-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2012; 2(4): 33-36
doi: 10.5923/j.cmd.20120204.03
An Unusual Presentation of Coronary Artery Fistula in Athlete - Case Report
Alexander S. Kisko 1, Lubica Dernarova 1, Jan Kmec 1, Marika Vereb 2, Anna Hudakova 1, 1, Marta Jakubikova 1, Nelli Kishko 3
1Faculty of Health Care, Presov University in Presov, Presov, 080 01, Slovakia
2Nuclear Medicine, Sekcov Polyclinic, Presov, 080 01 Slovakia
3Medical Faculty, Uzhgorod National University, Uzhgorod, 080 01, Ukraine
Correspondence to: Alexander S. Kisko , Faculty of Health Care, Presov University in Presov, Presov, 080 01, Slovakia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
A 32-year-old active cyclist was referred for the evaluation because of syncope he had performed in preseason. He was found to be normostenic, acyanotic, normotensive with clear lungs and a regular pulse of 60 bpm, with normal dual heart sounds and a grade Levine 2/6 continuous diastolic murmur in the second intercostal space of the left parasternal area. He had no family history of premature cardiac death and his lipids were normal. Rest ECG showed a regular sinus rhythm of 62 bpm with incomplete right bundle branch block and no significant ST-T changes. A transthoracic ECHO in parasternal short-axis view revealed an anomalous colour flow jet in diastole arising from the lateral wall into the main pulmonary artery and coronary artery fistula with non-significant left-to-right shunt (Qp/Qs ratio 1.2).came under suspicion. In contrast, it has not been confirmed clearly by the transoesophageal ECHO. Coronary angiography was without coronary stenosis and confirmed a 'serpentine' anomalous drainage supposedly from left anterior descending artery to the main pulmonary artery. A complex anatomy of sacculary dilated fistula that originates from the proximal left anterior descending artery and drainages the main pulmonary artery was showed in detail by a 64 slice MDCT scanning. Myocardial Tc-99m Myoview perfusion SPECT imaging showed no perfusion defects in maximal physical stress and follow-up without intervention was suggested. In addition, due to the results of holter ECG monitoring, head-up tilt testing, carotid sinus massage and programmed atrial stimulation syncope was concluded as vasovagal, but its nature still remains discussible. After a three year follow-up patient remains asymptomatic and recently performed control myocardial perfusion SPECT showed no signs of stress related myocardial ischemia. In conclusion, several imaging techniques are needed for an accurate diagnosis of coronary fistula and for the suggestion of proper further management. In some cases syncope may be the first manifestation of CAF, but it is still unclear if it is directly related to the coronary anomaly.
Keywords: Coronary Artery Fistula, Syncope, Doppler Colour Flow Imaging, MDCT Scanning, Tc-99m Myoview Perfusion SPECT
1. Introduction
- Congenital coronary artery fistula (CAF), first described by Krause in 1865 is characterized by normal aortic origin of the coronary artery but with a fistulous communication with the great vessels as well as all cardiac chambers. CAFs are rare, predominantly congenital or occasionally acquired (such as stab or projectile injuries, post-coronary angioplasty) coronary artery anomalies that can originate from any of the three major coronary arteries. The evolution of the coronary artery network involves complex embryology. In early foetal development, persistence of myocardial sinusoids and the subsequent connection with the endothelial buds that Although coronary fistula is rare, it is one of the most common among the coronary artery anomalies. CAF most commonly affects the right side of the heart. It may occur isolated or along with congenital heart diseases[1]. According to the global experience the current characteristics of congenital coronary fistulas in adults had changed in the last decade. It was reported in 2006 that the origin of the fistulas was from the left coronary artery in 58% and from the right in 42% of patients and in the recently published review the overall figures were 69% and 31%, respectively. In 2006, the fistulas were unilateral, bilateral and multilateral in 93%, 6% and 1%, respectively. Currently, the majority, as expected, were unilateral fistulas (80%), followed by bilateral fistulas (18%) and finally multilateral fistulas (2%). Among the unilateral fistulas, the left anterior descending artery was predominantly the origin (42%) of the fistulas, followed by the right coronary artery (31%), the circumflex (20%) and finally the left main trunk (7%)[2]. CAFs most commonly drain into the right atrium or right ventricle, but occasionally can drain into the pulmonary artery. Bilateral coronary fistulas with the coronary artery stenosis are rare[3]. In these coronary artery abnormalities blood is shunted into a great vessel, or other structure, bypassing the myocardial capillary network and may produce steal phenomenon. Unless very large and hemodynamically significant, it is usually asymptomatic in younger patients. With increasing age, symptoms begin to appear, and the incidence of complication rises.The patients with CAFs are mostly asymptomatic, but some may present with symptoms of fatigue, dyspnoe, angina, arrhythmias, and signs of congestive heart failure, pulmonary hypertension or infective endocarditis. Syncope is very rarely associated with CAF. We report the case of coronary to main pulmonary artery fistula in active athlete first presented with syncope.
2. Case Presentation
- A 32-year-old active cyclist was referred for the evaluation because of syncope he had performed in preseason. He reported no history of the episodes of shortness of breath or chest pain associated with extreme physical exertion as well as palpitations or other clinical symptoms of cardiac arrhythmias. He was physically absolutely normal with no familial predisposition to sudden cardiac death or ischemic heart disease and normal lipids.At physical examination patient was found to be normostenic, acyanotic, normotensive, with clear lungs and a regular pulse of 60 bpm, with normal dual heart sounds. A grade Levine 2/6 continuous murmur could be heard mainly at the level of the second intercostal space of the left parasternal area. There were no signs of heart failure. An electrocardiogram at rest showed a regular sinus rhythm of 62 bpm with incomplete right bundle branch block and no significant ST-T changes.A transthoracic echocardiography in parasternal short-axis view revealed an anomalous colour flow jet arising from the lateral wall into the main pulmonary artery, identifying the fistula drainage site (fig.1) with non-significant left-to-right shunt (Qp/Qs ratio 1.2). In contrast, despite various projections, the exact anatomic course of the suspected fistula could not be clearly shown by the transoesophageal echocardiography. Coronary angiography confirmed 'serpentine' fistula with aneurysms corresponding the proximal portion of the left anterior descending artery and the main pulmonary artery with no significant signs of coronary atherosclerosis (fig.2).The complex anatomy of the fistula was demonstrated in detail by 64 Slice MDCT scanning using multiplanar and 3D reconstruction techniques. It showed a sacculary dilated fistula that originates from the proximal left anterior descending artery and drainages the main pulmonary artery (fig.3).
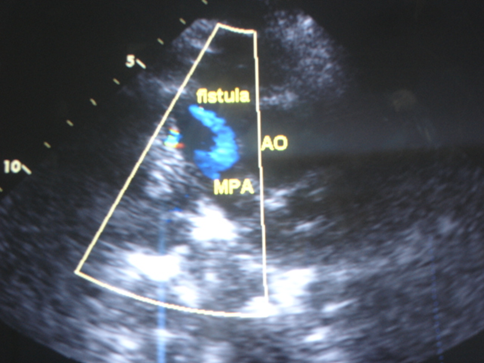 | Figure 1. A transthoracic echocardiography in parasternal short-axis view reveals an anomalous colour flow jet at colour Doppler analysis arising from the lateral wall into the main pulmonary artery |
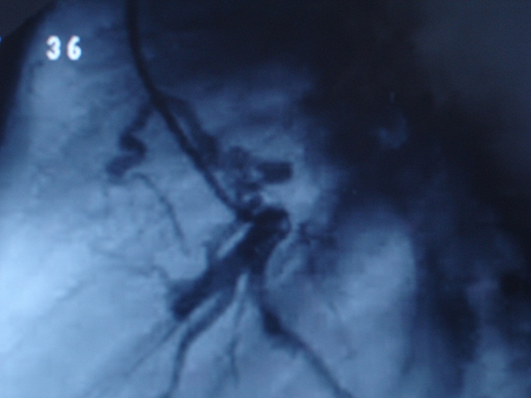 | Figure 2. Coronary angiography showing a ‘serpentine’ fistula with aneurysm corresponding the proximal portion of the left anterior descending artery and the main pulmonary artery |
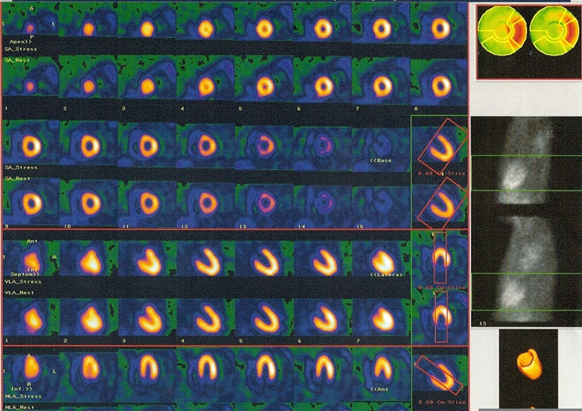 | Figure 4. Stress/Rest Tc-99m Myoview perfusion SPECT shows no stress-related perfusion defects |
3. Discussion
- The incidence of CAF ranges from 0.2-0.4% in selected series of congenital heart disease patients, and its incidence in the overall population is estimated to be about 0.002%. The incidence of CAF during 14,708 diagnostic cardiac catheterizations was 0.13. There was 1 traumatic and 19 congenital cases. All fistulas were small and of little hemodynamic significance. No symptoms or complications could be ascribed to these fistulas. In the large majority no continuous or other murmurs suggested their presence. Surgical treatment for these fistulas was not indicated. The majority of these fistulas arise from the right coronary artery. Left CAF is less common, but usually drains into the right ventricle or right atrium. A combination like the one described in the presented case is unusual since fistulas from the left coronary artery with drainage into the pulmonary artery occurs in only 17%[4].The majority of the patients with CAFs are clinically asymptomatic but the long-term outcome is not fully known. The clinical course of CAF may vary greatly from spontaneous closure to severe complications. The patients with coronary fistulas may present with dyspnoea, congestive heart failure, angina, endocarditis, arrhythmias, or myocardial infarction. Syncope is not a typical symptom related to fistulas and is very rare first clinical manifestation of CAF. It may be associated with some underlying congenital heart defects. Our patient presented with an isolated CAF but no other coexisting heart abnormalities and it was not fully understood whether a syncope episode was directly related to the fistula. Clinically manifested myocardial ischemia is resulting from fistula steal phenomenon. Coexisting congenital or acquired heart disease is found in 40% of patients; however, no associated lesion was found to have a specific relationship with CAF.Up to now there is no generally accepted recommendation about standard diagnostic protocol in case of suspected CAF. Clinical examination, transthoracic echocardiography, stress electrocardiogram and stress/rest myocardial perfusion imaging may be first line examinations in evaluation of coronary fistulas[5]. Clinical diagnosis of CAF is difficult due to symptomless or lack of specific symptoms. Clinical manifestations vary considerably and as it was mentioned above the patients with coronary fistulas may present with dyspnea, congestive heart failure, angina, endocarditis, arrhythmias, angina or myocardial infarction, but a majority of patients are asymptomatic as fistulas cause myocardial ischemia only in a small number of them. A continuous murmur heard at the upper sternum border is often presented and is highly suggestive of a coronary fistula Differential diagnosis includes persistent ductus arteriosus, pulmonary arteriovenous fistula, ruptured sinus of Valsalva aneurysm, aortopulmonary window, prolapse of the right aortic cusp with a supracristal ventricular septal defect, internal mammary artery to pulmonary artery fistula, and systemic arteriovenous fistula[6].Transthoracic echocardiography with colour flow imaging by an experienced echocardiographer is an ideal routine first-line and in some cases definitive diagnostic tool in the evaluation and diagnosis of CAF. The diagnosis of coronary fistula to the main pulmonary artery can usually be made by Doppler colour flow imaging when abnormal flow signals with mosaic appearance in the pulmonary artery is visualize. It is diagnostically useful to visualize shunt flows originating from the exit of a CAF. However, sometimes fistulas to the pulmonary artery may be difficult to detect. Nowadays, a contrast echocardiography and live three-dimensional transthoracic echocardiography can be useful in demonstration of coronary fistula[4],[7]. Transoesophageal echocardiography is capable of precisely demonstrating the origin, the course and the drainage site of the fistula, but sometimes like in presented case it may fail.Although noninvasive imaging may facilitate the diagnosis and identification of the origin and insertion of CAF, coronary angiography and MDCT are necessary for the precise delineation of coronary anatomy, for assessment of hemodynamics, and to show the presence of concomitant atherosclerosis and other structural anomalies.Ergometry or stress/rest myocardial perfusion imaging are required to determine the possible ischemic changes in the heart. In most cases bicycle/treadmill ergometry and stress/rest Tc-99m Myoview SPECT may be useful for coronary flow assessment and fistula-related steal phenomenon. No evidence of the stress induced myocardial ischemia was found in presented case. Risk stratification in CAF mostly depends on the significance of left-to-right shunt (QP/Qs ratio >1.5) and presence of the stress related reversible myocardial ischemia. In patients with non-significant CAF, conservative follow-up is strongly suggested and intervention procedures may be unnecessary. Elective closure of coronary artery fistulas by percutaneous transcatheter techniques or surgery is generally accepted in the presence of symptoms, but controversies exist in the management of asymptomatic patients[8]. Based on the experience, there is no evidence that clinically silent CAF diagnosed incidentally by colour Doppler echocardiography are associated with adverse clinical outcome. Conservative management with continued follow-up of these patients appears to be appropriate. Potentially serious and hemodynamically significant CAF require accurate recognition, and at times, percutaneous or surgical correction.
4. Conclusions
- Several imaging techniques are needed for an accurate diagnosis of coronary fistula and for the suggestion of proper further management. The patient presented in this case experienced a syncope at the time of diagnosis which was concluded as being of vasovagal etiology but its nature remains discussible. Consequently no intervention was recommended. The patient is seen in follow-up and is doing fine, participating in sports reporting no complaints, but he might require transcatheter closure or surgical treatment of fistula in case when he becomes symptomatic.
ACKNOWLEDGEMENTS
- Authors wish to acknowledge Claudia Gibarti, MD for performing MDCT scanning, Juraj Cencarik, MD and Jozef Stasko, MD for providing coronary angiography. Written consent was obtained from the patient for publication of this case report.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML