-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2014; 4(2): 29-31
doi:10.5923/j.cmd.20140402.03
Plummer-Vinson Syndrome with Hyperplastic Gastric Polyp
Kelly Schrapp MD, Marvin Crawford MD, Punita Kaveti MD, Avantika Chenna MD
Department of Internal Medicine, Morehouse School of Medicine, Atlanta, GA 30310-1495
Correspondence to: Kelly Schrapp MD, Department of Internal Medicine, Morehouse School of Medicine, Atlanta, GA 30310-1495.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Plummer-Vinson syndrome (PVS) is a rare disorder characterized by iron deficiency anemia, post cricoid dysphagia and esophageal webs. It is usually seen in 40-70 years of age. This disorder has been associated with autoimmune disorders like Celiac disease, Sjogren’s disease and also malignancies. In our literature review, iron deficiency anemia (IDA) has been hypothesized as the cause for esophageal web formation; however the cause of IDA was not discussed in these cases. This is a case of 75 year old female who presented with severe fatigue secondary to grade III dysphagia and found to have IDA. Esophagogastroduodenoscopy showed an esophageal stricture and a large hyperplastic gastric polyp. We postulate that hyperplastic gastric polyp was the probable cause of IDA which led to esophageal stricture formation and dysphagia.
Keywords: Plummer-Vinson syndrome, Paterson-Brown-Kelly syndrome, Hyperplastic gastric polyp
Cite this paper: Kelly Schrapp MD, Marvin Crawford MD, Punita Kaveti MD, Avantika Chenna MD, Plummer-Vinson Syndrome with Hyperplastic Gastric Polyp, Clinical Medicine and Diagnostics, Vol. 4 No. 2, 2014, pp. 29-31. doi: 10.5923/j.cmd.20140402.03.
1. Introduction
- Plummer Vinson Syndrome (PVS) is characterized by esophageal webs, iron deficiency anemia (IDA), and post cricoid dysphagia [1, 2, 3, 4]. It is a rare disorder that occurs in middle aged woman from the 4th decade of life until the 7th decade [5]. Plummer Vinson Syndrome was common in the first half of the 20th Century in middle aged Caucasian women. Now, it is very rare due to improved nutritional state of the population. Elderly population is still at risk for malnutrition and iron deficiency anemia [6]. We present a case of PVS in which the dysphagia did not respond to iron repletion which required endoscopic dilatation.
2. Case Report
- A 75 years old female with no significant past medical history including cardiac history, surgical history or family history who presented with weakness, fatigue and shortness of breath with exertion of 5 months duration. Patient denied any cough, chest pain, light-headedness, palpitation, orthopnea or PND. She reported difficulty swallowing solid food for 3 months. She had no difficulty swallowing liquids and she would either blend her food or eat soft food. She denied any nausea, vomiting, or any history of gastro esophageal reflux disease, diarrhea, constipation or melena. She admits to an increased craving for dirt and ice. She did not have any significant past medical, surgical or family history. She was allergic to aspirin and with no history of tobacco, alcohol or illicit drug use.On examination, she was afebrile, tachycardic with HR- 112, BP- 163/ 85 mm Hg, SaO2- 100% on room air. Physical examination findings were significant for pallor, loss of eye brows, glossitis (picture 2) with smooth red tongue and angular cheilitis (picture 1) with significant limitation in opening her mouth due to scarring at the corners of her mouth.
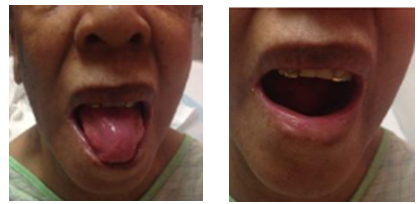 | Picture 1. Glossitis, Angular cheilitis (left side) and Limitiation in opening mouth (right side) |
 | Picture 2. Loss of eyebrows, glossitis |
 | Figure 1. Barium Swallow showing a benign short segment moderate grade stricture in the lower cervical esophagus with smooth borders. |
 | Figure 2. Esophagogastroduodenoscopy image with dilatation under fluoroscopy and proximal esophageal stricture was dilated to 12.8 mm with savory dilation |
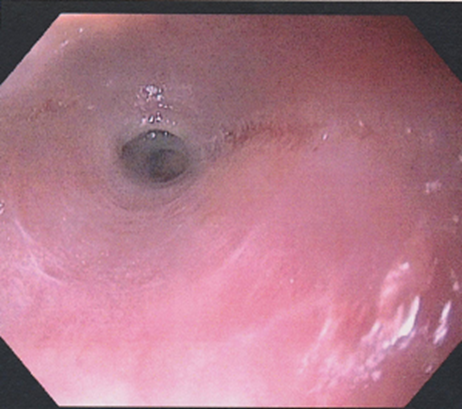
 | Figure 3. Esophagogastroduodenoscopy image of the large pedunculated polyp in antrum and sessile nodular polyp in the body of stomach |
3. Discussion
- Plummer Vinson Syndrome is a triad of symptoms including iron deficiency anemia, post cricoid dysphagia and esophageal webs. While we do not have good data on incidence and prevalence of this disease, we do know that it is more common in developing countries due to poor nutritional status. Although the pathogenesis of web formation is not known, most probable cause has been hypothesized as iron deficiency which causes reduction in iron dependent enzymes in rapid turnover cells leading to mucosal degenerations, atrophic changes and web formation and may even lead to cancer development of the upper gastrointestinal tract [7]. Some suggest that PVS is an autoimmune phenomenon and has been associated with autoimmune conditions, such as rheumatoid arthritis, pernicious anemia, celiac disease, and thyroiditis [8, 9, 10, 11]. In one study, a significantly high proportion of patients with PVS had thyroid cytoplasmic autoimmune antibodies compared to controls with iron deficiency. The autoimmune theory, however, has gained little acceptance to date. It has also been suggested that a complicated inlet patch (heterotopic gastric mucosa) has also been implicated in the pathogenesis of PVS [3-6].Esophageal stricture is usually painless and not associated with inflammation, swelling or ulceration, which causes obstructive dysphagia. Its anatomical forms range from thin web to long sleeve stricture [12]. While literature review elucidates the resolution of the dysphagia with iron therapy, as the web progress to stricture formation, iron therapy may not be useful and endoscopic dilation of stricture may be required for symptomatic relief [13].Hyperplastic gastric polyps are usually asymptomatic polyps incidentally found in 6% of upper GI endoscopies [14]. They may also present as abdominal pain, iron deficiency anemia secondary to occult GI bleeding, gastric outlet obstruction and rarely as overt GI bleeding [15,16]. They are associated with conditions such as Helicobacter pylori gastritis and atrophic autoimmune gastritis, which predispose the epithelium to chronic inflammation and epithelial repair. These polyps are typically identified in patients older than 60 years of age and rare in young individuals. Hyperplastic gastric polyps are usually benign lesions although malignant transformations have been reported in about 1.5 to 2.1% cases [17]. Endoscopic polypectomy should be considered in gastric hyperplastic polyps > 1 cm to avoid missing neoplastic lesions.Plummer Vinson Syndrome has been thought to be precancerous causing squamous cell cancer in the hypopharynx, esophagus, and oral cavity [18]. The reviewed literature recommends close follow up of patient with PVS for cancer surveillance but does not provide any guideline about how frequently the patient should be followed up or have screening upper GI endoscopy. PVS has been known to us for decades and its incidence is reducing due to improved nutritional status. There are many important questions that need to be answered regarding PVS pathogenesis, disease progression, treatment and cancer surveillance.IDA in PVS has been associated to nutritional deficiency, blood loss due to menstrual bleeding or autoimmune disorders. From the literature review, PVS has not been associated with gastric polyps. We hypothesize that the cause of the IDA and dysphagia in our patient was due to obscure GI bleeding from gastric polyp. As this can be precancerous, it is extremely important to have continued close follow up to monitor for recurrent esophageal webs and cancer.
4. Conclusions
- Iron deficiency anemia in Plummer Vinson syndrome could be due to occult gastrointestinal bleeding from hyperplastic gastric polyp. Due to improved nutritional status of population, PVS incidence may be reduced but elderly population are still at risk for iron deficiency anemia and PVS.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML