-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2016; 6(1): 1-6
doi:10.5923/j.cmd.20160601.01

Effect of Noise on Neonatal Vital Data and Behavior in NICU
Hisham Ahmed Aly1, Ahmed Mohamed Ahmed2
1Department of Pediatrics, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
2Department of Audiology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Correspondence to: Hisham Ahmed Aly, Department of Pediatrics, Faculty of Medicine, Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

High sound pressure levels may be harmful to the maturing newborns. Current guidelines suggest that the sound pressure levels within a neonatal intensive care unit should not exceed 45 dB. It is likely that environmental noise as well as the noise generated by the incubator fan and respiratory equipment may contribute to the total sound pressure levels. Knowledge of the contribution of each component and source is important to develop effective strategies to reduce noise within the incubator. Aims: To identify if there is any changes of neonatal response behaviors and their vital signs when newborns exposed to noise or not. The study included 100 newborns. All newborns included in the study were subjected to complete neurobehavioral assessment using Brazelton neonatal behavior scale before and after exposure to noise. Also they were subjected to measurement of vital signs before and after noise and we compared between them. We used sound level meter to measure level of noise that newborn exposed to in NICU. We measured level of noise at different times of days and nights and reported the mean of all measures. Results: We had found that noise exposure causes significant behavioral changes, and changes of all vital signs expect temperature. We had found difference between pre-term and full-term of their vital signs and behavior before and after noise exposure. Conclusions: The current study had shown that noise exposure in NICU has some negative drawbacks on vital signs and behavior of neonates.
Keywords: Neonatal, Behavior, Noise
Cite this paper: Hisham Ahmed Aly, Ahmed Mohamed Ahmed, Effect of Noise on Neonatal Vital Data and Behavior in NICU, Clinical Medicine and Diagnostics, Vol. 6 No. 1, 2016, pp. 1-6. doi: 10.5923/j.cmd.20160601.01.
1. Introduction
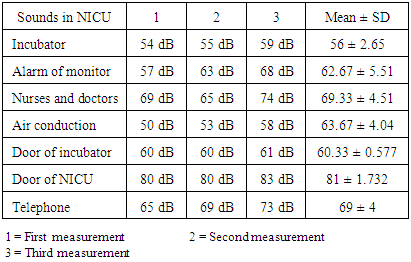
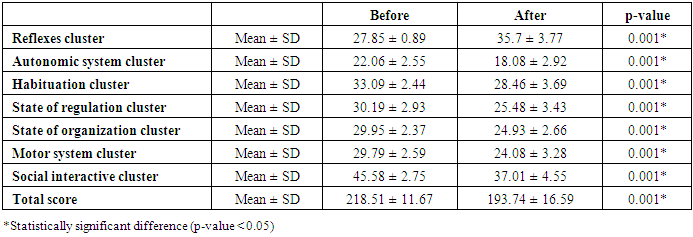
- Noise is any sound – independent of loudness – that may produce an undesired physiological or psychological effect in an individual. [1]The goal for neonatal intensive care unit (NICU) is to provide an environment that promotes sleep, supports neonatal physiologic stability, and reduces potential adverse effects on the auditory development of newborn infants. [2] There is a growing concern that such noise puts newborn at high risk for adverse health effects. Loud transient noise has negative short-term effects on the cardiovascular and respiratory systems of newborn infants. [3]The NICU is often characterized by loud, unpredictable noise from extraneous sources such as alarms, ventilators, phones and staff conversation to which newborn infants are especially vulnerable. [4]Some studies conclude that the average sound levels in a NICU ranges anywhere between 70 to 80 dB. The American Academy of Pediatrics (AAP) recommends a maximum safe noise level of 45 dB in a NICU. Failure to maintain noise levels under the maximum levels recommended by AAP may result in numerous adverse noise-induced health effects on premature babies as they are very fragile. [3]Aim of the work:The aims of this study were to: - Identify sound characteristics in NICU that disrupt sleep, increase episodes of tachycardia, or desaturation and disrupt all vital data in newborn infants.- Examine if there is any changes of neonatal response behaviors when newborns exposed to noise or not. - Examine if there is any changes of vital signs when newborns exposed to noise or not.Patients and methods:The current study was designed as an interventional pre and posttest study with aim to evaluate the effect of noise exposure on vital signs (including heart rate, blood pressure, respiratory rate, temperature and oxygen saturation) and neonatal behavior among neonates admitted to NICU.This study included 100 newborn chosen from Sayed Galal University Hospital, at period from February 2013 to January 2014 at different times of days and nights, and at different gestational age and birth weight. They were classified into two groups:Group 1: 100 (males (70%) and 30% females) with more than half of them were preterm with gestational age less than 37 weeks (55%). This group not exposed to noise.Group 2: The same above newborn but after we exposed them to noise ranging from 60 – 130 dB for about 10 minute.Inclusion criteria were:1 – Mild neonatal jaundice (in phototherapy range).2 – Mild neonatal sepsis3 – Mild neonatal respiratory distress4 – Growing baby include preterm and IUGR.Exclusion criteria were:1 – Sever neonatal sepsis.2 – Hypoxic ischemic encephalopathy.3 – Kernictrus or any CNS abnormality.4 – Newborn on drugs affecting hearing such as aminoglycoside.All newborn were subjected to the following:1- History taking with special emphasis on gestational age, birth weight, maternal health, mode of delivery, consanguinity and type of feeding.2- Detailed clinical examination to diagnose the presence of postnatal complications e.g. perinatal asphyxia, hemorrhage, malformations or suspected metabolic disease.3- Measurement of vital sign (heart rate, respiratory rate, blood pressure, temperature, oxygen saturation) before and after noise and we compared between them.4- Complete neurobehavioral assessment using brazelton neonatal behavior scale before and after exposure to noise and we compared between them.Brazelton Neonatal Behavioral Assessment Scale (BNBAS) includes 27 behavioral items, each scored on 9-points scale and 16 elicited reflexes scored on 5-point scale. The infants neurobehavioral performance is summarized according to 7clusters including (social-interactive, motor behavior, state organization, regulation of state, habituation, autonomic stability and reflexes cluster). (Brazelton and Nugent., 1995).5- We used sound level meter to measure level of noise that newborn exposed to in NICU. We measured level of noise at different times of days and nights and reported the mean of all that measures.We measured noise by sound level meter through putting sound level meter at the head of newborn and measured every sound alone by exclusion of other sounds. Note that newborn may be exposed to more than one sound. In our study newborns were exposed to noise ranging from 54 -83 dB for about 10 minute.
|
2. Results
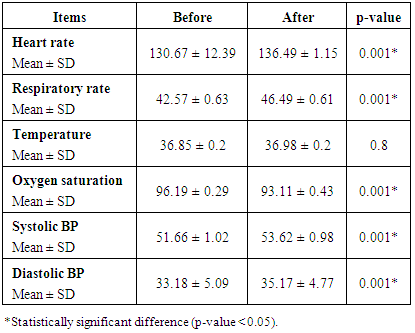
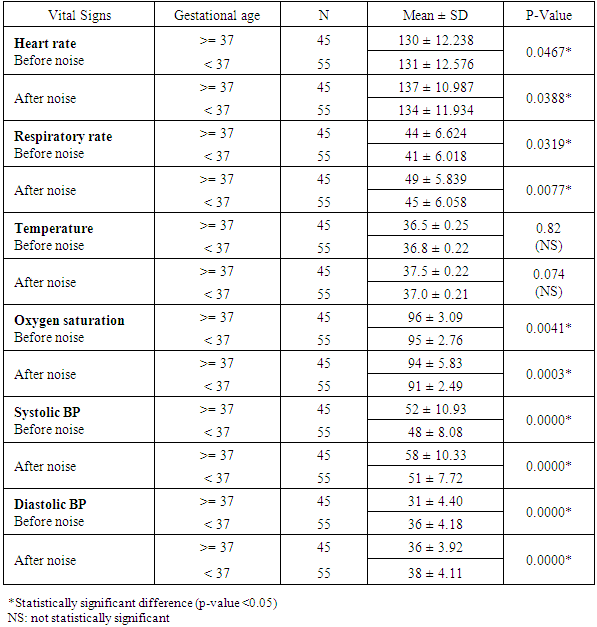
- There was significant increase of heart rate, respiratory rate, systolic and diastolic blood pressure. There was significant decrease of oxygen saturation among the studied neonates due to noise exposure. Only temperature didn't show significant change with noise exposure.
|
|
|
3. Discussion
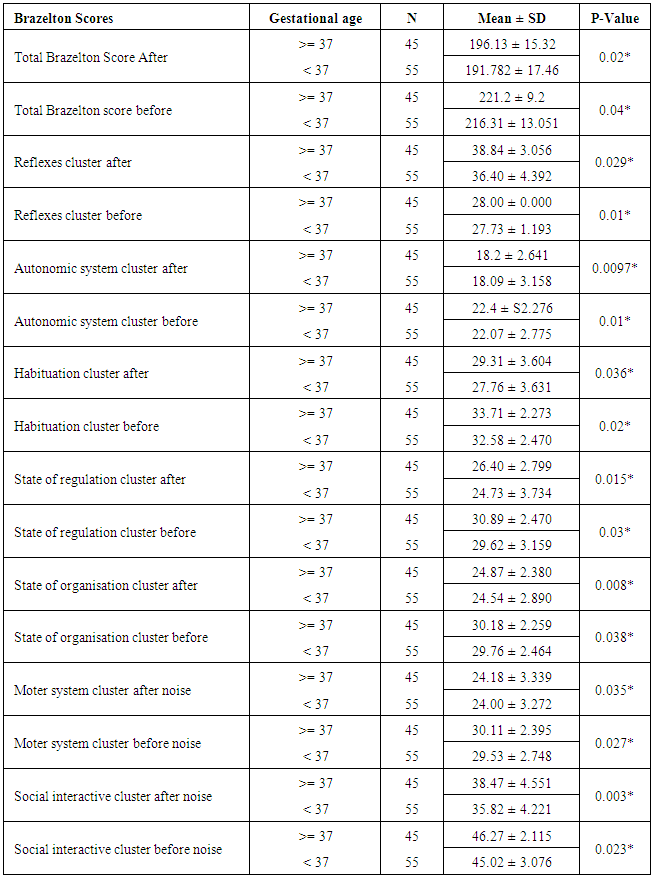
- As increasing numbers of survivors reach school age, more minor impairments cause concern; difficulties with attention, behavior, language performance, and academic skills are becoming apparent. [5]It has been suggested that the persistence of these developmental problems may be associated with the NICU environment. [6] One possibility is that the impairments emerging in school-age children may be the consequence of noise and light stimulation of the NICU environment exceeding the capacity of the preterm infant's central nervous system to cope with it. [7]It is well documented that high noise levels are harmful to preterm infants and result in increased physiologic stress. Even brief stimulation from alarms and telephones can result in an increase in autonomic response with a subsequent physiologic decline that puts the infant at risk for both bradycardia and hypoxic episodes. Bremmer Byers, Kiehl (2003), [8] Documented physiologic changes include apnea, bradycardia, alterations in sleep-wake states and fluctuations in heart rate, respiratory rate, blood pressure, and oxygen saturation. [9]According to the current study, it was found that noise exposure causes significant increase of heart rate, respiratory rate, systolic and diastolic blood pressure (table 5). These findings are inconsistent with the available reports in the previous papers. [9], [8].
|
|
4. Conclusions
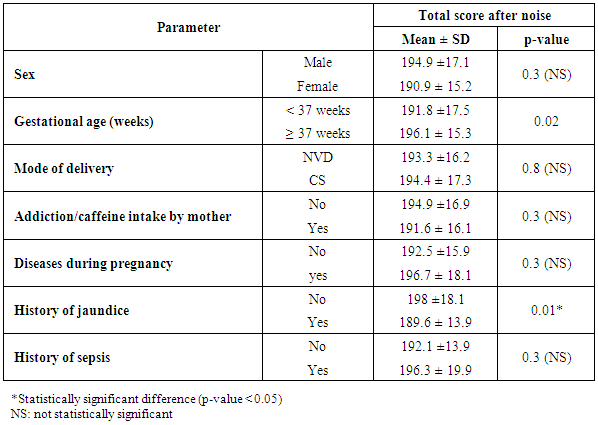
- 1 - The current study had shown that noise exposure in NICU has some negative drawbacks on vital signs and behavior of neonates. 2- We had found significant changes of vital signs of newborns before and after noise.3 - We had found significant changes of neonatal behavior before and after noise.4 - Their was differences between preterm and full term of their vital signs and behavior before and after noise exposure.5 - Neonates with neonatal jaundice had more severe impact of noise on these neonates.
Recommendations
- Based on our results we recommend the following:1. NICU environment is an important determinant of neonatal outcome in NICU.2. Noise exposure in NICU should be evaluated routinely and reduced as much as possible.3. Newborns with neonatal jaundice and preterm should be placed in the most quite place in NICU.4. Doctors and other caregivers making morning rounds should discuss patient’s care plan away from the bedside of neonate. 5. All staff members involved in neonatal care will take a developmental care course that addressed the importance of management of the environment. The nurses should be educated about reducing conversation by the bedside. 6. All incubators should have acoustical foam placed in them to reduce the amount of noise inside the incubator.7. In all NICU units, walls and trash cans should be padded and ceilings should have acoustic tiles. 8. Pregnant woman should work in quite place as fetus will be affected by noise.9. All NICU doors and drawers should be padded.10. Further studies that evaluate the long term effects of noise exposure on neural development should be conducted.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML