Osahon O. D.1, Ojo O. A.2, Ushie P. O.3
1Department of Physics, University of Benin, Benin City, Nigeria
2Department of Physics, Osun State University, Osogbo, Nigeria
3Department of Physics, Cross River University of Technology, Calabar, Nigeria
Correspondence to: Ojo O. A., Department of Physics, Osun State University, Osogbo, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
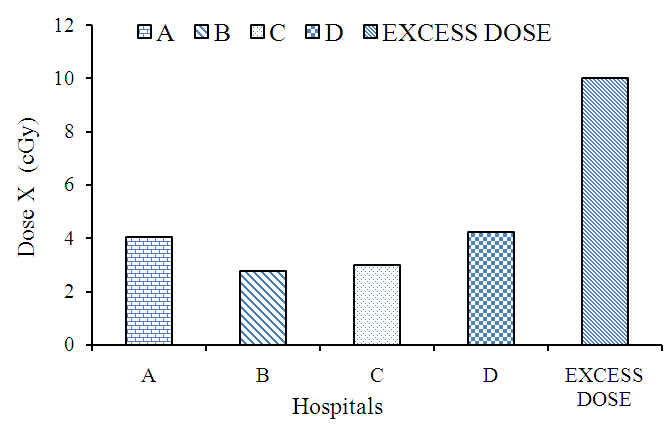
Medical Imaging accounts for the largest radiation exposure of population from artificial sources of radiation. The radiation dose received by patients from medical X-ray examinations in Nigeria has shown large variations within and among diagnostic centers for similar examinations. This could be traced to lack of imaging protocols and availability of local or national diagnostic reference levels. The purpose of this study is to use film densitometry to estimate radiation absorbed dose to patients undergoing chest X-ray examination in the hospitals where this study was carried out, in order to determine their levels of exposure and compare with internationally recommended limits.Although the radiation doses resulting from diagnostic X-ray examinations are routinely measured in terms of entrance surface dose and effective dose using thermoluminescent dosimeter (TLD), optically stimulated luminescent dosimeter (OSLD), film badges, pocket dosimeter and electronic personal dosimeter (EPD). In this study for the purpose of radiation protection, the radiation doses from chest X-ray examination were estimated in terms of Mean Optical Density (MOD), by means of densitometer; model MA 5336, with a range of 0 to 4.0 optical density, an accuracy of ± 0.02 density and reproducibility of ± 0.01 density, manufactured by Gammex, U.S.A. The hospitals where this study was carried out are: hospital A in Ondo State; hospital B in Oyo State; hospitals C and D in Osun State. A total of one hundred and fifty five (155) chest X-ray radiographic films were collected from these hospitals in South – West Nigeria. The optical density of each radiographic film was measured five times at different spots. The MOD was obtained and a mathematical relation was used to convert the MOD to absorbed radiation dose in centi Gray (cGy). The results obtained in this study show that the mean absorbed X-ray dose was 4.04 ± 2.06 cGy in hospital A, 2.77 ± 1.45 cGy in hospital B, 3.01 ± 1.33 cGy in hospital C and 4.23 ± 1.98 cGy in hospital D. These values were compared with the excess dose of 0.10 Gy recommended by International Commission on Radiological Protection (ICRP, 2000), which is considered injurious or harmful to the human body.The absorbed radiation doses to patients at the different hospitals were observed to vary slightly and the percentage of mean absorbed dose above the excess dose was 1.9% of the total number of the films.
Keywords:
Absorbed radiation dose, Densitometer, X-ray radiographic film, Mean optical density
Cite this paper: Osahon O. D., Ojo O. A., Ushie P. O., Estimation of Radiation Absorbed Dose to Patients Undergoing Chest X-ray Examination in Four Government Own Hospitals in Nigeria, International Journal of Biophysics , Vol. 7 No. 2, 2017, pp. 24-32. doi: 10.5923/j.biophysics.20170702.02.
1. Introduction
One of the most frequently required diagnostic procedures used in clinical practice is chest X-ray examination and it may also be implemented in screening programs for large populations with significant impact on the collective dose [1]. According to ICRU report 70, chest radiography is responsible for approximately twenty five percent (25%) of all X-ray examination performed [2]. Increasing concern for the potentially high radiation dose in fluoroscopy guided international procedures has led to the use of a variety of techniques to monitor patience dose [3-6]. Some X-ray machines of recent design are able to provide information on radiation exposure in the form of absorbed dose. An example of such device would be a large area ionization chamber installed in the X-ray machine, which would allow radiation input to be measured directly. For X-ray machines lacking similar capability, it would be desirable to find an alternative means to measure radiation output. Radiographic film is use to record the skin entrance radiation exposure. It has the ability to record high radiation dose [7]. The radiographic film could therefore be an alternate means to record absorbed dose. Such possibility was investigated here by placing the film at the output of an X-ray tube assembly and then measuring the film response by a hand held densitometer [8]. Optical density (D) is the degree of blackening of the radiographic film image, as a result of the X-ray energy deposited on the film. It is a dimensionless quantity. The radiographic film is the image-receptor, where the image of the X-rayed object is formed [9-11]. The final image of the object can be developed for further use by the radiographer or radiologist. Note that there are different types of radiographic film manufacturers, but they all achieve the same purpose of X-ray radiography [12]. When measuring the dose absorbed in a human due to X-ray exposure, unit of absorbed dose is used, which is the centi Gray (cGy), in the SI system of units [13].In this study, for the first time in Nigeria, the radiation doses from chest X-ray examination were obtained in terms of MOD of radiographic films via an established equation. The result obtained was compared with the work of Artur, 2003 and the excess dose of 0.10 Gy. This study is a pilot study to estimate patients absorbed radiation dose in chest X-ray examination using radiographic films in Nigeria. This research work is intended to provide users of X-ray equipment one means of achieving compliance with the International Commission on Radiological Protection recommendation [14].
2. Materials and Method
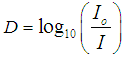
Samples of adult chest X-ray radiographic films were collected from four public and busy hospitals across the South - West Zone of Nigeria. The hospitals are: Hospital A, in Ondo State; Hospital B in Oyo State and Hospitals C and D in Osun State.The following abbreviations were adopted for the purpose of this study:Optical density: DAbsorbed X-ray dose: X Mean Optical Density: MODMin: MinimumMax: MaximumkVp: kilovolt peak (X-ray tube voltage)mAs: milliampere second (X-ray exposure time)SD: Standard Deviation1st Q: First Quartile3rd Q: Third QuartileThe optical density (D), of the radiographic films was measured repeatedly five times at different spots on each film as optical densities D1, D2, D3, D4 and D5 with a densitometer, model MA5336, with a range of 0 to 4.0 optical density an accuracy of ± 0.02 density and reproducibility ± 0.01 density, manufactured by Gammex, U.S.A. This was done for each radiographic film. The mean of the five optical densities was then taken to obtain the Mean Optical Densities (MOD). The optical densities were converted to the absorbed X-ray radiation doses X, in centi Gray (cGy), which is the amount of X-ray radiation dose that each patient has absorbed. The various standard deviation (SD) was also estimated for each Mean Optical Densities (MOD) of the radiographic film and the absorbed X-ray radiation dose X.The blackening of the film after X-ray radiation exposure is expressed in terms of its optical density as [15]: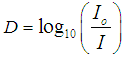 | (1) |
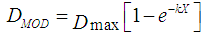
where Io and I is the light intensities before and after passing through the exposed film material.Optical density is a numerical value indicating the degree of blackening on an X-ray radiographic film.The correlation between the optical density D and the maximum number of sensitized grains results in a relation between the optical density D and the absorbed dose X, as,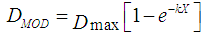 | (2) |
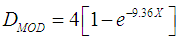
where, Dmax = 4 and k = 9.36 [15] Therefore, equation (2) for the optical density becomes,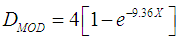 | (3) |
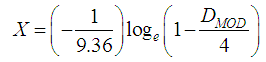
Solving equation (3) for the absorbed X-ray radiation dose X, gives,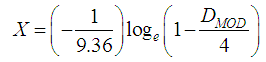 | (4) |
Equation (4) was developed into a densitometric software simulator to perform the task of calculating the amount of the absorbed X-ray dose X (cGy) for each radiographic film from the MOD. The software runs on the WAMP server (Windows Apache MySQL PHP), with the following languages used PHP, MySQL, JavaScript, Html, and CSS, which can be applied remotely with internal or external networks anywhere. The standard deviation (SD),  , of each of the measured optical densities (D) was estimated from the relation:
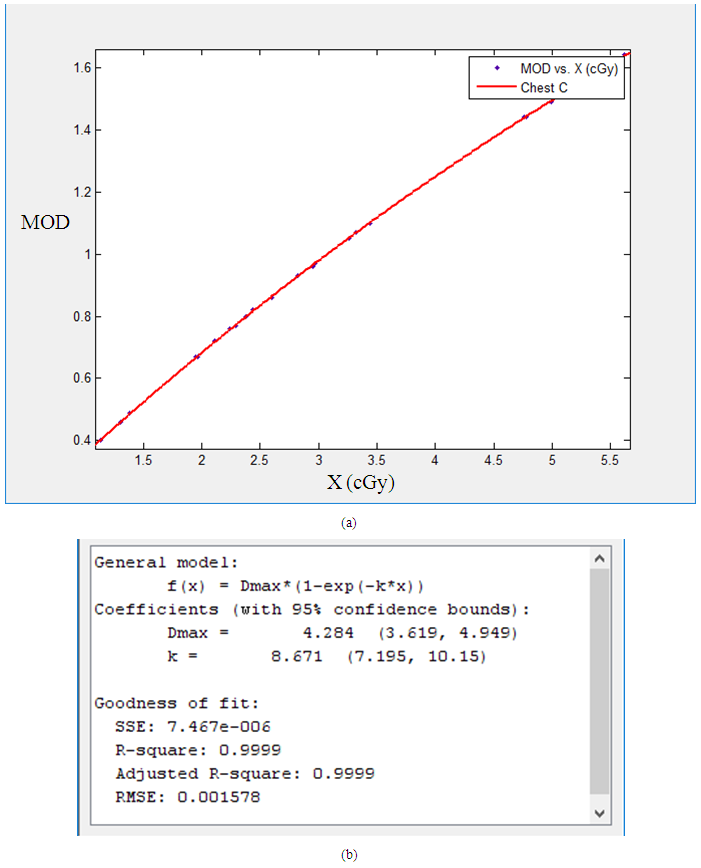
, of each of the measured optical densities (D) was estimated from the relation: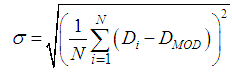 | (5) |
where:N: is the total number of times the optical densities were measured per radiographic film. : is the optical density of each radiographic film.
: is the optical density of each radiographic film. : is the Mean Optical Density (MOD) of the radiographic film.
: is the Mean Optical Density (MOD) of the radiographic film.
3. Results and Discussion
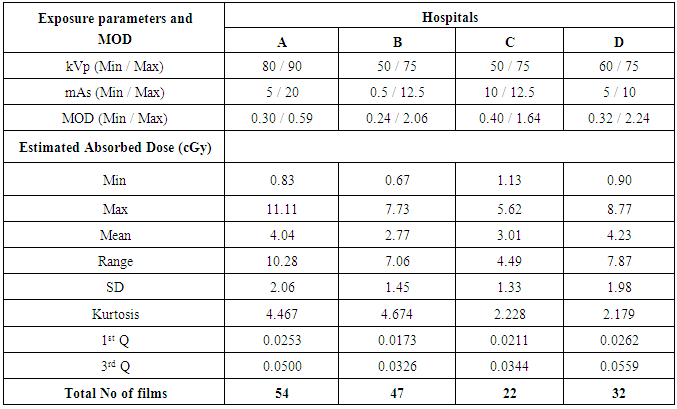
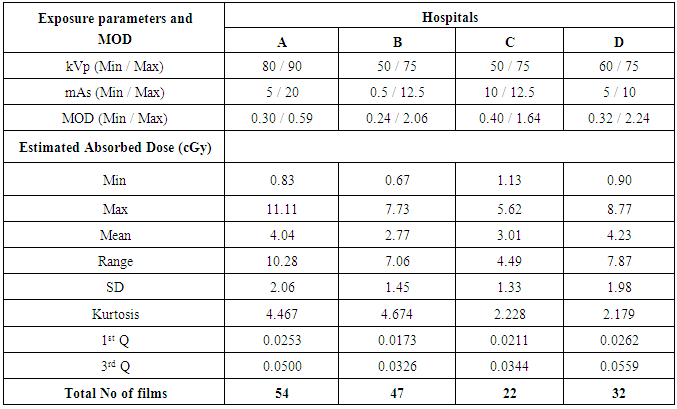
Exposure parameters were collected from the selected hospitals. The results are summarized in Tables 1, 2 and 3.Table 1. Exposure parameters and descriptive statistics of the estimated absorbed dose
 |
| |
|
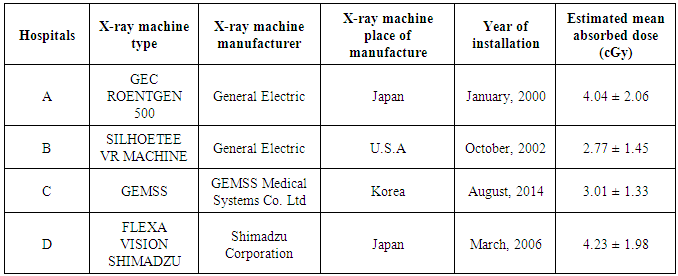
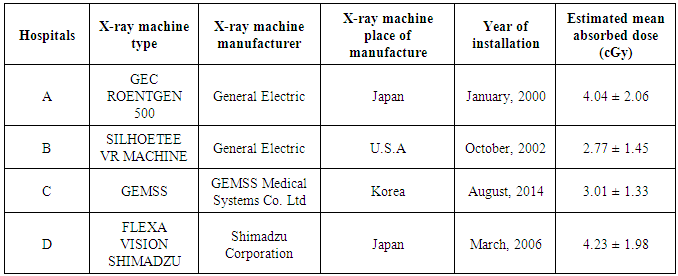
Table 2. X-ray machine type, manufacturer, place of manufacturer, year of installation and estimated mean X-ray dose (cGy) with standard deviation
 |
| |
|
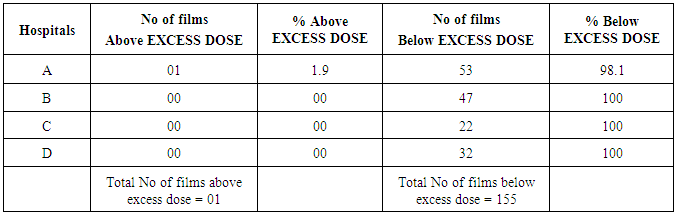
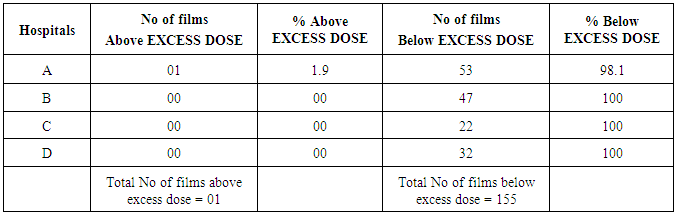
Table 3. Percentage of estimated mean absorbed dose above and below excess dose
 |
| |
|
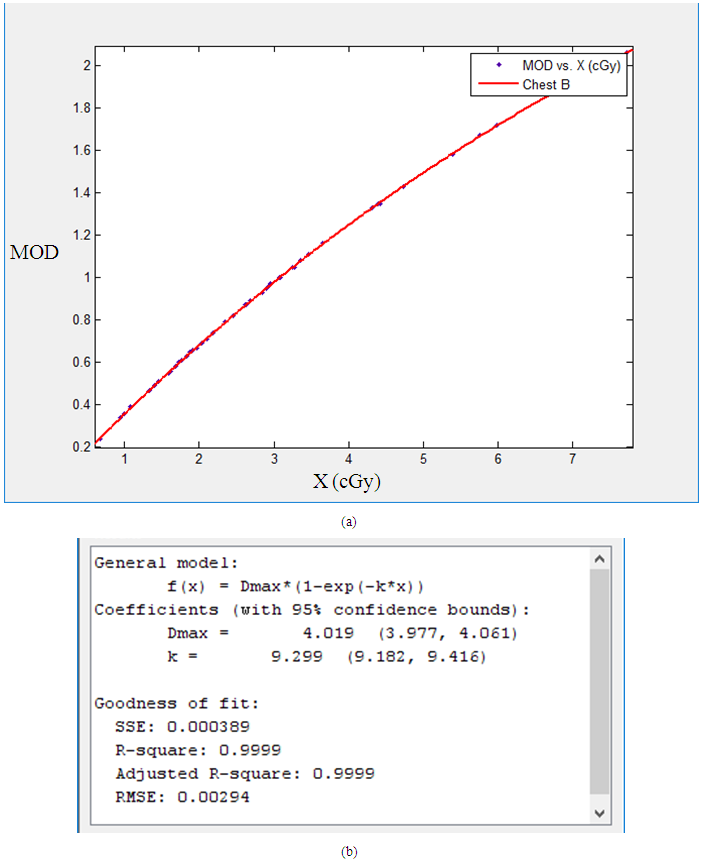
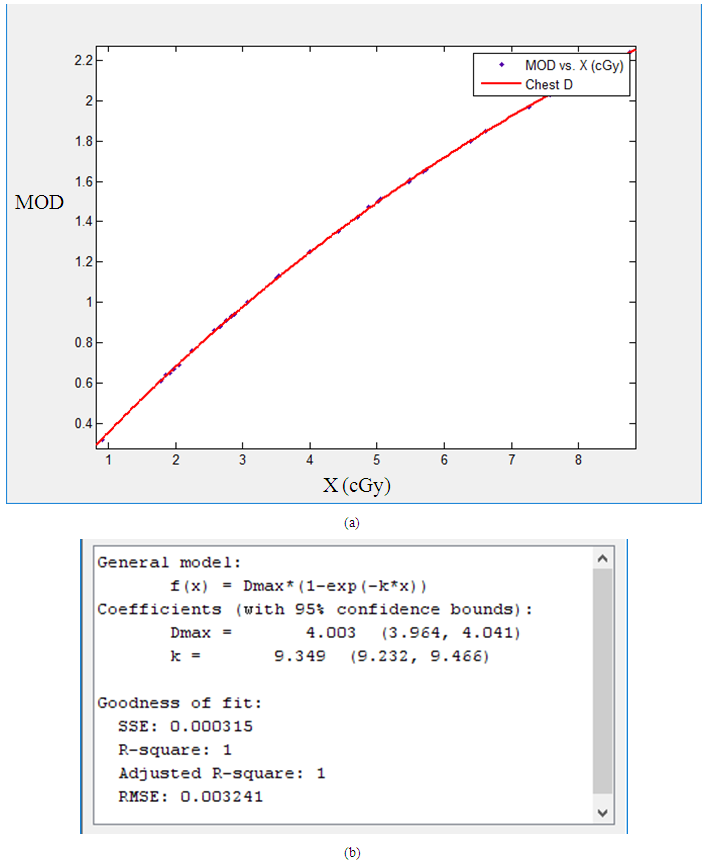
Table 1 presents the exposure parameters of the X-ray machines and the descriptive statistics of the estimated absorbed dose. The values of the absorbed X-ray radiation doses, X (cGy), vary from one hospital to the other. The characteristic curves for the optical density (D) against the absorbed X-ray radiation dose (X) for each of the four hospitals were plotted as shown in Figures 1 to 4. Figure 5 is a bar chart of mean doses in this study compared with excess dose. While it is not possible to attribute the causes of variations in the doses at the hospitals to only one factor, the causes are however, multifactorial. Such factors include: technical parameters, patients size, film screen speed, filtration, radiographic technique and perhaps the condition of the X-ray machine with particular emphasis on the year of installation. It is observed in this study, from the X-ray machine in hospital D, the highest mean absorbed dose value was obtained.According to [16], National Diagnostic Reference Levels (NDRLs) is not universal but specific to a country, equipment and training of personnel. They concluded their study with emphasis on the need for national diagnostic reference levels and local diagnostic reference levels for dose optimization in Nigeria. Although mean absorbed dose disparity is expected among the hospitals, presently there is no NDRLs in Nigeria to compare the results of this study with. However, a comparison of the results of the study with the work of Artur (2003) shows that the mean absorbed doses in this study compare favorably with the mean absorbed doses of 7.61 cGy and 10.8 cGy respectively obtained in two hospitals where Artur’s study was carried out. The values of the absorbed X-ray radiation doses can be seen to be large for optical densities greater than 1.0 and tends to a maximum value around optical density of 4.0.The curve fittings in this study were done using Matlab and the best fit was obtained using a custom equation. The result of the fit contains General model, coefficients (confidence bounds), the maximum optical densities and the conversion constant k. The Goodness of fit also contains the Sum of Square Error (SSE), R – Square, Adjusted R – Square and Root Mean Square Error (RMSE). These results are replicated throughout the hospitals. 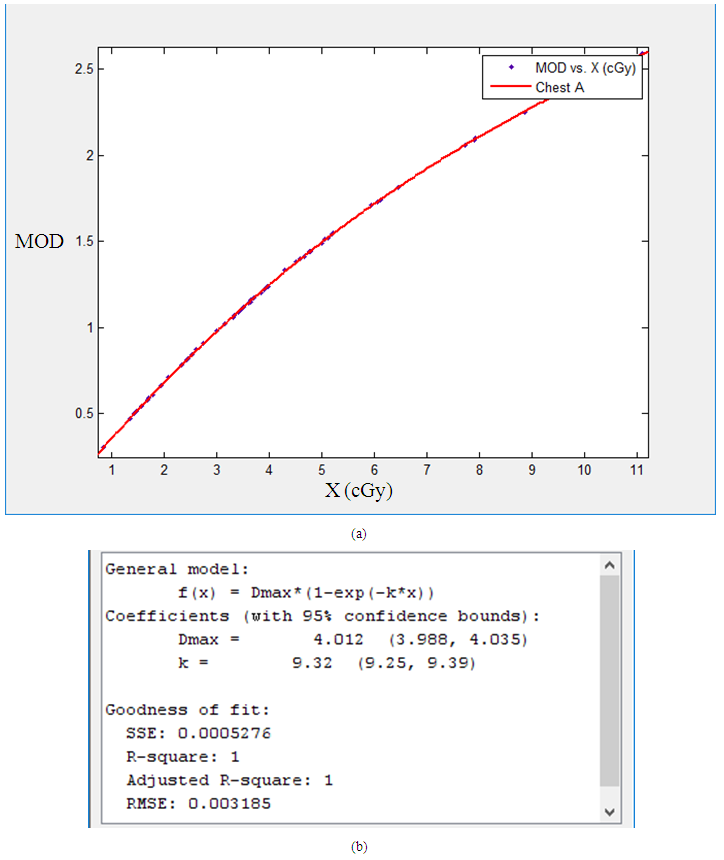 | Figure 1. (a). Graph of mean optical density (DMOD) vs absorbed X-ray radiation dose (X) for chest examination in hospital A (b). Results of the fit |
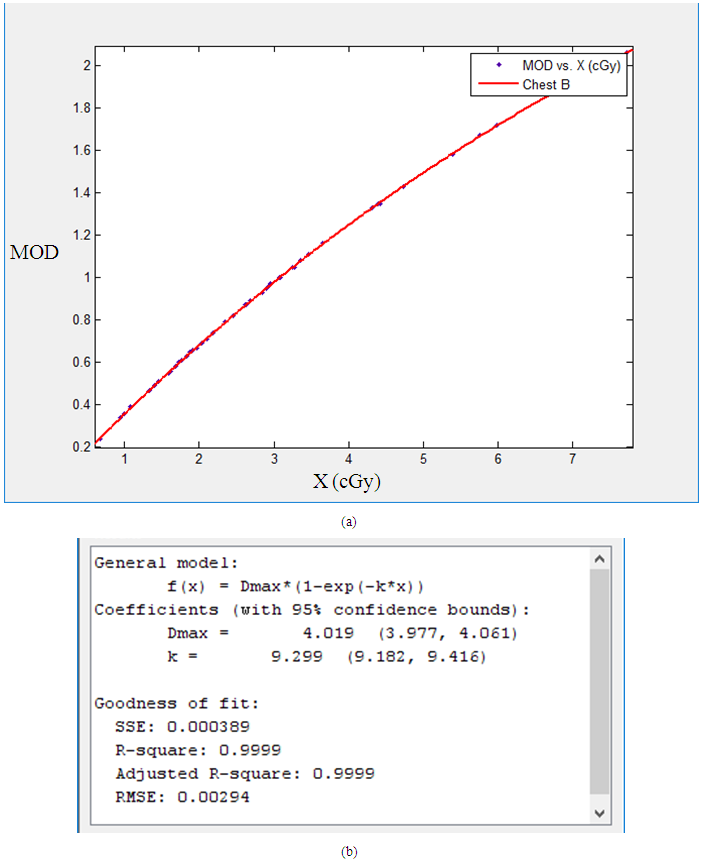 | Figure 2. (a). Graph of mean optical density (DMOD) vs absorbed X-ray radiation dose (X) for chest examination in hospital B (b). Results of the fit |
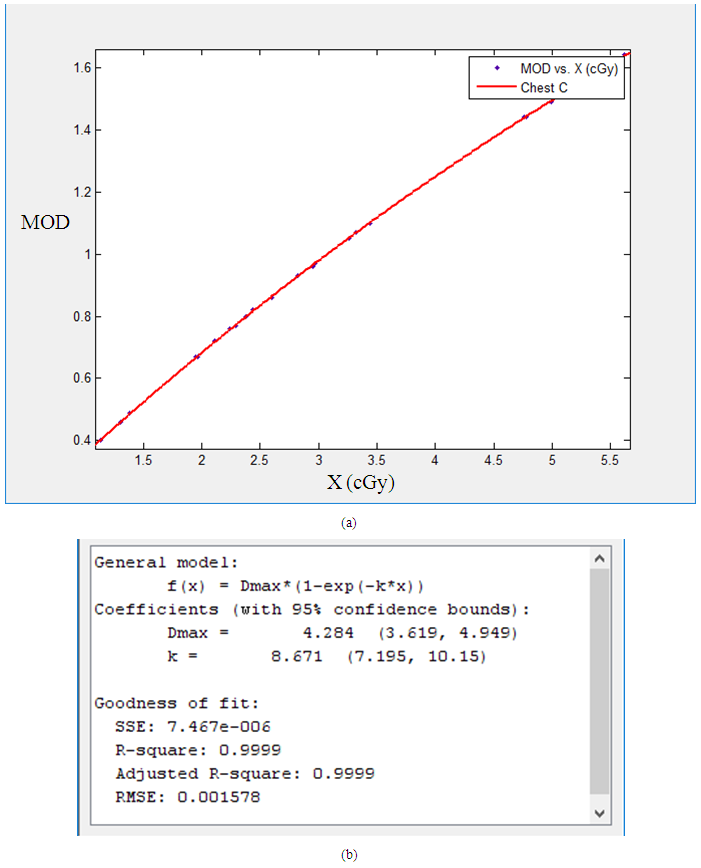 | Figure 3. (a). Graph of mean optical density (DMOD) vs absorbed X-ray radiation dose (X) for chest examination in hospital C (b). Results of the fit |
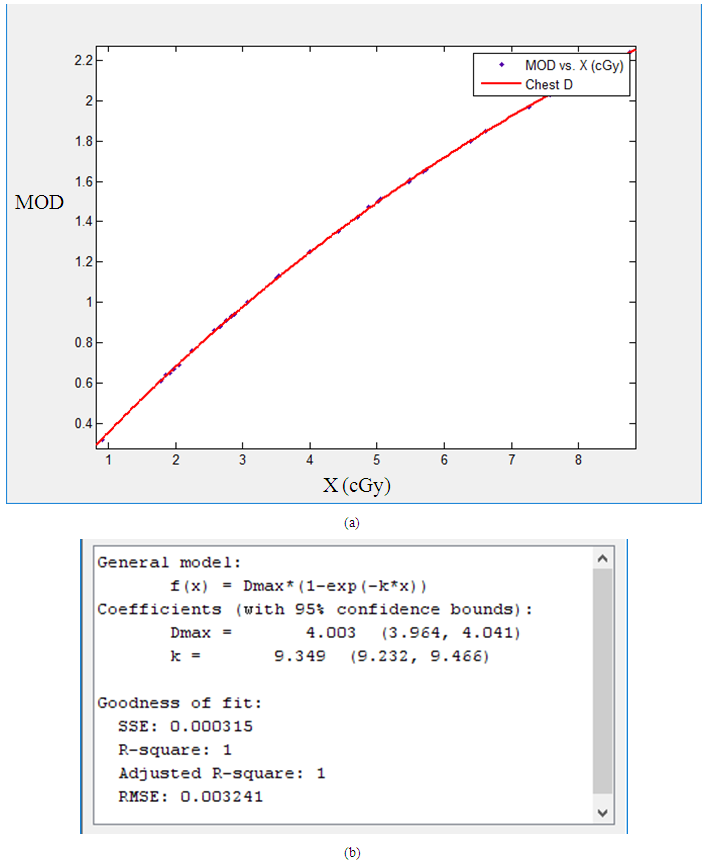 | Figure 4. (a). Graph of mean optical density (DMOD) vs absorbed X-ray radiation dose (X) for chest examination in hospital D (b). Results of the fit |
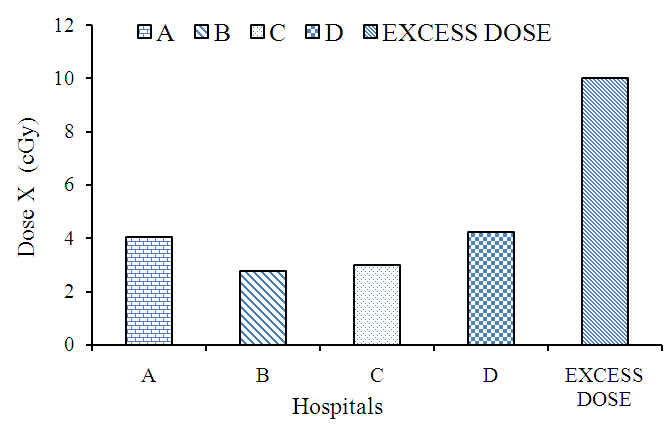 | Figure 5. Bar chart of mean X-ray radiation dose in the four hospitals and excess dose |
4. Conclusions
This study has shown that the absorbed radiation doses to patients at the different hospitals were observed to vary slightly and 1.9% of the total films available recorded excess dose. This study can be adopted for Quality Assurance (QA) and Quality Control purposes, to guide against excess radiation dose to patients during the course of an X-ray examination. Further work is necessary to define appropriate procedures for optimization of patient’s dose and adopting correction actions.
ACKNOWLEDGEMENTS
The authors will like to thank the authority and staffs of the four hospitals for allowing access to their premises and facilities.
References
| [1] | Salat D. and Nikodemova D. (2008). Patient doses and image quality in digital chest radiology. Radiat. Prot. Dosim. 129: 147 - 149. |
| [2] | ICRU (2003). International Commission on Radiation Units and Measurements. Image quality in chest radiography. ICRU Report 70, ISBN 1473 – 6691. |
| [3] | Chu R.Y.L., Perry C., Thompson III W. and Loeffler C. (1998). Patient doses in abdominal aorta grams and aorta femoral run off examinations. Health Phys.; 75:487–491. |
| [4] | Giles E.R. and Murhpy P.H. (2002). Measuring skin dose with radiochromic dosimetry film in the cardiac catheterization laboratory. Health Phys.; 82:875–880. |
| [5] | Miller D.L., Balter S., Noonan P.T. and Georgia J.D. (2002). Minimizing radiation-induced skin injury in interventional radiology procedures. Radiology; 225:329–336. |
| [6] | Koenig T.R., Mettler F.A. and Wagner L.K. (2001). Skin injuries from fluoroscopically guided procedures. II. Review of 73 cases and recommendations for minimizing dose delivered to the patient. AJR Am J Roentgenol; 177:13–20. |
| [7] | Thomas G., Chu R.Y.L. and Rabe F. (2003). A study of Gaf Chromic XR Type R film response with reflective-type densitometers and economical flatbed scanners. Am Coll Med Phys.; 4(4). Available at http://www.jacmp.org/archive/vol_4/iss_4/307_1.pdf. |
| [8] | George T., Yushan Li., Robert Y.L. Chu, John Y.C, Feroz M., Frank R. and Scott G. B. (2005). Measurement of dose area product with GafChromic XR Type R film. J of App. Cl. Med.Phy. vol 6. No 3. Received 20 August 2004; accepted 25 February 2005. |
| [9] | www.megaslides.com (2016). Film optical density. |
| [10] | www.researchgate.com (2016). Optical density, a dimensionless quantity. |
| [11] | www.studystack.com (2016). Spatial resolution improves with decreased blur. |
| [12] | Serman N. and Singer S. (2016). Intensifying screens, cassettes and screen films. Publication Number: US9324469 B1. Publication type: Grant. Application number: US 14/530, 426. Publication date: 26 Apr 2016. Inventors: Geraldine M. Hamilton. Original Assignee: Geraldine M. Hamilton. |
| [13] | www.sprawls.org (2016). Radiation quantities and units. |
| [14] | ICRP (2000). International Commission on Radiology Protection). Publication 85. Ann ICRP; 30(2). Avoidance of Radiation Injuries from Medical Interventional Procedures. ICRP Reg. No. 52/261/01. |
| [15] | Artur T. (2003). Determination of Absorbed X-ray Radiation Dose in X-ray Diagnostics and Imaging. Journal of Medical Sciences. Vol 1. No 2. pp 31-36. |
| [16] | Olowookere C.J., Babalola I.A., Jibiri N.N., Obed R.J., Bamidele L and Ajetumobi E.O. (2012). A preliminary radiation dose audit in some Nigeria hospitals: Need for determination of National Diagnostic Reference Levels (NDRLs). The Pacific Journal of Science and Technology. Vol 13 No1: 481 – 495. |



 , of each of the measured optical densities (D) was estimated from the relation:
, of each of the measured optical densities (D) was estimated from the relation: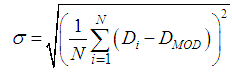
 : is the optical density of each radiographic film.
: is the optical density of each radiographic film. : is the Mean Optical Density (MOD) of the radiographic film.
: is the Mean Optical Density (MOD) of the radiographic film.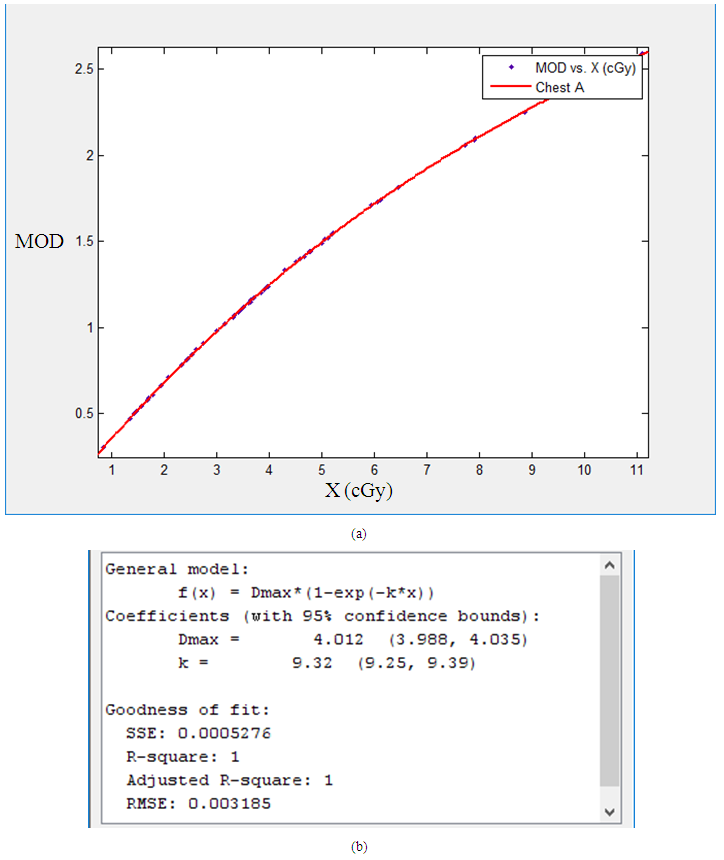
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML