-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2015; 5(6): 107-113
doi:10.5923/j.cmd.20150506.01

Medication Non Adherence in Schizophrenia: Prevalence and Correlates among Outpatients in a Tertiary Healthcare Facility in Uyo, South-South Nigeria
Jombo Henry Effiong1, Kufre Albert Umoh2
1Department of Psychiatry, Faculty of Clinical Sciences, University of Uyo, Uyo, Nigeria
2Department of family Medicine, Faculty of Clinical Sciences, University of Uyo, Uyo, Nigeria
Correspondence to: Jombo Henry Effiong, Department of Psychiatry, Faculty of Clinical Sciences, University of Uyo, Uyo, Nigeria.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

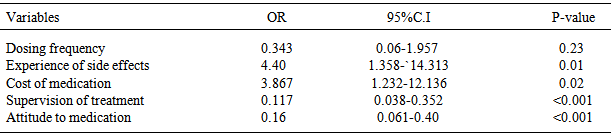
Background: Treatment non adherence in patients with schizophrenia is the main reason for frequent relapses, poor treatment outcome, reduced quality of life and significant increases in healthcare cost. Objectives: This study was conducted to determine the prevalence of treatment non adherence in patients with schizophrenia and identify factors associated with it. Method: One hundred and twenty patients with schizophrenia receiving treatment in the mental health unit were randomly selected to participate in the study. Data were collected using a socio-demographic questionnaire, the 8-item Morisky medication adherence scale (MMAS-8), Drug attitude inventory (DAI-10), Positive and Negative Symptoms Scale (PANSS). Logistic regression was used to determine significant variables associated with suboptimal adherence to medication. Results: Theprevalence of treatment non-adherence was 51.7%. The factors significantly associated with treatment non adherence were a poor attitude to medication (OR 0.067,95%CI0.012-0.387, P-value 0.03) lack of supervised treatment (OR 0.117, 95%CI 0.038-0.352, P-value <0.001) experience of side effects (OR 4.40, 95%CI= 1.358-14.313 p-value 0.01). Cost of medication (OR 3.867, 95%CI 1.232-12.136) and a high negative PANSS score (t=-1.91, P value 0.04) Conclusions: Adherence to antipsychotic medications among patients with schizophrenia is suboptimal. The findings strongly recommend the need to develop a standard protocol for carrying out adherence counselling to all patients and their relatives.
Keywords: Schizophrenia, Antipsychotics, Adherence, Nigeria
Cite this paper: Jombo Henry Effiong, Kufre Albert Umoh, Medication Non Adherence in Schizophrenia: Prevalence and Correlates among Outpatients in a Tertiary Healthcare Facility in Uyo, South-South Nigeria, Clinical Medicine and Diagnostics, Vol. 5 No. 6, 2015, pp. 107-113. doi: 10.5923/j.cmd.20150506.01.
Article Outline
1. Introduction
- Schizophrenia is a chronic mental disorder that causes prominent psychological dysfunction. It is one of the top 10 causes of long–term disability in the world. It affects about 1% of the population worldwide [1]. It is characterised by psychotic symptoms and runs a chronic course often resulting in repeated hospitalisation and a low quality of life [2]. Antipsychotic medications represent the cornerstone of pharmacological treatment for patients with schizophrenia. Although these agents have been shown to improve psychopathology, reduce relapse, improve functioning, non-adherence to treatment is common. Non adherence rates range from 20% to 89% with average of 50% reported in the literature [3, 4].In the treatment of psychiatric disorders, non adherence may be defined as a failure to enter a treatment programme, premature termination of treatment or incomplete implementation of instructions including those that pertain to medication administration [5]. Medication non adherence is the best predictor of relapse after a psychotic episode [6] and thus is an important clinical and public health issue.Previous studies have shown factors associated with non-adherence to medical treatment. These factors are patient related factors, medication related factors and factors related to social and medical support. [7] Patient’s factors include age, economic status and health beliefs about medication. [8] Social and Medical support factors include among others family help and support and patient-healthcare provider relationship. Medication related factors take into account the attitude towards medicines, the complexity of the medication regimen, and the experience of side effects [9].Generally, drug compliance in patients with schizophrenia is predicted by the patients’ subjective response to and attitude towards medication [10-12]. Positive attitude of patients towards treatment can improve therapeutic alliance, medication compliance and long term prognosis [13]. Attitude towards antipsychotic medication is significantly affected by factors such as lack of insight into the illness [14], degree of global psychopathology [14], and side effects of medications [15, 16]. This study was conducted to determine the prevalence of treatment non adherence in patients with schizophrenia and identify factors associated with it in my environment.
2. Materials and Methods
2.1. Location of the Study
- This study was conducted at University of Uyo Teaching Hospital from July 2014 to November 2014. The hospital is located in Uyo, the capital city of Akwa Ibom State, Nigeria. The hospital is a 450 bed capacity tertiary healthcare centre that offers secondary and tertiary care. It receives referral from primary and secondary healthcare facilities in the state as well as from the neighbouring states.
2.2. Subjects
- The sample size was calculated using a public domain software available on-line (www.statpages.org) [17] using a prevalence of treatment non adherence as determined from previous studies (52%) [18] The sample consisted of one hundred and thirty two (n=132) patients with schizophrenia who were randomly selected based on the table of random number on each clinic visit. A subject was enrolled if he/she met the following inclusion criteria: a diagnosis of Schizophrenia, subjects who had been on medications for at least one year prior to study entry, adults above the age of 18years, and who granted consent. The exclusion criteria were: current florid psychopathology capable of impairing response and co morbid psychoactive substance use or physical disorders.
2.3. Procedure
- Approval for the study was obtained from the Research and Ethical Committee of the University of Uyo teaching Hospital. Informed consent was obtained from patients and their accompanying family members. Patients who met the inclusion criteria were recruited into the study after a comprehensive psychiatric evaluation and diagnosis by resident doctors in psychiatry. The Mini International Neuropsychiatric Interview (MINI) English Version 5.0.0 [19] was further used to confirm the diagnosis of schizophrenia in the participants. The MINI was designed as a brief structured interview for the major Axis 1 diagnosis in the Diagnostic and Statistical Manual (DSM-IV) [20] and ICD-10.
2.4. Measures
2.4.1. Semi-structured Questionnaire
- A questionnaire designed by the authors was used to obtain information Measures evaluated included socio-demographic details (age of the patient and family member, gender, educational status, marital status, religion, monthly family income, place of stay, occupation), attitude towards medication, illness related variables (total duration of illness, severity of illness,) and medication related variables (number of tablets taken per day, cost of monthly medication, supervision of medication, type of medication, side effects of medication).
2.4.2. Medication Profile
- The medication profile of each respondent was obtained through review of the medication record files domiciled in the hospital. Data recorded include: The number of antipsychotic medicines on the patients treatment regimen, the class of medication, the frequency of intake of medication. The side effects of medication.
2.4.3. Morisky Medication Adherence Scale (MMAS)
- The compliance level of patients was defined by the application of the MMAS-8. The MMAS is a reliable and validated 8 items; self reported measure of medication use patterns. Each item on the MMAS measures a specific medication-taking behaviour. Each of the item is presented in a “yes or no” format. These involve asking the patient about the extent and tendency to forget to take their medication and their discontinuance of medication treatment upon feeling that their condition has improved or worsened. Answers were scored as 0 or 1, with score 1 corresponding to positive answers. The item scores obtained from the MMAS are summed to indicate an overall level of medication adherence [22]. The MMAS scores range from zero to eight and have been stratified into three levels to classify adherence levels: high adherence-MMAS score of 8, moderate adherence-MMAS scores of 5 to 7 and low adherence-MMAS score of less than or equal to 4.
2.4.4. Positive and Negative Symptoms Scale (PANSS)
- Severity of illness was measured using positive and negative syndrome scale (PANSS) [23]. It is a 30-item scale. Seven constitute a positive scale, seven a negative scale, and the remaining sixteen a general psychopathology scale. For each item, ratings are made on a 1–7 scale of increasing levels of psychopathology ranging from absent to extreme. The scores for the scales are arrived by summation of ratings for the component items. The Interrater reliability was established (r=0.82).
2.4.5. Drug Attitude Inventory (DAI 10)
- The attitude towards antipsychotic medication was assessed using 10 item drug attitude inventory (DAI). It is a self report questionnaire consisting of true/false statements about the perceived effects and benefits of antipsychotics with which the patients can agree or disagree. Each item ticked ‘yes’ is rated +1 and items ticked ‘no’ is rated as -1. The positive scores and negative scores are calculated and the total score will be positive score minus negative score. The positive total score indicates positive attitude and negative total score indicates negative attitude towards antipsychotic medications [24].All the questionnaires were translated into Ibibio language separately by two bilingual translators. The two versions were combined and revised and then back translated into English by another bilingual translator. The translation was refined after back translation until agreement was obtained among the four people involved in the translations.Data AnalysisDescriptive statistics such as frequencies, median, mean and standard deviation were computed for socio-demographic and clinical characteristics of the participants and other variables as appropriate. Relevant inferential statistics such as chi-square and t-test were used to determine the relationship between outcome and independent variables. Significant variables were entered into a regression analysis to determine predictors of attitude to medication and treatment adherence. Significance was computed at p < 0.05.
3. Results
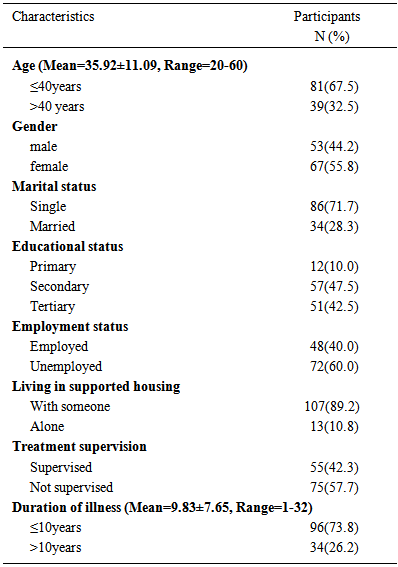
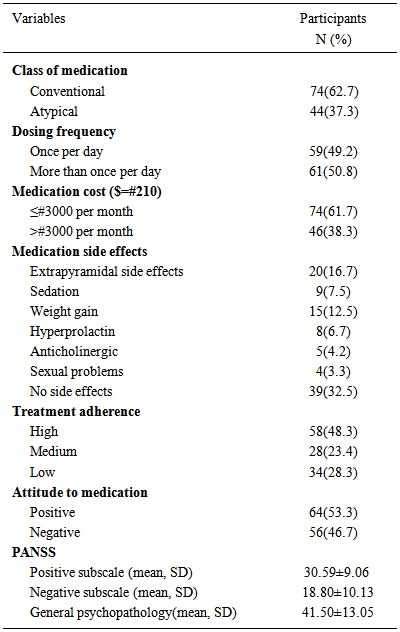
- Of the 132 participants in the study, 12 had incomplete data, so the result of 120 subjects was used for analysis. Females constituted (55.8%) of the subjects. The majority were single (71.7%) and unemployed (60.0%). Most of the subjects (57.5%) had secondary education as the highest level of education attained (Table 1).
|
|
|
|
|
4. Discussion
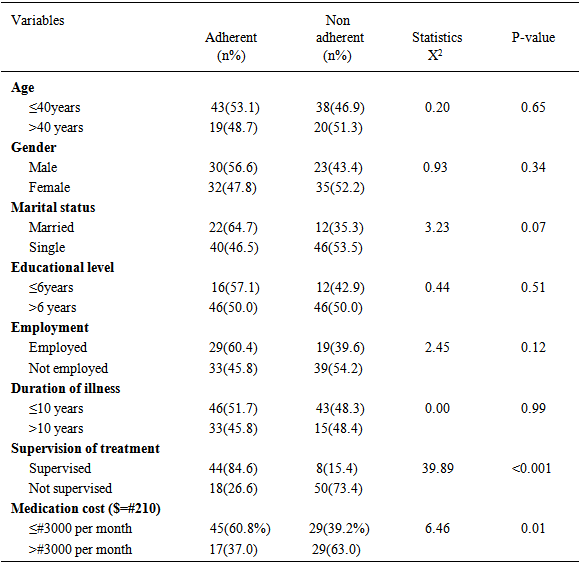
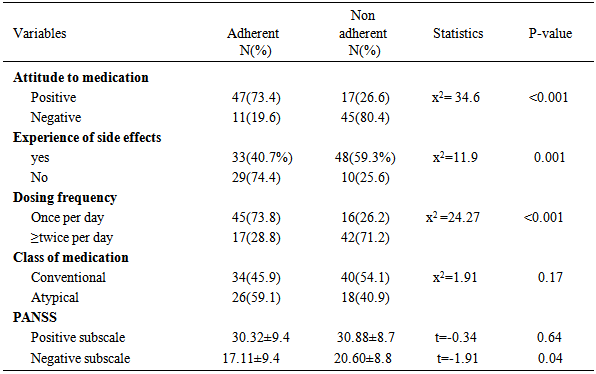
- The prevalence of treatment non-adherence in this study was 51.7% indicating that almost one in two patients were non-compliant with their medications. Similar rates have been reported in studies conducted in other regions of Nigeria [19, 25]. Studies conducted in other countries have indicated that over 60% of patients with schizophrenia were non compliant with medication [26, 27, 28]. The variations in the reported rates of treatment non adherence between these studies may be due to differences in the methods used in estimating adherence, different cut-off values and some peculiar characteristics of the study populations. Nevertheless, this level of non adherence is bound to translate to increased morbidity, relapses and rehospitalisation and increased cost burden of management. In this study, socio-demographic variables of the participants had insignificant impact on treatment adherence. Some subjects’ characteristics were found to influence treatment adherence to varying degree but their impact were not significant statistically. In previous studies, demographic variables have not been consistently associated with medication non compliance. Present study results are in support of the previous findings that there is no significant relationship of adherence with gender [29], age and marital status [30]. Although patients who were less than 40 years of age, who were married and who were employed were more likely to be adherent to treatment though, their impact were not statistically significant. We found a significant association between attitude to medication and treatment adherence. Previous study had reported that attitude to medication was an indirect representation of adherence to treatment [31]. We found an average level of general positive attitude to medication among patients with schizophrenia. Subjects with positive attitude were significantly more likely to adhere to medication compared to those with poor attitude. Previous studies showed some features of mental disorders which were significantly associated with attitude to medication like having insight, the degree of psychopathology and the side effects burden of medication [11-13]. It has also been reported that beliefs regarding the need for treatment and the benefit of treatment may affect medication adherence in a patient [31]. In this study, the degree of involvement of relatives in the management of patients and the dosing frequency of medication were significantly associated with positive attitude to medication. Also, from a cultural perspective, the patients’ belief systems and cultural values may be associated with poor attitude to medication and non-adherence since some patients may prefer traditional spiritual healing over conventional medical treatment. The belief in spiritual causation of mental disorders may influence patients and their caregivers help seeking behaviour and attitude to medication in believing that a spiritual solution is required to resolve their mental health problems and therefore treatment with orthodox medicine becomes futile [19]. However, the degree of positive attitude observed in this study may be related to more discernable improvements in treatments outcomes in orthodox setting compared to the treatment outcomes in religious and traditional medical settings. The degree of psychopathology has been cited as an important reason for poor attitude to medication and treatment non adherence. We found a significant association between the degree of negative symptoms and treatment adherence. Previous studies had reported that higher positive symptom, PANSS score predicts noncompliance. [31] Fenton et al reported in their study that the severity of psychopathology and failure to respond to treatment are associated with non adherence to treatment [32]. In this study, increased negative symptoms was a risk factor for non adherence. This partly can be attributed to the social, emotional withdraw and lack of volition seen in these patients which may impair their ability to comply with medication. Social support may become crucial to enhance treatment adherence. The availability of family or friends to assist or supervise medications has been consistently associated with outpatient adherence [33]. In this study, patients who were supervised at treatment were significantly more likely to adhere to medication compared to those who were not supervised. This outcome seems related to the fact that relatives’ involvement in treatment will ensure compliance with treatment and regular long term follow up management.The role of medication related variables in adherence was also explored in this study. The independent medication-related predictors of non adherence found in this study were; the cost of the medications, the dosing frequency and the side effects profile. The side effects burden has been reported as an important reason for treatment non compliance [10]. Casey noted that for many patients, extra pyramidal side-effects (EPS), weight gain, and sexual dysfunction are especially likely to decrease adherence [34]. Our finding is in agreement with studies that have found a significant relationship between extra-pyramidal side-effects [10, 33] and in disagreement with those studies that found no such relationship [35].In terms of the cost of the medications, the higher the cost of the medication per day, the higher the rate of non-adherence. This partly may be due to the observation in this study that a high proportion of participants (60.0%) were unemployed and majority (57.5) were observed to have had less than 12 years of formal education implying that most patients with schizophrenia are from a low socioeconomic background. This implies that limited financial resources are available to fund medicare especially as funding for healthcare in mainly out-of-pocket in the absence of comprehensive health insurance scheme in a resource poor setting like ours. This study has some limitations. Self reports were utilized in the assessment and measurement of medication adherence; this may occasionally be unreliable and biased. This is due to self reported measures being subject to recall bias and recall difficulties. The cross sectional nature of the study cannot establish causality. Therefore the value may remain exploratory. Also, standardised measures were not used in determining the side effects profile of the subjects.In conclusion, this study has shown that the level of adherence to treatment is suboptimal among out-patients with schizophrenia in our setting and that strategies that encourage family member’s participation in patient’s management will significantly improve treatment adherence.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML