-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Composite Materials
p-ISSN: 2166-479X e-ISSN: 2166-4919
2015; 5(1): 18-24
doi:10.5923/j.cmaterials.20150501.03
The Clinical Applications of Fiber Reinforced Composites in all Specialties of Dentistry an Overview
Tabassum Tayab1, Akshay Shetty2, Kayalvizhi G.3
1The Oxford Dental College, Bangalore
2KGF Dental College, KGF
3Indira Gandhi Institute of Dental Sciences, Puducherry
Correspondence to: Tabassum Tayab, The Oxford Dental College, Bangalore.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Fiber reinforced composites are high strength filling materials composed of conventional composites and glass fibres. They exhibit extensive applications in different fields of dentistry. In the past decade, follow-up studies on fiber-reinforced composite used in various clinical situations have been described. Combining the results of these studies to draw conclusions about the effectiveness of FRC as a splint, appliance or FPD is challenging. The objective of this overview was to present the versatility of this material in all areas of dentistry. In addition, we explain the material properties and different techniques for each clinical scenario.
Keywords: Fibers Reinforced Composites, Bonded Retainers, Metal-Free Prostheses, Chairside Prostheses
Cite this paper: Tabassum Tayab, Akshay Shetty, Kayalvizhi G., The Clinical Applications of Fiber Reinforced Composites in all Specialties of Dentistry an Overview, International Journal of Composite Materials, Vol. 5 No. 1, 2015, pp. 18-24. doi: 10.5923/j.cmaterials.20150501.03.
Article Outline
1. Introduction
- Fiber reinforced composites (FRCs) have many clinical applications in dentistry because of the ability to manipulate the properties of composites to match with structural aspects. In addition the mechanical properties of FRC can be optimized to equal that of bone or dentin. This unique property has been tailored for dental needs by designing frameworks for crowns, anterior or posterior fixed prostheses, [1, 2] chairside tooth replacements, [3] posts, [4] and appliances such as space maintainers, [5, 6] periodontal splints [7] and orthodontic retainers. [8] (Figure 1)
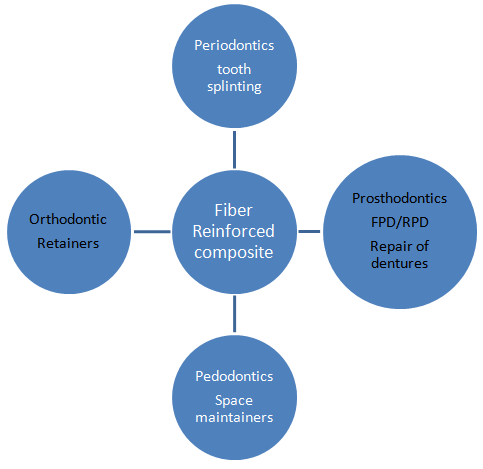 | Figure 1. Versatility of FRC in Various Dental Specialities |
2. The Two Approaches have Evolved Namely Non-Impregnated and Pre-Impregnated
2.1. Non Impregnated
- The non-impregnated fibers need to be wetted with an unfilled 4th or 5th generation bonding resin at chairside. A partially filled bonding resin should not be used to wet the Ribbond as they are more viscous and hence not self wetting. [13] While it provides complete wetting, this approach can be cumbersome, requires an additional step in the procedure and displays limited service as splints. It does, however, offer versatility in the selection of fibers.
2.2. Pre-Impregnated Fibers
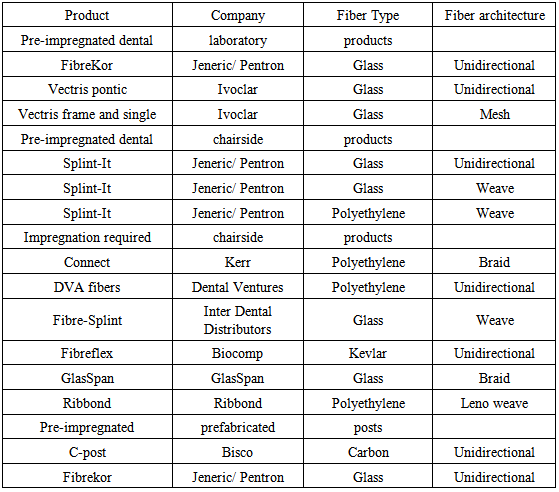
- In view of the fact that non-impregnated fibers lack good adhesion between the fiber and resin matrix compromising clinical longevity and freshly drawn glass fibers exhibit higher strength than ordinary glass fibers but are rapidly degraded on exposure to moisture and humidity. Immediate coating of these fibers with resin maintains the high strength values, thus the concept of pre-impregnation of glass fibers evolved (Splint-it). This is done by pre-impregnating the fiber bundles with resin during a controlled manufacturing process. [11] Glass fibers are pretreated with organo-silanes and polyethylene fibers are subjected to cold gas plasma treatment that increases their wettability and chemical bond. There are two types of glass fibers E-glass and S-glass of which E-glass is employed in dental materials. Another type known as C-glass was used in chemical applications requiring greater corrosion resistance to acids than is provided by E-glass. [12] (Table 1)
|
3. How FRC Materials Work
- The mechanical performance of FRC is influenced by several parameters. Increasing fiber volume leads to a greater increase in mechanical strength. The fiber architecture: unidirectional fibers long, continuous, and parallel followed by braided and woven fibers also increase flexural strength b van Hueman. Typically, fibers are 7 to 10 µm in diameter and span the length of the prosthesis or appliance. By comparison, the particles used in standard restorative dental composites are 1 to 5 µm in diameter, or submicron in size. Glass fibers of various kinds are commonly used in dental laboratory products, while polymeric reinforcements, such as ultra high molecular weight polyethylene, are often used for chair-side applications. Posts are made of carbon or glass fibers. • Woven fiber is less technique-sensitive, has lesser flexural strength and easier to manipulate hence conforms to the desired shape and maintains its adaptation during placement and is the ideal choice while making an appliance for rotated or malpositioned teeth. C Dyer et al • Unidirectional fiber has greater flexure strength and rigidity and is the better choice for high stress situations as in prosthodontic frameworks. [14]
4. Mechanical Properties
- For unidirectional fiber composites, in which fibers run parallel and in one direction, properties are highest in the direction parallel to the fibers and lowest in the direction perpendicular to the fibers. [14] As a result, restoration and appliance designs seek to place the reinforcing fibers parallel to the areas with highest stresses. In a posterior bridge the pontic is a freestanding structural component subjected to immense force. Hence the pontic bar is made up of unidirectional fibers and then multiple layers of fibers are wrapped around the pontic bar spanning the abutments to reinforce the pontic multidirectionally. In anterior bridge the incisal edge of the anterior pontic is not as wide and therefore a pontic bar made of unidirectional fibers will suffice. [15]
5. Fiber-Reinforced Fixed Prostheses (FRC FPD)
- FRC FPD’s consist of a framework made of glass fibers onto which a particulate composite veneer is made. They are fabricated in the dental laboratory to minimize chair time and optimize esthetics and mechanical properties. FRC FPD’s are versatile and can be used in a variety of clinical situations and are accordingly classified as complete coverage or partial coverage FPD’s depending on the case. They vary from complete crown-retained FPDs in terms of procedure, as 1) onlay- complete coverage 2) inlay-intra coronal preparations 3) surface-retained FPDs. [16]Tooth preparations made for complete coverage FRC FPD require a shoulder or chamfer preparation with minimally tapered axial walls and smooth continuous finish lines (with 90-120 degree) cavosurface angle placed above the cervical third of the tooth. Additionally 1.2 – 1.5 mm axial reduction on the facial and lingual surfaces and 1.5 mm occlusal reduction are required for adequate thickness. The survival rate of single pontic complete coverage FRC FPD was reported by Frielich et al to be 95% after a 4.3 year follow upd. In contrast Vallittu reported a 75% survival rate after a follow up of 24-36 months. This difference could be attributed to the lower modulus of elasticity that enables the prosthesis to debond during function. eThe intra coronal type is used when the tooth adjacent to the edentulous space has an existing restoration. The tooth preparation for this type of FRC FPD requires the placement of a proximal step and isthmus to enhance retention. The proximal step is 3-4 mm wide and 1 mm deep on axial walls adjacent to edentulous space. An occlusal isthmus is placed in posterior abutment teeth (0.5 mm deep and 2-3 mm wide) and a lingual step on anterior abutment preparations. One of the factors that affects the strength of inlay retained FPD’s is the dimension of the proximal box. This allows for sufficient material at the connector area and also gives the technician a positive stop for placing the pontic FRC support. The isthmus allows for a continuous I-beam configuration of FRC over each abutment tooth and across the edentulous space. In the hand fabricated framework (FibreKor) for anterior tooth preparations an additional step or double shoulder configuration on the lingual surface is provided to avoid creating a retainer with an over contoured lingual axial surface. [17] Jain & Cobb reported a 95% survival rate for singke pontic inlay retained FRC after a 4.5 year follow up. F A meta analysis by Cruegers and van’t Hof found a 75% survival rate with maxillary frameworks surviving longer than mandibular frameworks. The failure for this type of FRC was delamination of the veneering resin under masticatory laods of 300-500N indicating that they are suitable for clinical application. However the clinical longevity is largely influenced by the fiber system used eg: E-glass fibers and indirectly fabricated FRC’s demonstrated higher functional survival rates.gThe final impressions, dies and working casts for both onlay and inlay preparations should be made using conventional methods and materials. The laboratory fabricated framework commonly employs two commercially available pre-impregnated systems. They are Targis/Vectris, Ivoclar available as unidirectional and woven glass forms which require custom made matrices and special equipment and Sculpture/ FiberKor (Jeneric/Pentron) that uses hand fabrication to form the framework. The unidirectional glass fibers are preferred for FRC FPD and they are first used to form the pontic bar. It is then covered with woven fibers by circumferential wrapping of the FRC around the axial walls of the abutment teeth. The final anatomic form of the pontic is obtained by placement of particulate composite overlay. The completed prosthesis is then cured in a special oven for 15 minutes after which is it finished and polished prior to delivery. Care should be taken to place the pontic bar above the proximal contact area as this will facilitate the placement of the final gingival form with particulate composite. Hence it is important for the dentist to be familiar with the design features of FRC prosthesis as the tooth preparation requirements are different for each type and are critical to the success of the FRC framework. The flexure strength values for laboratory–processed FRC range from approximately 300 to 1,000 MPa. [15, 18] The procedure for surface retained FRC FPD is similar to the extra coronal splinting method the only difference being that a denture tooth is attached to the fiber.
|
5.1. Chairside Applications of FRC
- Tooth stabilization is required in periodontally compromised teeth, [19, 20] after traumatic injuries or of after orthodontic treatment. [21, 22, 23] This is easily fabricated at chairside using FRC technology. It can be of two types intracoronal and extracoronal. In the intracoronal method lingually a retention horizontal channel 2-3 mm wide and 1-2 mm deep is prepared in the middle to incisal third of the teeth to accommodate the thickness of the fiber. Both pre-impregnated and non-pre-impregnated fibers are used for stabilization. [24-26] The technique for chairside FRC prosthesis is the same and the pontic that is used can be an extracted tooth or denture tooth and is bonded to the fiber. [27-29] In extra coronal method no tooth preparation is required and is based on adhesive retention. In mandibular teeth it is placed lingually and in the maxillary teeth it can be either facial or lingual. The fiber is embedded in composite and light cured. In both types 30% of the failures were due to debonding over a 2.5 year follow-up and the presence of a retentive groove did not improve survival rates. Although FRC is added to composite to increase the enamel resin bond strength Meir’s et al did not find any significant difference in bond strength of composite alone and composite reinforced with glass or polyethylene fibers. Connect seemed to demonstrate the highest bond strengths whereas Splint-It woven, Slint-It unidirectional and Ribbond did not significantly increase the bond strength of composite. Hence this technique can be a viable alternative to metal- resin bonded FPD’s especially in the restoration of a single anterior tooth or for splinting teeth for a short time. h
5.2. FRC for Posts
- The requirement of fiber reinforcement as post for endodontically treated teeth are that they should have physical properties such as modulus of elasticity, compressive strength and thermal expansion and esthetics similar to that of dentin and it should bond predictably to root dentin. A prefabricated FRC root canal post consists of reinforcing fibers of a predetermined diameter embedded in a fully polymerised resin matrix between the fibers [7, 12]. The problem with this material is that the polymer matrix between the fibers is highly cross-linked and due to the high degree of conversion is non-reactive. This makes it difficult to bond the prefabricated FRC posts to composite resin cement and tooth structure. This difficulty in bonding is overcome by embedding glass fibers in a semi interpenetrating polymer network (semi-IPN). [30] The semi-IPN structure, consists of both linear polymer phases and cross-linked polymer phases mixed at the level of polymer chains thereby allowing monomers of the adhesive resin and cements to diffuse into the linear polymer phase and form an interdiffusion bonding, called a secondary- IPN bonding by polymerization. The flexural moduli but not the flexural strengths of FRC posts appear to correlate with fiber type. [31] The FRC posts form a single bonded complex within the root canal and improved esthetics when used with all-ceramic or FRC crowns as compared to custom-made cast or metal-prefabricated posts.Two categories of FRC posts are available: ● Chairside-fabricated and prefabricated. Chairside fabricated posts are custom designs that use polyethylene non-pre-impregnated woven fibers (Ribbond, Connect) or glass fibers (GlasSpan). [32] ● Prefabricated posts are constructed of two kinds of fiber: carbon fibers (C-Post, U-M C Post and Aestheti-Post) [33] and S-type glass fibers (FibreKor Post) [34].
5.3. Repair of Acrylic Resin Prostheses
- FRC strips can be used effectively for chairside repairs of fractured acrylic resin prostheses. If a denture is cracked but still in one piece a T-shaped cavity approximately 1.5 to 2.0 mm deep is created over the crack. The surface of the cavity is wetted with acrylic resin monomer and then with unpolymerized special resins (Jeneric/Pentron) which provides an adhesive surface for tacking the FRC. Four or more strips of unidirectional or woven FRC are cut to size and placed horizontally over the fracture and light polymerized for four minutes. It is then filled with acrylic resin. The finished prosthesis is placed in a pressure pot with warm water at 20 psi for 15 minutes. It is then removed, pumiced and polished. If the prosthesis is fractured in two halves it is placed over a stone cast to maintain the orientation of the two segments throughout the repair. The entire fracture site is opened up with a carbide bur and prepared with acrylic monomer and then with the unpolymerized special resin. The fracture site is filled with multiple strips of FRC and light cured. The remaining cavity is then covered with resin and the same procedure as above is repeated. [14]
5.4. Reinforcement of Provisional Acrylic Resin Prostheses
- When dentures oppose with natural teeth or implant supported prosthesis fractures of maxillary dentures are very common. To overcome this drawback the dentures can be reinforced with FRC. Reinforcement can also be extremely useful with long-span provisional FPDs in patients with destructive parafunctional habits and when only minimal space is available for the acrylic resin. [35, 36]
5.5. Implants
- Implants are routinely restored with overdentures, fixed partial dentures or hybrid prostheses. However the standard metallic or cylinder form abutment has proven unacceptable for hybrid prostheses due to limitations in bonding hence FRC can be bonded and retained successfully especially in short edentulous spans. [37] Another advantage is the development of the papilla at the implant site as osseous integration takes place. Since these FRC FPD’s are provisional restorations the choice of glass or polyethylene fiber used as re-inforcement is not very critical as both give excellent survival rates as short term restorations.i
5.6. Fiber reinforced Composite Space Maintainers
- Owing to the success of FRC in other specialties of dentistry its potential in space maintenance in primary and permanent dentition is gaining popularity. Both polyethylene and glass fibers have been used to fabricate simple unilateral fixed space maintainers (SM). Subramaniam et al compared band and loop SM using stainless steel and glass fibers (Everstick, Stickteck Ltd, Turku, Finland) in children aged 6-8 years in both arches for premature loss of first primary molar and found that FRCSM demonstrated superior retention to stainless steel band and loop SM after one year follow up.38 Kulkarni fabricated loops using Stickteck and Ribbond fibers both measuring 2mm and 4 mm using stainless steel loops as controls and evaluated their flexural strength and bacterial colonization in an in vitro study. The 4mm Ribbond fiber demonstrated better flexural strength than Sticktech and control and this was attributed to the greater surface area available for bonding thereby increasing retention.39.Mainly band and loop types and functional space maintainers with one tooth when used for a short time have shown promise as alternatives to stainless steel space maintainers. The clinical performance of FRCSM was found to be 7.17 months for the maxilla and 6.69 months in the mandible. FRCR space maintainers holding space for 1 tooth lost survived longer than space maintainers for 2 teeth lost. Kirzioglu in his study, found that the space maintainers placed on primary teeth (1 or both abutment teeth) showed the highest failure rate (94%). One possible explanation for this low success rate may be attributed to the presence of prismless enamel areas, which may negatively influence resin retention. Another possible reason is complete salivary isolation is difficult in children.The FRCSM designed in most studies were applied without preparing grooves on the abutment teeth to prevent unnecessary loss of tooth structure. This may be another reason for the short functional life of the appliance. The commonest mode of failure observed was debonding rather than fracture of framework. Hence the success of FRCSM relies on the skill of the operator and case selection. The clinical advantages of the FRCSM are that they provide reduced chairside time, cost do not require a cast model; easy to apply; provide reliable adhesive bonding and retention; can be used in cases of metal allergy and provided a natural feel and esthetic.40.Many studies on FRCSM have demonstrated that they need not be removed and inspected once every six months, do not cause harm to adjacent teeth as they are placed well above the gingival margin and do not get embedded in gingival tissue. Inspite of these advantages FRCSM can be accepted as successful appliances only for short periods and more long term studies are required for advocating FRCSM in routine clinical practice.
6. Conclusions
- In dentistry both glass and polyethylene fiber has tremendous potential as reinforcement but understanding the unique characteristics of each fiber type will enable the clinician in making appropriate choices during framework contruction. Unidirectinal pre-impregnated glass fibers that have greater fiber volume impart greater flexural strength and modulus of elasticity and are ideal for direct/laboratory prosthodontic frameworks. The flexural strength of polyethylene fibers is less compared to glass fibers and are ideal as provisional restorations such as splinting or direct adhesive bridge. The ease of fabrication, easy repair and esthetic properties have ensured that FRC has great promise in all areas of clinical and laboratory dentistry.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML