-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2015; 5(3): 45-49
doi:10.5923/j.cmd.20150503.03
The Prevalence of Cryoglobulinaemia in Patients with Non-Hodgkin’s Lymphoma and Relation to Hepatitis C Virus and Positive Rheumatoid Factor Patients
Karima Abd Elhalim Mohammed Mahfouz, Nagwa Mohammed Abd Elmoneim Mowafy, Mohammed Abd Elhameed Basiony Khedr, Mohammad Mohammed Aamer
Clinical pathology department, Faculty of medicine (Boys), Al-Azhar University, Cairo, Egypt
Correspondence to: Mohammed Abd Elhameed Basiony Khedr, Clinical pathology department, Faculty of medicine (Boys), Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Non-Hodgkin’s Lymphoma (NHL) represents a group of diverse disease that varies in clinical behavior and morphological appearance. The various types of NHL can be correlated to neoplastic lymphoid cells that are arrested at different stages of normal differentiation. Cryoglobulins (CRs) are special serum immunogloblulins that precipitate at temperatures below 37°C but mostly at 0 - 4°C, and that dissolve when re-warmed to 37°C. Mixed cryoglobulinemia is classified among the systemic vasculitis in the subgroup of small vessel vasculitis. Methods: The study population consists of 20 patients (10 women and 10 men; mean age, 55 years; range, 36-75 years) diagnosed as Non Hodgkin lymphoma and 5 presumably healthy controls. Patients referred to the AL- HUSSEIN UNIVERSITY HOSPITAL. There was no exclusion criteria for age, gender, or underlying diseases. Results: showed that the incidence of cryoglobulinemia in NHL patients is 25%, type I 5%, type II 15% and type III 5%. This classification depend on speed of cryprecipitation during 24 hours in type I, within 48 hrs in type II and within 7days in type III. And according to monoclonality and polyclonality detected by serum protein electrophoresis. Conclusions:prevalence of cryoglobulinemia 25%, 60% of these positive cryoglobulinemic cases were HCV positive while 40% were HCV negative. The NHL cases giving positive cryoglobulin were of B cell type.
Keywords: Cryoglobulinaemia, Non-Hodgkin’s lymphoma, Rheumatoid factor, Hepatitis C Virus
Cite this paper: Karima Abd Elhalim Mohammed Mahfouz, Nagwa Mohammed Abd Elmoneim Mowafy, Mohammed Abd Elhameed Basiony Khedr, Mohammad Mohammed Aamer, The Prevalence of Cryoglobulinaemia in Patients with Non-Hodgkin’s Lymphoma and Relation to Hepatitis C Virus and Positive Rheumatoid Factor Patients, Clinical Medicine and Diagnostics, Vol. 5 No. 3, 2015, pp. 45-49. doi: 10.5923/j.cmd.20150503.03.
Article Outline
1. Introduction
- Non Hodgkin’s Lymphoma (NHL) represents a group of diverse disease that varies in clinical behavior and morphological appearance. The various types of NHL can be correlated to neoplastic lymphoid cells that are arrested at different stages of normal differentiation [1].The recent World Health Organization (WHO) classification based on REAL; subdivide all lymphoid malignancies as well as lymphomas according to characteristic morphological, immunophenotypic, genetic and clinical features. Previously, The Working Formulation, originally proposed in 1982, classified and grouped lymphomas by morphology and clinical behavior (ie, low, intermediate, or high grade). The low-grade disorders are relatively indolent, respond well to chemotherapy but are very difficult to cure whereas high-grade lymphomas are aggressive and need urgent treatment but are often curable. In 1994, the Revised American European Lymphoma (REAL) classification was published and gained widespread application [2, 3].Staging is important in selecting a treatment and also for prognosis. In addition to staging, risk stratification is important in patients with NHL. Several scoring systems had been developed and validated prospectively in patients with diffuse large B-cell lymphoma (International Prognostic Index, IPI) or follicular B-cell lymphomas (Follicular Lymphoma International Prognostic Index, FLIPI) that can be used to predict the prognosis of patients with B-cell malignancies [3].Cryoglobulins (CRs) are special serum immunogloblulins that precipitate at temperatures below 37°C but mostly at 0 - 4°C, and that dissolve when re-warmed to 37°C [4].The majority (95%) of CRs are immune complexes that contain rheumatoid factor (RF). Such CRs are known as mixed” cryoglobulins to differentiate them from the CRs with monoclonal bands that do not contain RF or antigen-antibody complexes. The antigens present in the mixed complexes may include RNA and proteins (eg, hepatitis C virus proteins). A small fraction of CRs (5%) comprise pure monoclonal gammopathies, which have poor solubility at low temperatures because of their unique amino acid sequences. There are also other cryoproteins that precipitate in the cold, such as cryofibrinogen (in plasma) and fibronectin [5].Aim of the work: Studying the prevalence of cryoglobulinemia in patients with NHL.
2. Patients, Material and Methods
- The study population consists of 20 patients (10 women and 10 men; mean age, 55 years; range, 36-75 years) diagnosed as Non Hodgkin lymphoma and 5 presumably healthy controls. There was no exclusion criteria for age and gender, or underlying diseases. The patients were subjected for the following investigations.• CBC by sysmex KX 21N, ESR by westergren method.• Liver function tests (ALT and AST by kinetic method, Total protien by biuret method, Albumin by BCG method).• Kidney function test (CREATININ by Jaffe method), all were done by HITACHI 912 autoanalyzer.• Viral markers (HBsAg, HCVAb) by ELISA.• RF by latex method.• ANA by Immunoflourescence.• BONE MARROW examination was done to assess infiltration• Testing for cryoglobulinemia was carried out in 2 stages:The first stage involves an initial screening for cryoprecipitation in serum, in which a precipitate is demonstrated to be primarily immunoglobulin and is largely resolubilized by warming. This step is most useful when coupled with quantitation of the level of cryoglobulin in the sample.The second stage requires more detailed characterization and typing of the cryoglobulin by immunofixation analysis and, in the case of type I and type II cryoglobulins, a review or performance of other standard laboratory testing for monoclonal gammopathy.In our study sera were assessed for cryoglobulins, where 10 ml of blood was drawn while the patient was in the fasting state (since lipids may interfere with the test), into a tube without anticoagulant. The syringe was also preserved in an incubator at 37ºC. The serum was separated by centrifugation at 37ºC and placed in a 4ºC refrigerator in two tubes, one simple and another Wintrobe tube to see if precipitation occurs over a 48-hour to a seven-day period [4]. In the present work the type of cryoglobulin was determined by speed of cryoprecipitation and associated laboratory findings (HCV Ab and rheumatoid factor).• Serum protein electrophoresis was done by gel electrophoresis by (Helena / Bioscinces Europe) for all cases and in positive cases the electrophoresis was done to the cryoprecipitate to detect if the change in gamma globulin in serum was due to presence of cryoglobulin (Figure 1, 2, 3 and 4)
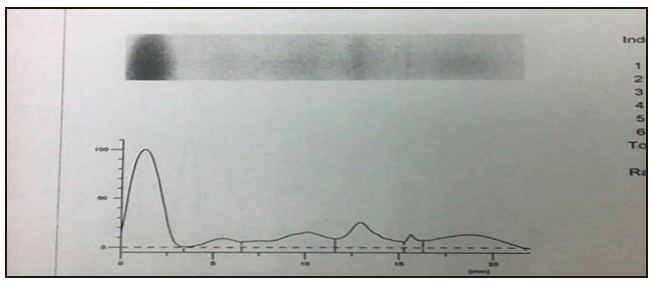 | Figure 1. Serum protein electrophoresis (Normal control) |
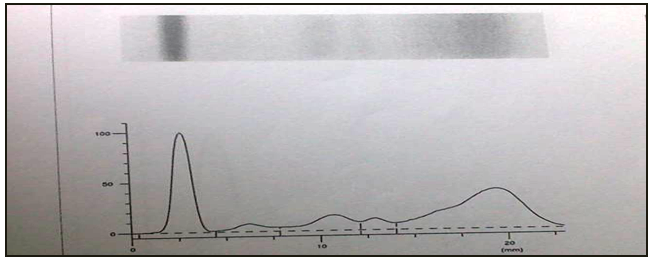 | Figure 2. Serum protein electrophoresis (polyclonal hypergammaglobulinemia), and positive cryoglobulin type II |
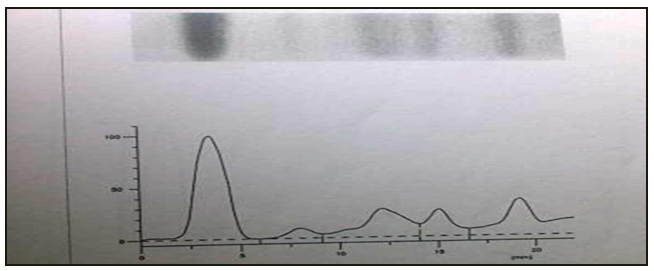 | Figure 3. Serum protein electrophoresis (Monoclonal hypergammaglobulinemia whole serum), and positive cryoglobulin type I |
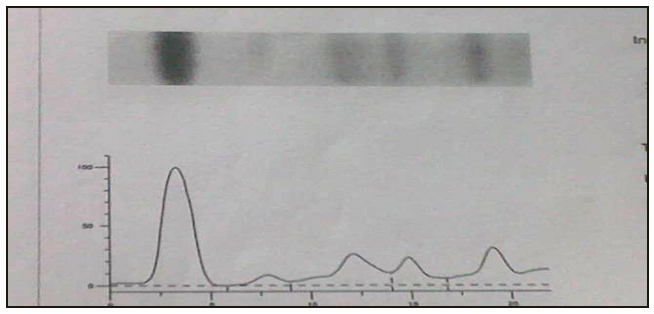 | Figure 4. Serum protein electrophoresis (Monoclonal hypergammaglobulinemia cryoprecipitate), and positive cryoglobulin type I |
3. Result
- • ANA is positive in 5% of cases while in +ve cryoglobulinemic pt is 20 %. Anemia is present in 75 % of all patients while in +ve cryoglobulinemic pt is 60%. Thrombocytopenia is present in 25 % of all patients, while in +ve cryoglobulinemic pt is 40%. Thrombocytosis is present in 4% of all patients. Leucopenia is present in 20% of all patients. ESR is markedly elevated in 15% of patients, while in +ve cryoglobulinemic pt is 40% .ALT is elevated in 30% of all patients, while in +ve cryoglobulinemic patients is 20%. AST is elevated in 40% of all patients, while in +ve cryoglobulinemic patients is 40% (Table 1).
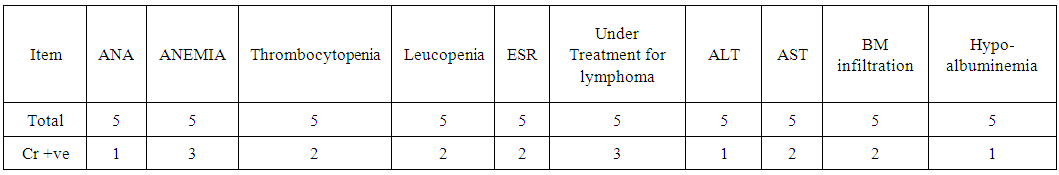 | Table 1. Correlation between cryoglobulinemia and ANA (anemia, Thrombocytopenia, leucopenia, ESR, ALT, AST, BM infiltration and hypoalbuminemia) |
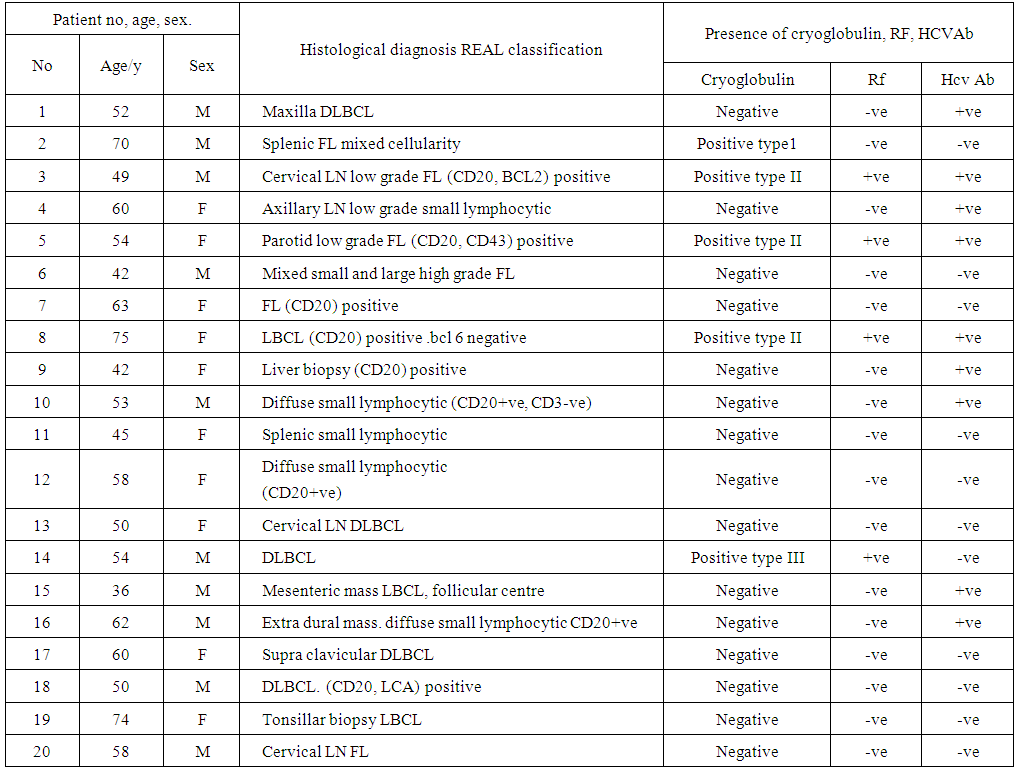 | Table 2. Correlation between lymphoma type, RF, HCVAb and cryoglobulinemia |
4. Discussion
- In the present work we aimed to study the presence of cryoglobulinemia in 20 patients suffering from NHL.We found the percentage of prevalence 25% positive cases (5 out of 20).60% of these positive cryoglobulinemic cases were HCV positive while 40% were HCV negative.The incidence of cryoglobulinemia in NHL patients with negative HCVAb in our study was 10% of total lymphoma cases. This result is in agreement with ferri, 2002 who stated that B-cell lymphoma is the most frequent neoplastic manifestation complicating MC, often as late manifestation of the MC syndrome. This complication may be related to peripheral B-lymphocyte expansion and to lymphoid nfiltrates observed in the liver and bone marrow of MC patients. In particular, these infiltrates have been regarded by some authors as "early lymphomas", since they are sustained by lymphoid components indistinguishable from those of B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma (B-CLL) and immunocytoma (Ic). However, unlike frank malignant lympomas they tend to remain unmodified for years or even decades and are followed by overt lymphoid tumors in about 10% of cases [6].In our study the association between (HCV) infection and mixed cryoglobulinemia was present in 60% of positive cases, this results is in agreement with Adinolfi 2003 who stated that by meta-analysis of 19 studies involving a total of 2323 patients showed the prevalence of cryoglobulinemia to average 44%. Low levels of circulating mixed CRs can be detected in 40-66% [7]. The association of hepatitis C (HCV) and cryoglobulinemia and the pathogenesis of HCV induced cryoglobulinemia have been intensively studied [8].As regard types of cryoglobulin in our study type I represent 20% of cryoglbulins, type II 60% and type III represent 20% and RF was negative in 20% and positive in 80% of positive cases.These results were approximately obtained by Kllemuchikkal and Gorevic 1999. They stated that the majority (95%) of CRs are immune complexes that contain rheumatoid factor (RF). Such CRs are known as mixed” cryoglobulins (type II and type III) to differentiate them from the CRs with monoclonal bands that do not contain RF or antigen-antibody complexes (type I). The antigens present in the mixed complexes may include RNA and proteins (eg, hepatitis C virus proteins). A small fraction of CRs (5%) comprise pure monoclonal gammopathies, which have poor solubility at low temperatures because of their unique amino acid sequences. There are also other cryoproteins that precipitate in the cold, such as cryofibrinogen (in plasma) and fibronectin [5].The positive cryoglobulinemic cases in our study are NHL of B cell.The study population was contain 20 patients 7 cases of follicular lineage which may be due to strong association between HCV infection and development of lymphoma as a late complication. It was explained by different authors. It is postulated that HCV infects circulating B lymphocytes, stimulating them initially to synthesize polyclonal IgM RF. However unknown factors induce a shift to abnormal proliferation of a single clone of B cells that produces monoclonal IgM-κ RF, leading to typeII mixed cryoglobulinemia [9]. CRs similar to those in the serum can be detected in white cells of the patients. HCV-RNA is found concentrated and bound to the CR precipitate. Patients with HCV and cryoglobulinemia [10]. Type II have been found to have a Bcl-2 rearrangement in peripheral blood leucocytes [10]. ANA was positive in 5% of cases while in +ve cryoglobulinemic pt was 20%. It was done to exclude auto immune causes of cryoglobulininemia. Anemia, leucopenia, thrombocytopenia were present by different percentage due to chemotherapy and BM infiltration.ESR is markedly elevated in 40% of positive cryoglobulininemic patients due to presence of abnormal serum proteins. ALT, AST. Serum albumin were affected may be due to liver affection by HCV or lymphoma.Lymphoma, 7 cases of diffuse larg Bcell lymphoma and 6 cases of diffuse small lymphocytic lymphoma. We found prevalence of cryoglobulinemia 25% (5 out of 20) of NHL cases. 60% of these positive cryoglobulinemic cases were HCV positive while 40% were HCV negative.In our study the incidence of cryoglobulinemia in NHL patients with negative HCVAb was 10%. As regard types of cryoglobulin typ I represent 20% of positive cases, type II were 60% while type III were 20% and RF was negative in 20% and positive in the other 80%.In our work all the NHL cases giving positive cryoglobulin were of B cell type.
Therapeutic Considerations
- For a correct therapeutic approach, three important factors namely, the HCV infection, the presence of autoimmune disorder, and the possible neoplastic complications should be considered.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML