-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2014; 4(5): 79-82
doi:10.5923/j.cmd.20140405.01
A Study to Evaluate Relationship of Tracheal Diverticulum with Emphysematous Changes in Lung Using Multi-Detector Computed Tomography - A Report from North-West India
Rajesh Sharma1, Manjit Arora1, Manik Mahajan2, Puneet Gupta1, Poonam Sharma3
1Department of Radio-diagnosis and Imaging, ASCOMS Hospital, Jammu University, Jammu, India
2Department of Radio-diagnosis and Imaging, PGIMS, Pt. B.D. Sharma University of Health Sciences, Rohtak, India
3Department of Pathology, GMC Hospital, Jammu University, Jammu, India
Correspondence to: Puneet Gupta, Department of Radio-diagnosis and Imaging, ASCOMS Hospital, Jammu University, Jammu, India.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
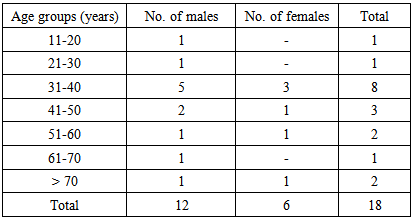
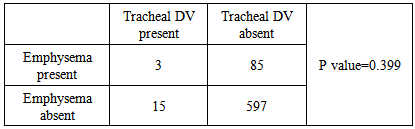
Tracheal diverticulum (DV) is an incidental finding in patients undergoing computed tomography (CT) examinations of chest & may have some association with chronic cough and emphysematous changes. A few studies have investigated the relationship between tracheal DV and emphysematous changes but still there is no consensus on the relationship. In our study, scans of 700 consecutive patients who underwent thoracic Multi-Detector Computed Tomography (MDCT) examination during a period of 2 years at a tertiary care centre in north-west India were reviewed. Tracheal diverticula were evaluated for localization, and communication with the tracheal lumen and their relation to pulmonary emphysema was analysed. Out of 700 patients, 435 were males & 265 were females. Tracheal diverticula were seen in 18 patients. Out of these 18 patients, 12 (66.6%) were males and 6 (33.3%) females. The highest proportion of tracheal diverticula (8/18, 44.4%) were seen in the fourth decade of life. In 16 out of 18 (88.9%) patients, the diverticula were located along the posterolateral aspect of the trachea on right side. 3 out of 18 (16.6%) patients with tracheal DV had underlying morphological emphysema. The relationship between the presence of Tracheal DV and emphysema was not statistically significant. We concluded that tracheal DV is often an asymptomatic finding in MDCT scans of chest and is more common in men than in women. The proportion of patients with tracheal DV was 2.57% in our study. No significant correlation could be established between tracheal DV and emphysematous changes.
Keywords: Emphysema, Multi-Detector Computed Tomography, Trachea, Diverticulum
Cite this paper: Rajesh Sharma, Manjit Arora, Manik Mahajan, Puneet Gupta, Poonam Sharma, A Study to Evaluate Relationship of Tracheal Diverticulum with Emphysematous Changes in Lung Using Multi-Detector Computed Tomography - A Report from North-West India, Clinical Medicine and Diagnostics, Vol. 4 No. 5, 2014, pp. 79-82. doi: 10.5923/j.cmd.20140405.01.
1. Introduction
- Paratracheal air cysts (PTACs) comprise of various pathological entities including tracheocele, tracheal diverticula and tracheogenic cysts [1, 2]. Tracheal DV is a paratracheal air cyst which is a collection of air that pouches out of the tracheal wall. Histopathologically, it is a lymphoepithelial or bronchogenic cyst. All these cysts consist of ciliated columnar epithelia and these may be connected to the trachea with a thin neck [3, 4]. Although most patients remain asymptomatic, some may have a history of repeated respiratory infections.MDCT is important for the diagnosis of tracheal DV and co-existing parenchymal pathologies. Goo et al [3] demonstrated that tracheal DV and bronchial DV may be accompanied by chronic obstructive pulmonary disease (COPD). A study by Buterbaugh and Erly [5] found no association between the presence of emphysematous lung changes and PTACs. Recent studies by Kurt A et al [6] and Sade R et al [7] showed that there is no significant association between tracheal DV and COPD. However the relationship between tracheal DV and pulmonary emphysema is still a matter of debate and needs to be further elaborated. The aim of this study was to determine the prevalence of tracheal DV in north-west India and its correlation with emphysematous changes in lung.
2. Materials and Methods
- This retrospective study was carried out at a tertiary care centre in north-west India. A total of seven hundred patients who underwent MDCT examination for any chest pathology from October 2012 to March 2014 were included in the study. Patients with mediastinal injury were not included in the study. The scans were performed using GE Health Care (Bright Speed Elite 16) CT system which is modified third generation machine. The CT examination of patients was performed in full inspiration in the supine position using 1.25 mm slice thickness. The window width was 1500 Hounsfield Units (HU) for the lung window and 400 HU for the mediastinal window. The window level was -700 HU for the lung window and 10 HU for the mediastinal window. Intravenous contrast agents were used for all the scans except for patients with acute or chronic renal insufficiency.Two radiologists independent of each other retrospectively reviewed all the CT scans. The decision about the CT findings was reached by consensus. All the CT images were reviewed on PACS using the continuous axial and coronal reformatted images for detecting tracheal DV. Tracheal diverticula were evaluated for location, and presence of visible communication with the trachea. Associated emphysematous changes in the lung parenchyma were also evaluated in all the patients. Patient demographics of age and sex were also collected.
3. Results
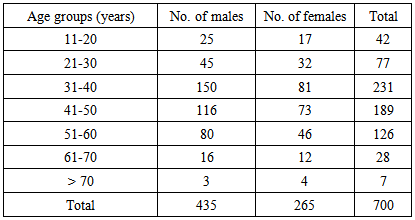
- A total of 700 patients formed the material of the study. The age of patients varied from 18 years to 80 years. The majority of the patients (231/700, 33%) belonged to 4th decade (Table 1). Out of 700 patients, 435 (62.1%) were males and 265 (37.86 %) were females with a male to female ratio of 1.64 (Table 1).
|
|
|
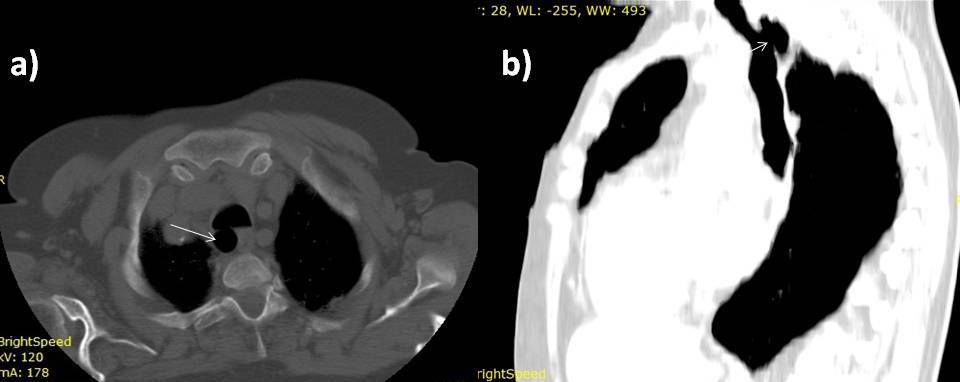
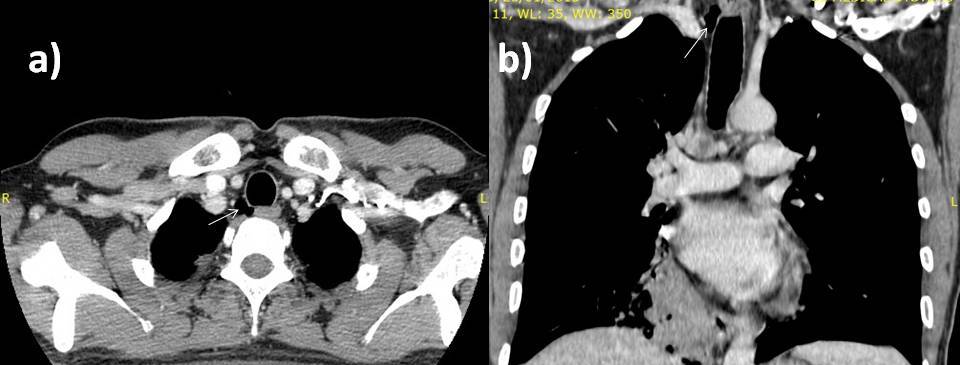 | Figure 1. a) Axial and b) Sagittal MDCT images of chest in mediastinal window showing the presence of tracheal diverticulum (white arrow) on right posterolateral aspect of trachea |
 | Figure 2. Axial MDCT images of chest in mediastinal window showing the presence of tracheal diverticulum (white arrow) on left posterolateral aspect of trachea |
 | Figure 3. a) Axial and b) Sagittal MDCT images of chest in mediastinal window showing the communication of tracheal diverticulum with trachea (white arrow) |
4. Discussion
- The differential diagnoses of PTACs include a laryngocele, a pharyngocele, a Zenker's diverticulum, tracheal diverticulum, an apical hernia of the lungs and apical paraseptal bullae [3]. Although the cause and pathophysiology of the PTACs are still unknown, they are mostly considered as tracheal DV. In previous studies, the incidence of PTACs was 2% according to Goo et al [3] and 3.7% according to Buterbaugh and Erly [5]. The incidence of tracheal DV in our study was 2.71% which is in accordance with literature reports. There is an increase in the detection rates of tracheal DV rather than its true increase because of the advanced CT technology used which results in thinner sections and a higher spatial resolution. Tracheal diverticula are rare and usually found post-mortem [8]. Tracheal diverticula are mostly located at the right posterolateral aspect of the trachea at the level of the T2 vertebrae, which is the transitional zone of the intrathoracic and extrathoracic trachea [9]. Two types have been reported; congenital and acquired [10]. Congenital tracheal DV are relatively smaller and located approximately 4–5 cm below vocal cords [11]. Acquired causes are common than the congenital one and its wall consists only of respiratory epithelium, without any cartilaginous or smooth muscular elements. Acquired tracheal diverticula are a result of increased intraluminal pressure that results in mucous membrane herniation through a weak point in the tracheal wall [11].Tracheal DV is commonly asymptomatic and incidentally detected. If it becomes a large cavitary lesion filled with secretions, it can lead to chronic cough, recurrent respiratory tract infections, dyspnea, hemoptysis or stridor. In addition, tracheal DV can apply pressure to the vocal cords, and thus, dysphonia can occur [12]. Sometimes tracheal DV can be a cause of unsuccessful intubation. Pneumomediastianum as one of the complication has been reported in such cases [13-15]. According to the study of Cheng et al. [16] and Buterbough et al. [5], PTACs are more common in females than males. They demonstrated a significant association between paratracheal air cysts and sex; however, in our study, we found that tracheal diverticula are more common in males.Axial, coronal and sagittal MDCT images are very useful for demonstrating the communication between the tracheal lumen and DV. Bronchoscopy can also be used in the diagnosis of the tracheal DV, but narrow-necked DV and fibrous connections can be easily misdiagnosed [17]. Buterbough et al. [5] observed 35% patients with DV had direct communication with trachea , on the other hand Goo et al. [3] observed only 8% patients had communication between trachea and DV. So there is a wide range of incidence between the two studies.A relationship between tracheal DV and COPD is noted in previous studies. Goo et al. [3] reported that right PTACs could be a sign of obstructive lung disease clinically and presence of emphysema radiologically. Buterbough et al. [5] on the other hand concluded that there was no significant relation between PTACs and obstructive lung disease in their study. Similarly Kurt A et al [6] and Sade R et al [7] in their studies found no significant association between tracheal DV and emphysematous changes. In our study also, no significant correlation could be established between tracheal DV and emphysematous changes in the lung.Our study has a few limitations. First, it is a retrospective study. Second, none of our patients had bronchoscopy to clearly demonstrate the communication between the DV and the tracheal lumen, although it should also be kept in mind that bronchoscopy may not always clearly reveal the communication between the DV and the tracheal lumen. Third, there was no confirmation of the tracheal diverticula histopathologically.In conclusion, tracheal DV is often an asymptomatic finding in MDCT scans of the chest. The proportion of tracheal DV in our study was 2.57%. Tracheal DV was more common in men than in women in our study. Our study also demonstrated that there is no significant association between tracheal DV and COPD and further research is required in future to substantiate the findings.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML