-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2016; 6(2): 32-37
doi:10.5923/j.cmd.20160602.02

Clinical Indications of Magnetic Resonance Imaging in Suspected Malignant Breast Lesions
Naglaa M. Elsayed 1, 2, Rawan F. Abuzinadh 1, Wojood Ramadan 1
1Department of Diagnostic Radiology, Faculty of Applied medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia
2Department of Diagnostic Radiology, Faculty of Medicine, Cairo University, Cairo, Egypt
Correspondence to: Naglaa M. Elsayed , Department of Diagnostic Radiology, Faculty of Applied medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Breast cancer is the most frequently diagnosed life threatening cancer in females and the leading cause of cancer death among them. About one third of cancers in females arise in the breast. Magnetic resonance imaging (MRI) has been used as an important diagnostic tool for the breast, and the role of MRI in breast cancer is progressing. Many techniques are developed for beast MRI, the most useful of them is dynamic contrast enhanced technique. MRI improves the detection of primary and recurrent breast malignancy and evaluation of the response to treatment. It offers high sensitivity for the detection of multifocal and multicentric lesions, which is important in selecting patient candidates for conservative breast surgery. MRI is an ideal tool in screening young women with strong family history of breast cancer. Aim of work: The aim of our work was to study clinical indications for the use of MRI in suspicious malignant breast lesions, and its impact on patients' outcome. Materials and method: We collected data of 50 female patients who had breast MRI after mammography. The mean age was 44.5 years (range = 23-69 years). Patients presented with various clinical indications for breast MRI. Correlations of MRI findings with histopathology results were analyzed. Conclusions: The sensitivity of MRI in detecting malignant breast lesions was 90%. MRI showed statistically significant sensitivity for post-operative, post chemotherapy cases as well as in screening high risk patients.
Keywords: Breast, MRI, Sensitivity, Malignant, Dynamic, Screening, Mastectomy, Lumpectomy, Chemotherapy
Cite this paper: Naglaa M. Elsayed , Rawan F. Abuzinadh , Wojood Ramadan , Clinical Indications of Magnetic Resonance Imaging in Suspected Malignant Breast Lesions, Clinical Medicine and Diagnostics, Vol. 6 No. 2, 2016, pp. 32-37. doi: 10.5923/j.cmd.20160602.02.
Article Outline
1. Introduction
- All over the world, breast cancer is the most common life threatening cancer in females and the leading cause of cancer death among them. About one third of cancers in women arise in the breast, making it by far the most commonly diagnosed cancer after excluding basal and squamous cell carcinomas of the skin [1]. A great and continuous effort for prevention, diagnosis, and treatment has led to significant reduction of the mortality rate of breast cancer. In addition, breast cancer management has become increasingly complex, requiring full assessment and review of multiple issues including mainly imaging [2]. The most commonly used radiology imaging modality for breast cancer is mammography. It is used as a screening and diagnostic tool, and also to monitor surgical or chemotherapeutic intervention. However, it has many limitations i.e. poor imaging of dense breast, detecting small lesions or multicentric tumor foci. Recently, Magnetic resonance imaging (MRI) has become an important diagnostic tool for breast imaging, and its role in breast cancer assessment is growing. In addition to mammography and Ultrasound, MRI can be valuable to the work-up of suspected breast lesions or in the follow up of biopsy-proven malignancy [3]. The value of MRI of the breast is increasingly recognized by physicians and radiologists which lead to more clinical indications of this technology [4]. Improvements in MRI scanners, development of new techniques and pulse sequences and the use of rapid dynamic contrast studies have improved the image quality, and raised the sensitivity and specificity of MRI for breast cancers detection [5].Indications of breast MRI imaging include breast implants, where it can assess the implant itself with its possible complications e.g. rupture, and also the surrounding breast tissue where some small lesions may be obscured by the implant in the mammographic images. MRI is also useful for detecting small breast cancers, multifocal or multicentric lesions, staging breast cancer, selecting the most appropriate treatment whether total mastectomy or conservative surgery, and for patient follow-up after surgical treatment to exclude recurrence or residual lesions. Breast MRI also has high specificity in evaluation of tumor response to neoadjuvant chemotherapy [4, 6]. In addition to its role as a diagnostic tool, MRI has been extensively investigated as a useful tool in screening younger women at high risk of breast cancer, where mammography and Ultrasound may fail in detecting some lesions [4].
2. The Aim of Work
- The aim of this work is to study different clinical settings in which MRI is shown to be valuable in detecting malignant breast lesions, in addition to studying its sensitivity, diagnostic accuracy and its impact on the clinical outcome of patients.
3. Patients and Methods
- This study was done after obtaining an ethical approval from the research ethics committee.
3.1. Subjects
- The study included 50 female patients, ranging in age from 23 to 69 years with the mean age 44.5 years. Thirty-five patients were premenopausal, aged 23-49 years, while 15 patients were post-menopausal aged 50-69 years. All participants had bilateral mammography with at least two views for each breast before doing MRI. Additional breast Ultrasound was done for 24 patients. The indications for breast MRI included; suspected breast lesions on mammography to confirm or exclude malignancy and before biopsy decision (21 patients), post mastectomy or lumpectomy for malignant breast lesions to exclude recurrence or residual (12 patients), follow up patients after chemotherapy for breast cancer (4 patients), screening of patients with strong family history of breast cancer (10 patients), in addition to miscellaneous indications which were; breast implants with lump (1 patient), recent indrawing of the nipple (1 patient) and unilateral mastalgia (1 patient). We included only patients with clinical or mammographic suspected malignancy and cases under treatment from biopsy-proved malignancy. The exclusion criteria included patients with normal or benign looking lesions on mammography.
3.2. MRI Procedure
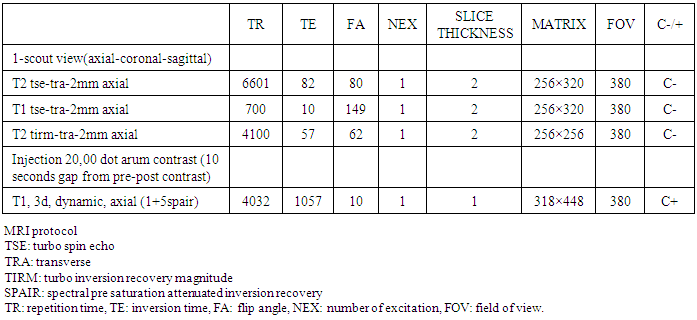
- The MR imaging was performed using a 1.5-T and 3-T magnet Siemens MRI machines in prone position with breast coil. No sedation was used. For premenopausal women, the best time to perform breast MRI was the second week of menstrual cycle. For postmenopausal patients, the examination was performed at any time. A written consent was taken from all participants. Table 1 summarizes the protocol parameters used.
|
4. Results
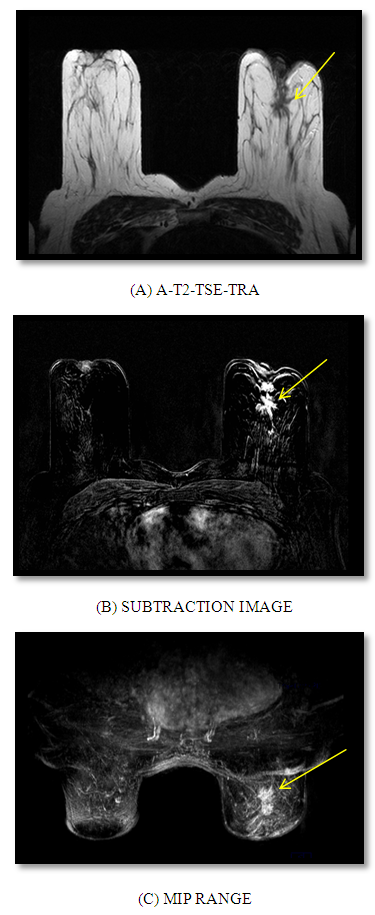
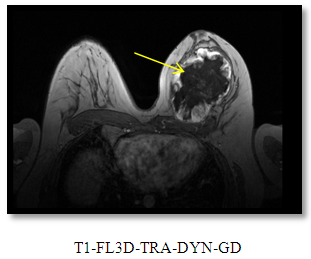
- We arranged the patients according to the clinical indications into 5 groups:Group 1: 21 patients with suspected malignant breast lesions on mammography. MRI was requested prior to biopsy and to exclude multiple lesions or lesions on the contralateral breast.Group 2: 12 patients with post mastectomy or lumpectomy to exclude recurrent or residual tumor.Group 3: Follow up of 4 patients after chemotherapy for breast cancer for suspected recurrence.Group 4: Screening of 10 females with strong family history of breast cancer with either suspected mammographic results or dense breasts in young ladies.Group 5: Miscellaneous case; one patient with breast implant and felt lump, one patient with mastalgia and one patient with recent indrawing of the nipple.The results were as the following:Group 1: MRI detected malignant lesions in all patients with suspected breast cancers; BIRADS IV in 12 patients, BIRADS V in 8 patients, and multicenteric lesions in one patient (Figure 1: A, B and C). These findings matched with the pathology in 19 cases (15 IDC, 2 DCIS and 2 ILC)*, while in two cases, the pathology was negative for malignancy. These 2 negative patients were diagnosed as BIRAD IV on MRI. MRI sensitivity was 90.4%.*IDC = intraductal carcinoma, DCIS = ductal carcinoma in situ, ILC = intralobular carcinoma
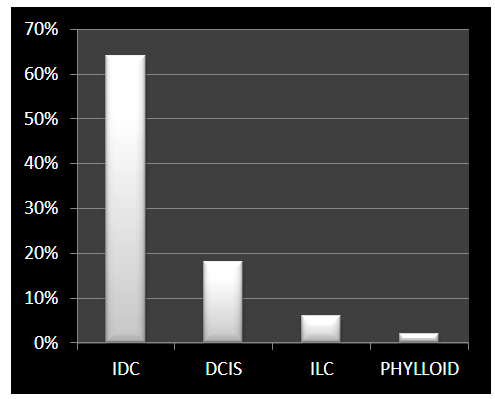 | Figure 4. Types and percentage of pathologically proved malignant breast lesions |
5. Discussion
- The current research shows that the overall sensitivity of MRI in detecting breast cancer is 90% which matches with what is mentioned in literatures where "the overall sensitivity of MRI for breast cancer has been proved to be relatively high, ranging from 85% to 100%" [7]. Among positive cases for malignancy in our study, IDC is the commonest detected malignancy (about 65%) followed by DCIS. In a study of Harms and Flamig, 1993, MRI sensitivity approaches 100% in detecting IDC [6]. MRI sensitivity for invasive lobular carcinoma and DCIS are lower than IDC [8]. It is mentioned in literature that "The detection of breast cancer with MRI is based on the fact that nearly 100% of invasive cancers will enhance after I.V. gadolinium injection. This is probably depends on the basis of invasive tumor angiogenesis. For in situ cancers, MRI detects only 40-100% of lesions. In other studies, the sensitivity for DCIS is probably in the 50% range", while the sensitivity for invasive breast cancers more than 3 mm is almost 100% [9, 10]. Dynamic contrast-enhanced MRI is an important technique in breast imaging. It shows high sensitivities up to 100% for IDC and 40% for DCIS [11, 12].MRI is done to evaluate breasts before biopsy in an effort to reduce the number of unnecessary biopsies for benign lesions and also to detect the possibility of multiple lesions [13, 14]. In young women with extremely dense breasts, multiple malignant foci could be easily missed by mammography, while MRI is significantly more sensitive in detecting such lesions. Multifocal or multicentric lesions may greatly affect the treatment plans of patients where conservative operation will not be optional. In our study, MRI could diagnose 3 multicentric lesions which were proved to be malignant by pathology. MRI breast has been used extensively more than before due to many reasons; many patients don't want to undergo a biopsy for a suspected lesion found in mammography or Ultrasound, doctors want to be very cautious in case of litigation, or because the abnormality has not been thoroughly worked up on mammography and Ultrasound [9, 10]. All our participants were referred for MRI of the breast as a mandatory imaging tool, either to exclude highly suspected malignancy before biopsy, to follow post-operative or post chemotherapy cases or for screening high risk females. Most of our participants aged less than 45 years. MRI is very beneficial for those young ladies with dense breasts because – in contrast to mammography- its sensitivity in detecting breast masses doesn't affected by breast density. Using MRI as a screening tool for breast cancer has been extensively studied. High risk females tend to develop breast cancer at a younger age when the mammography is not ideal tool due to increased breast density. Some authors mentioned that "breast cancer screening with MRI is associated with an increase in false-positive results that lead to more unnecessary biopsies" [15] and other studies stated that, "breast MRI for women at high risk for breast cancer development leads to a recommendation of biopsy in about 17% of cases, and cancer tends to be found in about 24% of those biopsies". [16, 17]. On the other hand, The American Cancer Society (ACS) recommends that all women with a greater than 20% lifetime risk of breast cancer should have MRI of the breast and mammogram every year starting at age 30 [5, 18]. It is mentioned in literatures that in high-risk women, MRI sensitivity for DCIS and IDC is 87% and 90% respectively [12, 19]. In our study, histopathology was positive for 80% of cases with strong family history of breast cancer and positive MRI findings, 50% proved to be DCIS. These findings are very close to the results of Kvistad et al, 2000 who found that more than 50% of MRI-detected breast cancers in high risk females were DCIS [20]. Other indications of breast MRI include post lumpectomy where MRI shows high sensitivity in detecting possible residual breast cancer in patients who have had conservative surgery with breast lump removed. MRI could detect the presence of very little amount of residual carcinoma at the operative margins. So, it helps to select patients for re-excision [21]. The sensitivity and specificity of MRI in detecting residual tumors after lumpectomy were100% in the study Cecil et al, 2001 [22]. Also after mastectomy, MRI has a great role to exclude recurrent tumors, or newly developed lesions on the contralateral breast. One of the most important diagnostic findings is that, after lumpectomy and radiation treatment, residual cancer will enhance, while inactive scar tissue will not. MRI after chemotherapy typically shows about a 75% correlation with histology and only 60% correlation to physical examination [10]. MRI is particularly useful in breast cancer patients who have not had a complete clinical response to the treatment [23, 24]. In the current study, MRI is correlated with histology results in 100% of patients where four patients having chemotherapy for breast cancer subjected to MRI. Malignancy was detected in all cases which was also proved by pathology. The variation in these percentages between our results and the previous one may be due to the few number of this group of patients in our research. MRI of the breast is not only important for accurately diagnose the tumor size, multifocality or multicentricity, local extent and distant spread - but also the presence of lymph node metastatic deposits which is essential in staging of cancer before treatment [25, 26]. Thirty percent of our patients have abnormal axillary lymph nodes in MRI. Out of them, 73% proved to be malignant by pathology, and this affects the staging and treatment plans of those patients. However, in our opinion MRI could not be used independently for breast imaging -in spite of its proved high sensitivity and specificity in many previous literatures- because it is expensive and sophisticated technique that makes it not suitable for all patients.
6. Conclusions
- MRI is highly sensitive in detecting malignant breast lesions which makes it an essential tool in breast imaging. However, it has some limitations that prevent its using widely, including its high cost compared to mammography and infrequent availability in many health facilities. The American Cancer Society's recent recommendation of MRI as a screening tool in young females at very high risk of breast cancer shows that this technology is beginning to play a more significant role in detecting breast cancer. An expanding study with a larger sample volume is needed to get better statistical results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML