depth analysis of data and through statistical treatment that was carried on laboratory and clinical evaluations of admitted pediatric patient diagnosed with acute gastroenteritis at Gharyan Central Medical and Teaching Hospital in Gharyan, Libya, the following conclusions were made: 1. Hypovolemic shock due to severe dehydration with hyperammonemia, hyperglycemia and hypernatremia is the potential cause of DIC in our patients based on the laboratory and clinical evaluation. 2. There is a strong positive association of serum electrolyte and acid base balance profile, and blood serum tests for DIC at which the increase or decrease in the laboratory values is significantly related to increase or decrease of the other. 3. There is no statistical association or correlation between the serum electrolytes and acid base balance profile, and hematological and metabolic profile. The increase or decrease in values of the first is not significantly related to increase or decrease of the other. This means that, if the laboratory value of serum electrolytes and acid base balance profile increases; the laboratory value of hematological and metabolic profile decreases and vice versa. 4. There is no statistical association or correlation between the hematological and metabolic profile; and blood serum tests for DIC. The increase or decrease in values of the first is not significantly related to increase or decrease of the other. This means that, if the laboratory value of serum electrolytes and acid base balance profile increases; the laboratory value of hematological and metabolic profile decreases and vice versa.5. There is a strong significant correlation with positive association between the laboratory evaluations for evidences of DIC and types of dehydration. Therefore, as the laboratory values of evidences of DIC increases, the dehydration also ascend to higher degree and vice versa. 6. There is a statistically significant correlation between the evidences of DIC and some metabolic profile at which the increase or decrease in the value of the laboratory tests for evidences of DIC is significantly related to the increase or decrease of the laboratory tests for some of the metabolic profile and the association is strong and positive.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML