-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2013; 3(4): 88-91
doi:10.5923/j.cmd.20130304.03
Utilisation of Hospital Emergency Departments among Immigrants from Refugee Source-Countries in Queensland
Ibrahim Mahmoud, Xiang-Yu Hou
School of Public Health & Social Work, Queensland University of Technology (QUT), Brisbane, 4059, Australia
Correspondence to: Ibrahim Mahmoud, School of Public Health & Social Work, Queensland University of Technology (QUT), Brisbane, 4059, Australia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
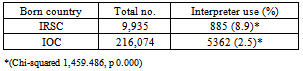
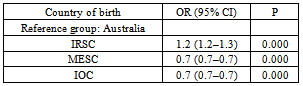
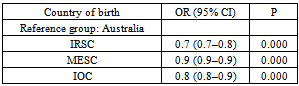
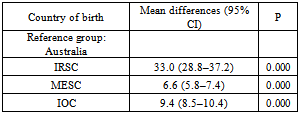
Despite the increasing number of immigrants, there is a limited body of literature describing the use of hospital emergency department (ED) care by immigrants in Australia. This study aims to describe how immigrants from refugee source countries (IRSC) utilise ED care, compared to immigrants from the main English speaking countries (MESC), immigrants from other countries (IOC) and the local population in Queensland. A retrospective analysis of a Queensland state-wide hospital ED dataset (ED Information System) from 1-1-2008 to 31-12-2010 was conducted.Our study showed that immigrants are not a homogenous group. We found that immigrants from IRSC are more likely to use interpreters (8.9%) in the ED compared to IOC. Furthermore, IRSC have a higher rate of ambulance use (odds ratio 1.2, 95% confidence interval (CI) 1.2–1.3), are less likely to be admitted to the hospital from the ED (odds ratio 0.7 (95% CI 0.7–0.8), and have a longer length of stay (LOS; mean differences 33.0, 95% CI 28.8–37.2), in minutes, in the ED compared to the Australian born population. Our findings highlight the need to develop policies and educational interventions to ensure the equitable use of health services among vulnerable immigrant populations.
Keywords: Emergency Department, Immigrants, Refugees, Utilisation
Cite this paper: Ibrahim Mahmoud, Xiang-Yu Hou, Utilisation of Hospital Emergency Departments among Immigrants from Refugee Source-Countries in Queensland, Clinical Medicine and Diagnostics, Vol. 3 No. 4, 2013, pp. 88-91. doi: 10.5923/j.cmd.20130304.03.
Article Outline
1. Introduction
- A number of international studies have shown differences in the use of emergency department (ED) care between immigrants and local populations[1-5]. Currently, a limited body of literature exists describing the use of ED care by immigrants in Australia. This is despite the 2011 Census showing that over 6 million (27%) of Australia’s people were born overseas[6]. However, immigrants are not a homogeneous group. Annually, Australia resettles about 13,000 refugees via the Humanitarian Program[7]. People from refugee backgrounds may have experienced the ill effects of the conditions in refugee camps, thus arriving with existing health problems[8-10]. For those people, access to appropriate health care facilities after their arrival in a new country is often limited by cultural, language, or financial barriers[11,12]. Poor and inappropriate access to the health care services for this vulnerable group might have serious implications for their health[13,14]. Several studies have shown that some immigrants from refugee backgrounds tend to use ED care as a primary source of health care[2,5]. This might be influenced by their previous patterns of use in their origin countries[15,16]. Therefore, these immigrants may be disadvantaged by a lack of access to preventive and primary health care facilities and thus place an additional burden on ED care due to inappropriate access. Immigrant access to healthcare services, such as ED services, and outcomes of such interaction have been widely studied in a number of countries; however, the topics have received little attention in Australia. Therefore, this study aims to describe how immigrants from refugee source countries (IRSC) utilise ED care in terms of their requirement of interpreters, ambulance use, admission to hospital, and length of stay (LOS) in the ED, compared to immigrants from the main English speaking countries (MESC), immigrants from other countries (IOC) and the local population in Queensland. The study may provide original data to fill some of the gaps in this area.
2. Methods
2.1. Study Design and Setting
- An analysis of the Queensland public hospitals’ ED dataset for the three calendar years, from 1 January 2008 to 31 December 2010, was undertaken. Queensland, located in northeast Australia, is the second-largest in land mass and third-most populous state of Australia.
2.2. Data Source
- The data were sourced from the Emergency Department Information System (EDIS). The EDIS is an electronic information system for public hospital EDs in Queensland. It provides data such as modes of arrival (ambulance, walk-in including via public transport and others), triage category, gender, age, country of birth, and ED departure status (admission to hospital, did not wait, died, or discharge). Ethical approval to use unidentified data was obtained from the Queensland Health Central Ethics Unit(HREC/11/QHC/29).
2.3. Data Analysis
- The proportions of interpreter use were calculated using Pearson’s chi-square test. Logistic and multiple linear regression analyses were performed to determine the relationships between ambulance use and country of birth, admission status and country of birth, and LOS in the ED and country of birth. The analyses were adjusted for gender, age, interpreter use, and triage categories (resuscitation, emergency, urgent, semi-urgent, and non-urgent), according to the Australasian Triage Scale (ATS)[17]. The results were calculated using Statistical Package for the Social Sciences (SPSS) version 19 (IBM SPSS Statistics 19).
2.4. Immigrants’ Countries of Origin
- The term main English-speaking country (MESC) is used to describe people migrating from the United Kingdom, the Republic of Ireland, New Zealand, Canada, South Africa, and the United States of America, according to the Australian Bureau of Statistics (ABS)[18]. Information about immigration status and distribution of refugees is not available from the EDIS. Therefore, we used the same approach used by[19] in their study on the Victorian Admitted Episodes Dataset (VAED)[19]. They used country of birth as a proxy indicator of refugee status[19]. Refugee source countries are those countries where significant numbers of people have been forcibly displaced due to persecution, violence, and war[19]. A cut-off was made from 1980 onwards to differentiate recent refugees from former refugees, who entered Australia through the Refugee and Humanitarian Program. The new refugee source countries, as indentified by[19], are Afghanistan, Bosnia-Herzegovina, Burma, Eritrea, Ethiopia, Iraq, Somalia, and Sudan[19]. We excluded from the analysis those people who did not state their country of birth.
3. Results
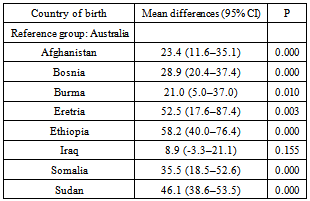
- Of the total of 2,953,731 visits to Queensland public hospital EDs between January 2008 and December 2010, 2,395,382 (81.1%) were born in Australia, 292,138 (9.9%) were born in MESC, 9,935 (0.3%) were born in refugee source countries, 216,074 (7.3 %) were born in other countries, and 40,202 (1.4%) did not state their country of birth. Overall, people from MESC and IOC had very similar rates of ED care use and LOS in ED, with little difference from people born in Australia.
|
|
|
|
4. Discussion
- Our study showed heterogeneity in the use of ED care among immigrants in Queensland. The study found that people born in refugee source countries have higher interpreter use, higher ambulance use, lower admission to hospital, and longer LOS in the ED than immigrants from other countries, using the Australian born population as a reference group. Understanding that immigrants are not one group, their patterns of ED care use are vital in terms of policy planning and the development of educational interventions to provide equitable health care to disadvantaged immigrants. People from refugee source countries might use ED care as their the principal provider of their health care instead of primary care due to several barriers[2,5]. General practitioners who do not speak the patients’ languages and the unavailability of interpreters in general practice settings might be two of the reasons why patients with limited English proficiency seek care in hospital Eds[20]. Furthermore, a lack of transport might encourage low socio-economic refugees to use ambulance service for transport to hospital EDs for non-critical conditions[14]. However, a study from the Liverpool Hospital ED in Sydney that found that recently resettled refugees were afraid of calling for an ambulance, despite their ability to do so and their conviction that such a call was needed[16]. However, their study was a single site study with a small sample size, which limits its applicability to the Australian refugee population. Unfortunately, Our study was not able to determine whether the high use of ambulances among IRSC is due to the vulnerability of this group to illness, and attending EDs with advanced illness requires an ambulance, or due to a lack of transport. To date, there has been a paucity of empirical studies on how immigrants in Australia use ambulances. Thus, this topic warrants further investigation. LOS is a marker of ED overcrowding and a key component of ED quality assurance monitoring[21,22]. Our study found a significant prolonged LOS in the ED among people from refugee source countries, particularly those from Sudan, Bosnia, Afghanistan, and Burma, compared to the Australian born population. These findings agree with other studies that showed an association between longer LOS in the ED and differences in language between health care providers and patients[23,24]. Although our regression model controlled for interpreter use and triage priority, it explained only 16.5% of the variability in LOS. This indicates that there are other significant factors influencing LOS in EDs, besides language and the severity of the condition, which were not captured by our study. Our study has some limitations. It originated from routinely collected state-wide data (EDIS) and provides only limited information on the characteristics of the patients. Therefore, the study dataset did not allow for the inclusion of all important factors of ED care use, such as socio-economic status, immigration status, and LOS in Australia. Another limitation is that the EDIS data were de-identified, which did not allow analyses of individual patients. As such, some patients might have made multiple visits to the ED. There are also limitations when conducting a large secondary data analysis, such as adequacy, accuracy, and completeness[25]. However, every humanly possible effort was made to ensure accuracy and consistency in the data retrieval process.
5. Conclusions
- Our findings regarding ED care use may reflect some barriers that IRSC face when accessing primary health care services. We recommend further research using mixed methodologies to investigate why IRSC use ED care differently from others. This could help in developing educational intervention programs for this population and making policies that favour their access to primary care as well as ED care.
ACKNOWLEDGMENTS
- The authors are grateful to the Hospital Access Analysis Team (HAAT) of Queensland Health, the data custodians of the EDIS data. The authors are also grateful to Dr Ignacio Correa-Velez for his invaluable comments on the manuscript.
References
| [1] | M. Norredam, A. Krasnik, T. M. Sorensen, N. Keiding, J. J. Michaelsen, and A. S. Nielsen, 2004, Emergency room utilization in Copenhagen: A comparison of immigrant groups and Danish-born residents, Scand J Public Health, 32(1), 53–59. |
| [2] | M. Norredam, A. Mygind, A. S. Nielsen, J. Bagger, and A. Krasnik, 2007, Motivation and relevance of emergency room visits among immigrants and patients of Danish origin, Eur J Public Health, 17(5), 497–502. |
| [3] | M. Rué, X. Cabré, J. Soler-González, A. Bosch, M. Almirall, and M. C. Serna, 2008, Emergency hospital services utilization in Lleida(Spain): A cross-sectional study of immigrant and Spanish-born populations, BMC Health Serv Res, 8(1), 81. |
| [4] | A. Buron, F. Cots, O. Garcia, O. Vall, and X. Castells, 2008, Hospital emergency department utilisation rates among the immigrant population in Barcelona, Spain. BMC Health Serv Res, 8(1), 51. |
| [5] | P. J. DeShaw, 2006, Use of the emergency department by Somali immigrants and refugees, Minn Med, 89(8), 42. |
| [6] | Australian Bureau of Statistics (ABS). 2012. Migration. Canberra, ABS. [Online]. Available:http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/3C7F1FB366F20C54CA257A5A00120F44/$File/34120_2010-11.pdf |
| [7] | Department of Immigration and Citizinship (DIAC). 2012. How many people does Australia resettle? [Online]. Available:http://www.immi.gov.au/media/publications/pdf/A_New_Life_2.pdf |
| [8] | A. Neale, J. Y. Y. Ngeow, S. A. Skull, and B. A. Biggs, 2007, Health services utilisation and barriers for settlers from the Horn of Africa, Aust N Z J Public Health, 31(4), 333–335. |
| [9] | Z. Steel, D. Silove, K. Bird, P. McGorry, and P. Mohan, 2005, Pathways from war trauma to posttraumatic stress symptoms among Tamil asylum seekers, refugees, and immigrants, J Traumatic Stress, 12(3), 421–435. |
| [10] | M. F. Harris and B. L. Telfer, 2001, The health needs of asylum seekers living in the community, Med J Aust, 175(11-12), 589–592. |
| [11] | N. Davidson, S. Skull, D. Burgner, P. Kelly, S. Raman, D. Silove et al., 2004, An issue of access: Delivering equitable health care for newly arrived refugee children in Australia, J Paediatr Child Health, 40(9-10), 569–575. |
| [12] | M. Zimmerman, R. Bornstein, and T. Martinsson, 1990, An estimation of dental treatment needs in two groups of refugees in Sweden, Acta Odontologica Scand, 48(3), 175–182. |
| [13] | K. P. Derose, J. J. Escarce, and N. Lurie, 2007, Immigrants and health care: Sources of vulnerability, Health Aff (Millwood), 26(5), 1258–1268. |
| [14] | M. Sheikh-Mohammed, C. R. MacIntyre, N. J. Wood, J. Leask, and D. Isaacs, 2006, Barriers to access to health care for newly resettled sub-Saharan refugees in Australia, Med J Aust, 185(11-12), 594–597. |
| [15] | P. Nugus, K. Carroll, D. G. Hewett, A. Short, R. Forero, and J. Braithwaite, 2010, Integrated care in the emergency department: A complex adaptive systems perspective, Soc Sci Med, 71(11), 1997–2004. |
| [16] | M. Sheikh, P. I. Nugus, Z. Gao, A. Holdgate, A. E. Short, A. Al Haboub et al., 2011, Equity and access: Understanding emergency health service use by newly arrived refugees, Med J Aust, 195(2), 74–76. |
| [17] | R. Forero and P. Nugus. 2012. Literature review on the Australasian Triage Scale (ATS), Sydney, The Australasian College for Emergency Medicine (ACEM). [Online]. Available: http://www.acem.org.au/home.aspx?docId=1 |
| [18] | Australian Bureau Statistics (ABS). 2013. Perspectives on migrants. Canberra, ABS. [Online]. Available:http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3416.0Glossary1Mar%202013 |
| [19] | I. Correa-Velez, V. Sundararajan, K. Brown, and S. M. Gifford, 2007, Hospital utilisation among people born in refugee-source countries: An analysis of hospital admissions, Victoria, 1998–2004, Med J Aust, 186(11), 577–580. |
| [20] | G. Bonacruz Kazzi and C. Cooper, 2003, Barriers to the use of interpreters in emergency room paediatric consultations, J Paediatr Child Health, 39(4), 259–263. |
| [21] | A. Herring, A. Wilper, D. U. Himmelstein, S. Woolhandler, J. A. Espinola, D. F. M. Brown et al., 2009, Increasing length of stay among adult visits to US emergency departments, 2001–2005, Acad Emerg Med, 16(7), 609–616. |
| [22] | P. Yoon, I. Steiner, and G. Reinhardt, 2003, Analysis of factors influencing length of stay in the emergency department, CJEM, 5(3), 155–161. |
| [23] | R. D. Goldman, P. Amin, and A. Macpherson, 2006, Language and length of stay in the pediatric emergency department, Pediatr Emerg Care, 22(9), 640–643. |
| [24] | S. Yeo, 2004, Language barriers and access to care, Annu Rev Nurs Res, 22(1), 59–73. |
| [25] | C. M. Sanders, S. L. Saltzstein, M. M. Schultzel, D. H. Nguyen, H. S. Stafford, and G. R. Sadler, 2012, Understanding the limits of large datasets, J Cancer Educ, 27, 1–6. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML