-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Medicine and Diagnostics
p-ISSN: 2163-1433 e-ISSN: 2163-1441
2011; 1(1): 17-20
doi: 10.5923/j.cmd.20110101.03
Pituitary Adenoma Complicated by Multifocal Fibrosclerosis Involving Sella and Retroperitoneum
James R. Hackney 1, Kristen O. Riley 2, Michael S. Vaphiades 2, 3, 4, Asim K. Bag 5, Cheryl Ann Palmer 1, 4
1Division of Neuropathology, Department of Pathology, University of Alabama at Birmingham, Birmingham, AL, 35294, USA
2Division of Neurosurgery, Department of Surgery, University of Alabama at Birmingham, Birmingham, AL, 35294, USA
3Department of Ophthalmology, University of Alabama at Birmingham, Birmingham, AL, 35294, USA
4Department of Neurology, University of Alabama at Birmingham, Birmingham, AL, 35294, USA
5Department of Radiology, University of Alabama at Birmingham, Birmingham, AL, 35294, USA
Correspondence to: Cheryl Ann Palmer , Division of Neuropathology, Department of Pathology, University of Alabama at Birmingham, Birmingham, AL, 35294, USA.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Multifocal fibrosclerosis (MFS) is a rare syndrome characterized by the co-occurrence of two or more fibrosing diseases thought to be of similar pathogenesis.Rarely, central nervous system manifestations of pachymeningitis or sellar/suprasellar fibrosis have been described.We report a patient with a pituitary adenoma with extensive fibrosclerotic stroma and idiopathic retroperitoneal fibrosis who initially presented with retroperitoneal fibrosis and obstructive renal failure. One day after transsphenoidal removal of the adenoma, he developed worsening vision, confirmed as hemorrhage into the residual tumor by imaging studies, and required craniotomy.The association of MFS with pituitary adenoma has not been previously reported.Such patients may be at greater risk for hemorrhagic complications due to the consistency of the tumor and its adherence to nearby normal anatomy.
Keywords: Pituitary Adenoma, Multifocal Fibrosclerosis, Retroperitoneal Fibrosis
Cite this paper: James R. Hackney , Kristen O. Riley , Michael S. Vaphiades , Asim K. Bag , Cheryl Ann Palmer , "Pituitary Adenoma Complicated by Multifocal Fibrosclerosis Involving Sella and Retroperitoneum", Clinical Medicine and Diagnostics, Vol. 1 No. 1, 2011, pp. 17-20. doi: 10.5923/j.cmd.20110101.03.
1. Introduction
- Multifocal fibrosclerosis (MFS) is a rare syndrome characterized by the co-occurrence of two or more fibrosing diseases thought to be of similar pathogenesis, including retroperitoneal fibrosis, sclerosing mediastinitis, Riedel’s thyroiditis, orbital pseudotumor, sclerosing cholangitis, sclerosing pachymeningitis and others[1,2]. We describe a patient with MFS involving the sella and retroperitoneum who developed a pituitary adenoma complicated bypostoperative hemorrhage.
2. Patient History
- A 45-year-old African-American man presented with nausea, vomiting, and weight loss in May of 2010. Computed tomography scan demonstrated a large retroperitoneal mass measuring 8.4 x 6 x 4cm that encased the ureters, surrounded the aorta, and surrounded the inferior vena cava. There was bilateral hydronephrosis and ureterectasis. This led to the diagnosis of retroperitoneal fibrosis (RF) with renal failure, complicated by hypertension.Ureteral stents were placed, resulting in resolution of the renal failure and normalization of blood pressure.An endoscopic biopsy of the retroperitoneal mass was attempted without success.The patient was then administered prednisone, 40mg twice a day, resulting in dramatic shrinkage of the mass.
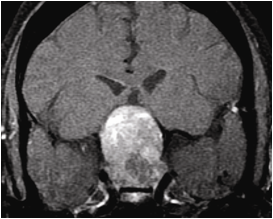
 | Figure 2. Axial post contrast T1 weighted MRI with fat saturation image reveals a focal intrasellar portion of the tumor that is relatively less enhancing compared to the rest of the tumor |
3. Neuropathology
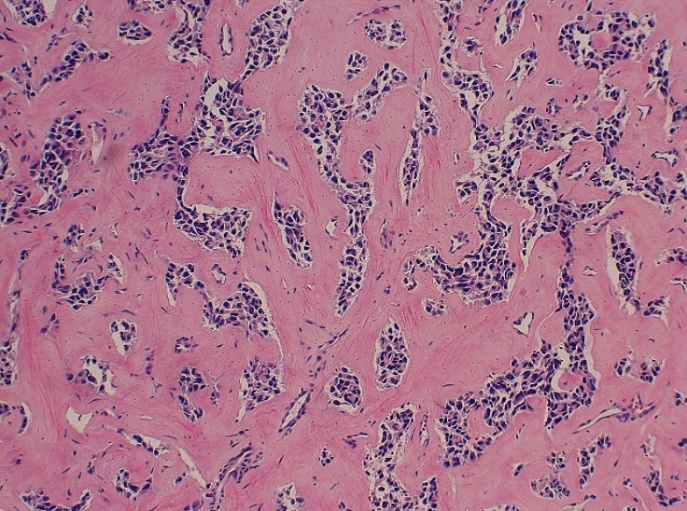
- Histologic examination demonstrated a pituitary adenoma with focal areas of dense, sclerotic stroma.In some areas, the adenoma maintained a classic appearance with rarefaction of the fibrovascular stroma and enlarged acinar structures containing characteristic monomorphic anterior pituitary endocrine cells without significant atypia (Figure 4).However, in other areas there wasan extensive sclerotic stroma within which the adenoma cells assumed an irregular trabecular configuration (Figure 5).There appeared to bea sharp transition between the classic area of adenoma and the extensively sclerotic area (Figure 6).
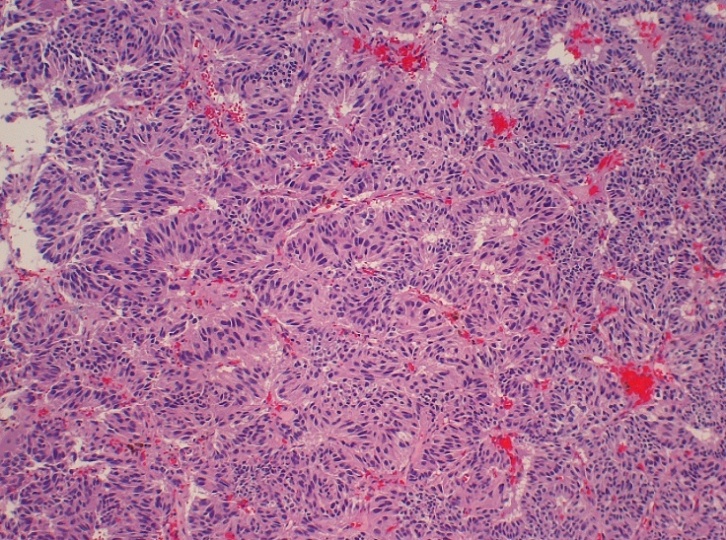 | Figure 4. Trabecular arrangement of tumor cells with bland nuclei, abundant cytoplasm, and a delicate fibrovascular stroma. H&E, 120x |
 | Figure 5. There is extensive stromal sclerosis within parts of the adenoma. H&E, 120x |
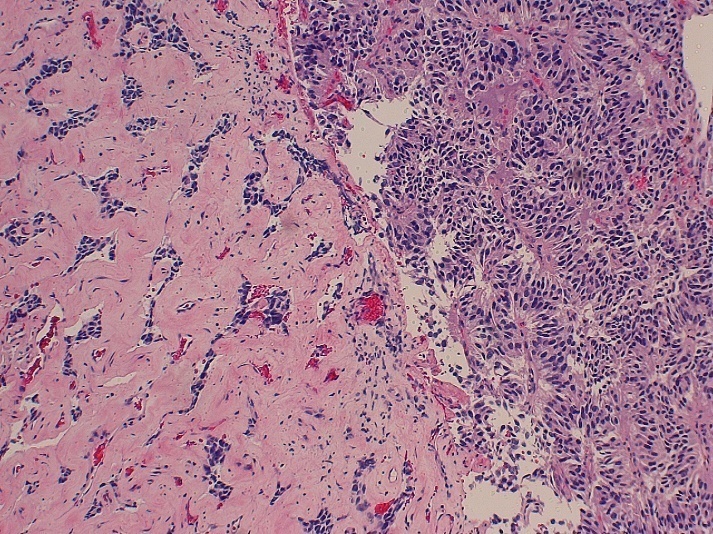 | Figure 6. There is a sharp transition between the sclerotic and more conventional portions of the tumor. H&E, 120x |
4. Discussion
- The presence of dense fibrous stroma in part of our patient’s pituitary adenoma along with the large suprasellar nodule suggests involvement by idiopathic sclerosing pachymeningitis, a reported component of multifocal fibrosclerosis[2].Fukuda and colleagues[2] described one case and identified six others that presented with retroperitoneal fibrosis and suprasellar masses.Three of these were consistent with sclerosing pachymeningitis with the remaining cases classified as either lymphocytic hypophysitis or nondescript fibrosis.There were no cases of pituitary adenoma.Thus, the specific combination of retroperitoneal fibrosis and sclerosing pachymeningitis producing a suprasellar mass, but without pituitary adenoma, appears to be a recognizable entity within the family of lesions comprising MFS. Sclerosing pachymeningitis presents as diffuse or localized thickening of the dura mater, with or without a chronic inflammatory infiltrate, and enhances on MRI scans after administration of gadolinium[3,4].Historically, tuberculosis or neurosyphilis was thought to be the cause of this condition, but more recent cases are primarily idiopathic[5].Presenting symptoms often include headache, radiculomyeloneuropathy, or cranial nerve palsies, and the disease follows a chronic course[3,4].Elderly men are generally more affected.Patients typically respond to steroid therapy, but about half will experience a relapse, especially as the steroids are tapered[4].Some of these patients will require additional immunosuppressive agents.Methotrexate, azathioprine, and cyclophosphamide have all been used successfully[2,4,5]. In recent years, the concept of IgG4-related sclerosing disease has emerged, characterized by inflammatory sclerosing lesions of exocrine glands such as pancreas and salivary glands, as well as other sites including retroperitoneum and dura[6,7].IgG4-related sclerosing disease apparently intersects with MFS, and cases of IgG4-related sclerosingpachymeningitis[8] and IgG4-related multifocal fibrosclerosis[9], involving pituitary stalk, paranasal sinus, and retroperitoneum have been described.Tissue biopsy prior to the initiation of therapy demonstrates fibrosclerosis with a lymphoplasmacytic inflammatory infiltrate[10].IgG4 levels in serum are elevated, and immunohistochemical study of the inflammatory infiltrate reveals increased numbers of IgG4-expressing plasma cells.Patients with IgG4-related sclerosing disease tend to respond well to glucocorticoid therapy with rapid reduction in the size of sclerosing lesions and resolution of clinical symptoms[6,11]. Our patient’s IgG4 level measured within the normal range when first tested about six weeks after initiation of high dose steroid therapy (44.1mg/dL; reference interval 4.0-86.0mg/dL).When measured recently with steroids tapered to 5mg per day, the IgG4 serum level was 77.0mg/dL, still well within the reference interval (4.0 – 86.0mg/dL).Since IgG4 was not measured prior to initiation of steroid therapy, it is impossible to determine what relationship our patient’s MFS syndrome might have had to an elevated IgG4 level.However, the rapid and dramatic shrinkage of the retroperitoneal mass is consistent with the steroid sensitivity that has been noted in cases of IgG4-related sclerosing disease.Further follow-up will be necessary before any conclusions can be drawn concerning a possible intersection of MFS (sclerosing pachymeningitis and retroperitoneal fibrosis) and IgG4-related sclerosing disease in our patient.
5. Conclusions
- We now add pituitary adenoma with sclerotic stroma to the previously reported cases of sellar fibrosis in MFS.As the association of pituitary adenoma and sclerosing pachymeningitis has not been previously reported, it is possible that the occurrence of pituitary adenoma in this setting is an unfortunate happenstance.In our case, it is likely that the densely fibrotic stroma of the large and well-vascularized pituitary adenoma necessitated increased intraoperative manipulation for adequate removal, and led to an increased risk of postoperative bleeding.Patients with MFS in its various forms and pituitary adenomas may be at increased risk for hemorrhagic complications due to both the anatomy of the tumor and the adherence of the tumor to the nearby normal anatomy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML