-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Bioinformatics Research
p-ISSN: 2167-6992 e-ISSN: 2167-6976
2024; 13(1): 8-18
doi:10.5923/j.bioinformatics.20241301.02
Received: Aug. 21, 2024; Accepted: Sep. 20, 2024; Published: Oct. 15, 2024

Evaluation of Telehealth Implementation in Improving Healthcare Management
Faisal A. Lutfi1, Ahmad Subhi2
1Master of Health Administration Program, College of Health Professions, Central Michigan Universaity, Mt Pleasant, Michigan, USA
2Infection Disease Consultant, Al-Qassimi Hospital, Sharjah, UAE
Correspondence to: Ahmad Subhi, Infection Disease Consultant, Al-Qassimi Hospital, Sharjah, UAE.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The transition towards integrated telehealth and Artificial Intelligence (AI) in healthcare is not just a technological shift but a transformative change, especially significant in the context of infectious disease management. This study examines the competencies required for healthcare managers to lead effectively in this new era, emphasizing digital literacy, strategic adaptability, and proactive policy engagement. With infectious diseases posing continual challenges globally, telehealth offers a unique opportunity to enhance patient outcomes while mitigating the risks associated with in-person consultations. As healthcare evolves, the competencies of leaders must adapt to ensure that the benefits of telehealth and AI are fully realized in controlling infectious disease outbreaks.
Keywords: Telehealth, Healthcare Management, Public health, Healthcare adminstration
Cite this paper: Faisal A. Lutfi, Ahmad Subhi, Evaluation of Telehealth Implementation in Improving Healthcare Management, American Journal of Bioinformatics Research, Vol. 13 No. 1, 2024, pp. 8-18. doi: 10.5923/j.bioinformatics.20241301.02.
Article Outline
1. Introduction
- The adoption of telehealth technologies is becoming a transformative force in the healthcare sector, revolutionizing the way healthcare services are delivered and managed. This shift towards digital healthcare delivery methods, including video conferencing, remote monitoring, and mobile health applications, is not only expanding access to care but also introducing new challenges and opportunities in healthcare management. As telehealth continues to evolve, understanding its impact on healthcare management competencies becomes crucial. [1]This study aims to evaluate the effects of telehealth implementation on the development and enhancement of healthcare management competencies in a specific healthcare setting. By exploring the integration of telehealth and its correlation with managerial practices, this research seeks to uncover insights into how digital health technologies influence the competencies required for effective healthcare administration.
2. Problem Statement and Significance
- The rapid integration of telehealth services into healthcare systems presents both opportunities and challenges for healthcare management. While telehealth promises to improve access to care, reduce costs, and enhance patient satisfaction, its implications for healthcare management competencies remain underexplored. [2] Effective management plays a pivotal role in the successful implementation and sustainability of telehealth programs. Thus, assessing the impact of telehealth on healthcare management competencies is essential for ensuring healthcare leaders are equipped to navigate the complexities of digital healthcare delivery.This study is significant as it addresses the gap in literature regarding the relationship between telehealth implementation and healthcare management competencies, providing valuable insights for healthcare administrators, policymakers, and educators in the development of training and policy frameworks that support the effective use of telehealth technologies.
3. Study Objectives
- This research’s main objective is to evaluate the impact of telehealth implementation on healthcare management competencies within a specific healthcare setting. Specifically, the study aims to:1. Identify essential healthcare management competencies in the telehealth context.2. Evaluate the influence of telehealth service implementation on these competencies.3. Examine the implications of changes in competencies for healthcare administration and policy formulation.
4. Research Methodology
- An established research methodology will be used to systematically evaluate the impact of telehealth implementation on healthcare management competencies. This study will employ a program evaluation approach, incorporating a mix of qualitative and quantitative data sources. The methodology will encompass:Defining the Evaluation Purpose: Clarifying the study's aim to examine the relationship between telehealth implementation and the development or enhancement of healthcare management competencies.Describing Program Inputs Reviewing existing data on telehealth technologies and practices adopted in healthcare settings.Specifying Activities: Analyzing documented managerial activities influenced by telehealth, including data management, training, and coordination of services.Establishing Performance Criteria and Operational Indicators: Utilizing existing research to identify indicators for healthcare management competencies relevant to telehealth.Conducting Data Analysis: Leveraging secondary data analysis to assess the impact of telehealth on management competencies.Video Conferencing Telehealth is garnering substantial attention in the literature, with a focus on convenience and positive impact on various aspects of healthcare. In terms of convenience, telehealth is lauded for its potential to save time, reduce costs, and alleviate stress associated with travel and disruptions to employment. [16] Mixed experiences are reported, with positive feedback being more prevalent than negative for both telehealth and in-person consultations. Interviews reveal thematic alignments with 'patient ability' dimensions, emphasizing convenience, value perceptions, relationships, technology, and the importance of being seen. [16] Future interest in telehealth remains high, with 80% expressing interest in telephone consultations and 69% in video consultations. Qualitative data align with the notion that telehealth supports self-management, emphasizing relationships, convenience, technology fit, and the need for visibility. [16]Another dimension of telehealth explored in the literature revolves around video consultations. Evidence suggests video consultations are effectively utilized for diagnostics in various clinical fields such as dermatology, psychiatry, neurology, orthopedics, and pediatrics, with reasonably good diagnostic agreement observed compared to face-to-face consultations. [25] Positive outcomes are reported for patients treated via video consultations across different conditions and specialties, particularly in telehealth-assisted chronic disease management, where improvements are noted, especially in diabetes. [25] However, the literature highlights limited evidence of cost-effectiveness for video consultations, with the overall quality of studies described as poor-to-average. Some evidence does suggest cost-effectiveness for home care and specialist consultations by general practitioners with patients present. [25] Notwithstanding the cost considerations, patient satisfaction with video consultations is notably higher than face-to-face consultations. Patients reported benefits such as reduced waiting times, less need for travel, time savings, and overall convenience. [25]Moreover, the clinical perspective on telehealth, as assessed in a study involving clinicians, indicates a positive outlook. Clinicians judged telehealth as equivalent to or better than home visits in 71.6% of cases, and the overall experience of conducting telehealth sessions is rated positively in 90.3% of the sessions. [28] These findings underscore the potential of telehealth to not only match but surpass traditional in-person healthcare delivery in terms of effectiveness and overall experience, as perceived by clinicians. [28]Remote Monitoring The integration of technology within healthcare, particularly through health informatics, is catalyzing a paradigm shift in patient care, notably through remote monitoring systems. Health informatics, an interdisciplinary field that converges information systems, computer science, and healthcare using information and communication technologies (ICTs), serves the fundamental purpose of acquiring, storing, managing, retrieving, and utilizing biomedical information. [28] Remote monitoring systems, a key facet of health informatics, is revolutionizing patient care by enabling the real-time collection, dissemination, and analysis of medical data from remote locations, particularly for managing chronic conditions and detecting health emergencies. [7] This advancement is bolstered by the integration of smart wearable mobile devices and cloud computing within public healthcare systems, which aim to better manage patient populations, especially those residing in remote areas far from healthcare service providers. [7]Moreover, within specialized domains such as Artificial Pancreas (AP) systems, remote monitoring plays a pivotal role in optimizing patient outcomes. Reliable measures of psychosocial impact are deemed crucial for regulatory approval processes and reimbursement decisions for AP systems, ensuring robust consideration of psychosocial factors during regulatory approval and reimbursement determinations by government and private payers. [20] By maximizing benefits for individuals with diabetes in terms of glycemic control and quality of life while minimizing the overall burden of diabetes in everyday life, remote monitoring through AP systems underscores the transformative potential of technology in healthcare. [20]In parallel, telehealth, another manifestation of remote monitoring, underscores the significance of patient-provider communication in enhancing satisfaction levels. Positive communication experiences facilitated by telehealth enable patients to feel heard, have their concerns addressed, participate in decision-making, and maintain confidentiality, thereby contributing to overall patient satisfaction. [23] However, challenges such as the absence of physical examinations and preferences for local healthcare provider presence persist among some patients, highlighting the ongoing need for refinement and adaptation of remote monitoring technologies to meet diverse patient needs. [23] Overall, remote monitoring systems, encompassing various technological advancements and applications such as telehealth and AP systems, hold immense promise in optimizing patient care, enhancing healthcare accessibility, and improving health outcomes across diverse patient populations.Telemedicine Applications The landscape of telehealth is experiencing a significant upsurge in interest and utilization, largely propelled by the anticipated implementation of the Affordable Care Act and the continual advancements across various telehealth services. These services, ranging from gap coverage to urgent care provisions and the facilitation of video-enabled multisite group chart rounds, reflect the dynamic and evolving nature of telehealth in meeting the diverse healthcare needs of patients and providers alike. [21] Within this landscape, critical success factors are emerging, underscoring the importance of establishing a well-defined business plan with sustainable revenue streams. Notably, programs offering gap service coverage, such as teleradiology, are demonstrating a higher likelihood of success, suggesting the significance of strategic service offerings in telemedicine initiatives. [21] However, despite the evident advantages, barriers to telemedicine success persist, particularly in the realm of reimbursement challenges that necessitate governmental or regulatory intervention. Issues such as disparities between Medicare and Medicaid reimbursement rates in certain states and complexities surrounding interstate medical licensure rules continue to pose significant hurdles to widespread telemedicine adoption. [21]Furthermore, the advent of mobile health (mHealth) represents a disruptive force within the healthcare landscape, marked by its rapid growth and transformative potential driven by the ubiquitous presence of smartphones. Leveraging networking systems, application software, and advanced devices, mHealth applications offer diverse functionalities for remote healthcare delivery, including user-friendly design, enhanced accessibility, and adaptability to varying user needs and preferences. [11] These applications not only facilitate healthcare accessibility and affordability through features like video medical appointments and electronic prescription delivery but also serve as valuable tools for linking clinicians with patients, fostering long-term engagement and supporting lifestyle changes conducive to improved health outcomes. [11] Moreover, by eliminating distance limitations and facilitating electronic communication between doctors and patients, mHealth applications hold promise for expanding healthcare access and bridging gaps in healthcare delivery, particularly in underserved or remote areas. Through enhanced information exchange and collaboration, these technologies can elevate the quality of healthcare facilities and services across geographically disparate regions. [11]Additionally, the transition from traditional paper-based medical records to electronic health records (eHR) facilitated by telemedicine applications represents a significant advancement in healthcare information management. This transition empowers healthcare providers with access to comprehensive and up-to-date medical information, thereby enhancing their ability to make well-informed management decisions and deliver personalized care to patients. [8] Furthermore, the proliferation of health apps and wearable devices is revolutionizing health monitoring and management, enabling individuals to track various health parameters, manage chronic conditions, and adhere to treatment regimens with greater ease and precision. The integration of these technologies allows for seamless data synchronization and analysis, providing clinicians and patients alike with valuable insights into health trends and facilitating informed decision-making. [8] Collectively, these developments underscore the transformative potential of telehealth and mHealth in revolutionizing healthcare delivery, improving patient outcomes, and advancing the quality and accessibility of healthcare services.Remote Health EducationThe integration of telemedicine into medical education is emerging as a promising avenue for enhancing clinical training and educational engagement among medical students. Remote clinical roles utilizing telemedicine platforms offer teaching hospitals an innovative means to involve medical students in outpatient care, enabling them to participate in various clinical activities such as patient history-taking, education delivery, and documentation of visits. This approach not only provides students with early exposure to clinical practice but also facilitates the development of communication skills essential for effective patient interaction. [32]Additionally, collaborative learning initiatives, including partnerships with other medical institutions for shared online education activities, and online mentoring programs, which utilize telecommunication for mentorship and portfolio updates, are shown to enhance educational engagement and facilitate mutual learning opportunities. [18]Moreover, leveraging online platforms for organizing competitions in arts and humanities and providing uninterrupted access to digital library resources contribute to fostering positive attributes and meaningful learning experiences among medical students. [32] Considering the COVID-19 crisis, leveraging online platforms to encourage student reflection, narrative writing, and proposal of innovative ideas for combating the pandemic is emerging as a valuable educational approach. Such strategies not only promote active learning but also foster resilience and adaptability in the face of disruptive circumstances. [32]Overall, indicators for effective online engagement encompass observational and application-based learning behaviors, with strategies aimed at incentivizing teacher-learner participation and ensuring continuous involvement in the learning process. By adopting these approaches, medical educators can effectively navigate the challenges posed by the COVID-19 pandemic while fostering meaningful learning experiences and enhancing educational outcomes among medical students. [32]Store and Forward TechnologyStore-and-forward telemedicine is emerging as a vital component in providing medical care in resource-limited settings, especially in specialties reliant on image-based diagnostics, although there is a notable scarcity of quality measurement reports within this field. [31] In response to this need, Médecins Sans Frontières (MSF) took the initiative in 2010 to establish a store-and-forward telemedicine network, which is managing over 1000 cases spanning 40 countries, demonstrating its potential to bridge healthcare gaps across diverse geographic regions. [31] A proposed method for assessing the quality of telemedicine services involves a panel of observers evaluating process and outcome quality through a questionnaire administered on a randomly chosen past case, with feasibility successfully demonstrated over a 9-month trial period. [31]Furthermore, the utility of store-and-forward telemedicine extends beyond resource-limited settings, with its significance highlighted in extreme environments such as Antarctica, where geographical isolation poses unique challenges to accessing specialized medical care. [32] In a study conducted in this remote region, telemedicine via email proved to be a crucial tool for obtaining specialist advice, particularly in cases where physical access to healthcare professionals is impractical. The study revealed that a store-and-forward telemedicine system, when employed by NGOs with trained specialist teams and automatic message-handling systems, was efficient and reliable in providing well-argued and adapted advice tailored to the specific needs of patients in remote areas. However, limitations used to identify in other methods, such as contacting personal acquaintances, underscores the importance of structured telemedicine systems in ensuring effective healthcare delivery. [32]Moreover, the integration of telemedicine into mainstream medical practice is yielding significant benefits, as evidenced by combined user feedback and patient follow-up data indicating high response rates and the perceived usefulness of teleconsultation advice for both referring doctors and patients. [31] Over 90% of referrers found teleconsultation advice to be educationally beneficial, underscoring its positive impact on medical practitioners' knowledge and decision-making processes. [31]Additionally, teleconsultations led to cost savings in approximately 20% of cases, reflecting the financial advantages of store-and-forward telemedicine applications for patients, families, and healthcare institutions. [31]In summary, the evolution and widespread adoption of store-and-forward telemedicine holds promise for improving healthcare accessibility, quality, and cost-effectiveness across diverse healthcare settings.Digital Health Platforms Digital Health Platforms (DHPs) are garnering widespread acceptance and satisfaction among users, with studies indicating a positive attitude toward their adoption and usage. Users often express elevated levels of satisfaction, with rates reaching 9 out of 10, citing the speed and accessibility of digital healthcare as key factors contributing to their positive perceptions. Compared to traditional healthcare settings, DHPs offer users the convenience of avoiding queues and the flexibility to manage recurring healthcare needs efficiently. However, there remain challenges in ensuring widespread adoption, particularly among elderly users. To address this, managerial implications for DHP developers include focusing on streamlining adoption processes, enhancing platform intuitiveness for elderly users, conducting test panels with elderly demographics, and implementing tailored information campaigns to boost awareness and address any negative attitudes. [10]Considering the Covid-19 pandemic, the importance of health informatics tools is underscored, particularly in mitigating pressure on healthcare systems and enhancing accessibility for consumers. Various health IT solutions are developed globally, with a specific focus on initiatives in Saudi Arabia. Facilitating conditions and trust emerge as crucial factors influencing consumers' intention to use digital healthcare platforms. Integrated tools and solutions that address trust and privacy concerns are highlighted as essential for fostering user acceptance and utilization of digital healthcare services, especially in regions like Saudi Arabia. [4]First-generation digital health applications are demonstrating substantial efficacy across diverse medical conditions, ranging from the detection of atrial fibrillation and epilepsy seizures to enhancing cancer diagnosis and predicting outcomes of gastrointestinal bleeding. These applications are revolutionizing healthcare delivery by enabling early identification and intervention, thereby improving patient outcomes and quality of life. Moreover, they play a critical role in disease prediction, management, and personalized treatment approaches, significantly impacting healthcare decision-making and patient empowerment. Additionally, the integration of digital health tools for self-monitoring of blood glucose exemplifies the democratization of medicine, providing individuals with enhanced control over their health outcomes and reducing the burden of diabetes-related complications. [15]Tele stroke Services The landscape of public healthcare is undergoing a profound transformation in the 21st century, driven by technological advancements that are reshaping the way medical services, particularly stroke care, are delivered. Among these innovations, tele stroke networks are emerging as a cornerstone, revolutionizing access to acute stroke therapies irrespective of geographical barriers. These networks leverage telecommunication technologies to enable remote consultations between stroke specialists and healthcare providers in underserved areas, facilitating timely diagnosis and treatment decisions. The outcomes of tele stroke interventions are demonstrating remarkable diversity, yet they consistently yield reproducible results, underscoring the efficacy and reliability of this approach. Moreover, the financial sustainability of tele stroke initiatives further bolsters their significance in enhancing acute stroke care delivery. However, as telemedicine continues to evolve and expand its scope beyond acute stroke management, the establishment of robust infrastructure, comprehensive policies, standardized protocols, and sustainable financial reimbursement models becomes imperative to ensure the continued success and scalability of tele stroke networks. [6]Despite the promising potential of tele stroke in transforming acute stroke care, several challenges persist, necessitating further research and development efforts. Rigorously designed studies are urgently needed to validate the accuracy, reliability, and clinical utility of telemedicine in stroke management. This imperative is underscored by the urgent need for evidence-based practices to guide the integration of tele stroke into routine clinical workflows effectively.Additionally, recent legislative changes, such as the approval of reimbursement for telemedicine consultations in rural Health Personnel Shortage Areas, signal a growing recognition of tele stroke's value in addressing disparities in access to acute stroke care. By harnessing the power of telemedicine, healthcare providers can leverage innovative technologies to overcome geographical barriers, enhance diagnostic accuracy, and optimize treatment outcomes for stroke patients. Thus, while tele stroke holds great promise for advancing acute stroke care, ongoing research, collaboration, and policy support are essential to unlock its full potential and ensure equitable access to high-quality stroke care for all individuals. [19]Tele mental Health Services Tele mental health is emerging as a significant area of growth within the healthcare sector, with estimations indicating that up to 50% of all healthcare services will be conducted electronically by 2020. [3] Despite this rapid expansion, scientific research in the field is struggling to keep pace, which is hindering the ability to provide robust recommendations, particularly regarding the substitution of online platforms for traditional care methods. However, existing literature on tele mental health underscores its potential in diagnosing and managing various psychiatric conditions. Notable advantages include increased access to care, improved efficiency, reduced stigma associated with visiting mental health clinics, and the ability to overcome diagnosis-specific treatment obstacles. Specifically, computerized cognitive-behavioral therapy (cCBT) and Internet-based cognitive-behavioral therapy (iCBT) demonstrate efficacy, while emerging options such as virtual reality exposure therapy (VRET) and mobile therapy (mTherapy) show promise. [3]Nonetheless, challenges such as the requirement for specific computer skills, concerns about therapeutic alliance, and patient attrition remain significant considerations for the widespread implementation of tele mental health services. Further research is needed to explore the efficacy, advantages, and limitations of technology-enabled interventions and to expand the scope of online psychotherapeutic and psychopharmacological modalities. [3]The transition from in-person to telehealth services during the COVID-19 pandemic demonstrated notable positive outcomes in mental health care delivery. Increased attendance rates are observed, attributed to the flexibility, and reduced logistical barriers associated with telehealth. [17]Additionally, fewer canceled appointments and unchanged no-show appointments indicate improved appointment adherence, effectively addressing logistical challenges. Participants undergoing the transition to telehealth are reporting a decrease in symptom severity and improvement in mental health symptoms, underscoring the potential of telehealth to yield positive outcomes. [17] Despite its limitations, telehealth emerges as a promising option for providing integrated mental health services, particularly benefiting low-income individuals, racial/ethnic minorities, adults, and children. Furthermore, there is optimism regarding the continued effectiveness of telehealth beyond pandemic conditions. These findings highlight the transformative potential of telehealth in mental health care delivery and emphasize the importance of further research and integration of telehealth services to ensure equitable access and enhanced outcomes for all individuals. [17]
5. Research Methodology - Program Evaluation Approach
- IntroductionThis chapter presents the research methodology adopted to investigate the impact of telehealth implementation on healthcare management competencies in a specific healthcare setting. Given the expanding role of telehealth in healthcare delivery, it is imperative to understand its influence on management practices and competencies. This study employs a program evaluation approach to systematically assess how telehealth initiatives contribute to the development and enhancement of healthcare management competencies, crucial for effective healthcare administration.Program Evaluation as Research MethodologyProgram evaluation is a systematic method for collecting, analyzing, and using information to answer questions about projects, policies, and programs, particularly about their effectiveness and efficiency. In the context of this study, the program evaluation approach is applied to examine the telehealth implementation process, its activities, outputs, and outcomes related to healthcare management competencies. This method enables the identification of key competencies affected by telehealth and the assessment of these changes' implications for healthcare administration.Defining the Evaluation PurposeThis evaluation’s main purpose is to determine the impact of telehealth implementation on healthcare management competencies within a specific healthcare setting. This involves exploring how telehealth has influenced the skills, knowledge, and abilities required by healthcare managers to effectively lead and manage healthcare services in a digitally evolving environment.Describing Program InputsProgram inputs refer to the resources, technologies, and processes deployed for telehealth implementation. This includes an examination of the telehealth technologies adopted, the training provided to staff, the infrastructural changes made, and the policies developed to support telehealth services. Understanding these inputs is crucial for assessing their contribution to enhancing healthcare management competencies.Specifying ActivitiesThis segment outlines the activities involved in the telehealth implementation process, such as the development and delivery of telehealth services, the management of telehealth platforms, and the integration of telehealth into existing healthcare workflows. Detailing these activities allows for a clearer understanding of the managerial tasks and challenges associated with telehealth and how they influence management competencies.Establishing Performance Criteria and Operational IndicatorsTo evaluate the impact of telehealth on healthcare management competencies, specific performance criteria and operational indicators will be established. These criteria may include measures of efficiency, effectiveness, quality of care, and satisfaction levels among staff and patients. Operational indicators will be defined based on the competencies of interest, such as leadership in digital transformation, strategic decision-making in telehealth deployment, and innovation in healthcare delivery models.Conducting Data AnalysisData analysis will involve the systematic examination of data collected through various sources, including internal reports, staff surveys, patient feedback, and performance metrics. The analysis will focus on identifying trends, patterns, and correlations between telehealth implementation and changes in healthcare management competencies. Qualitative data will be analyzed for thematic content related to management practices, while quantitative data will be assessed using statistical methods to evaluate the effectiveness and efficiency of telehealth services.ConclusionsBy employing a program evaluation approach, this study aims to provide a comprehensive understanding of the impact of telehealth on healthcare management competencies. This methodology facilitates a structured assessment of telehealth initiatives, from inputs and activities to outcomes, enabling a thorough evaluation of their effectiveness in enhancing management practices within healthcare settings. The findings from this evaluation will offer valuable insights for healthcare administrators, policymakers, and educators, informing strategies to optimize telehealth implementation and its contribution to healthcare management excellence.
6. Data Analysis
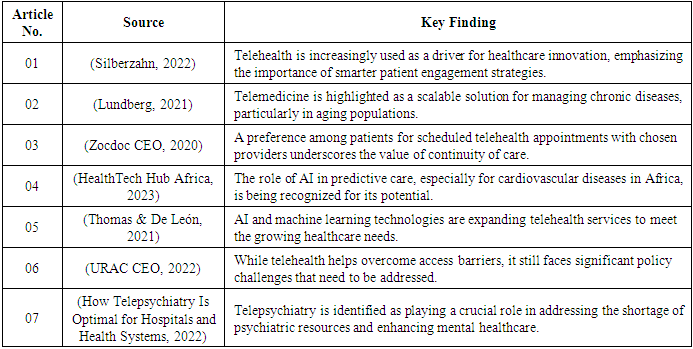
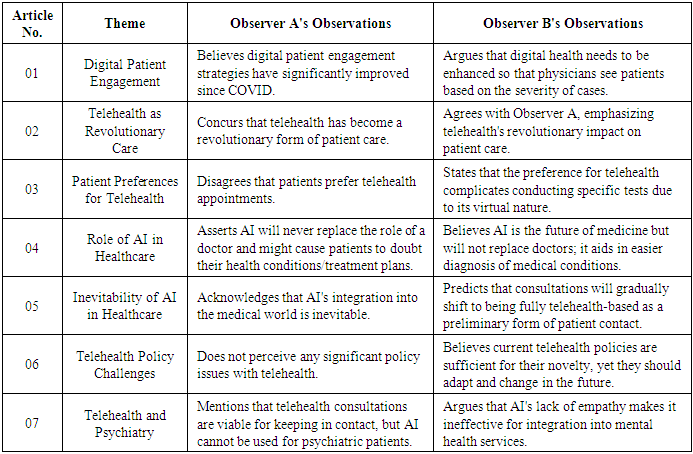
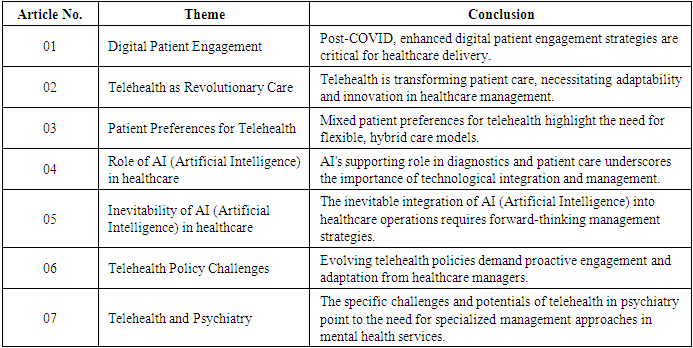
- IntroductionThis chapter focuses on presenting the data extracted from selected sources as outlined. By analyzing articles from influential thought leaders and industry experts, this chapter aims to elucidate the current state of telehealth and its implications for healthcare management competencies.Data PresentationFollowing the methodological approach from, the data extracted from the articles were synthesized into a table, providing a clear view of the key findings relevant to the research problem.
|
|
|
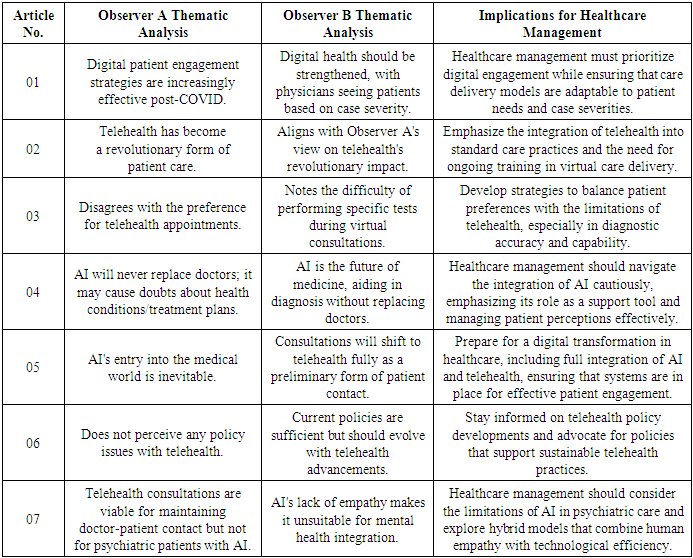
7. Summary
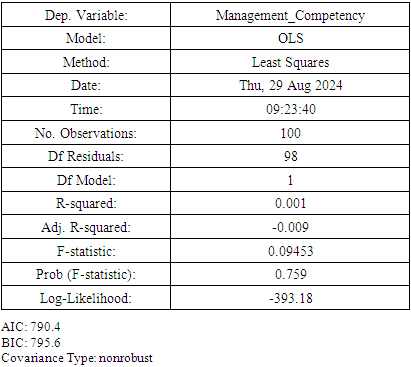
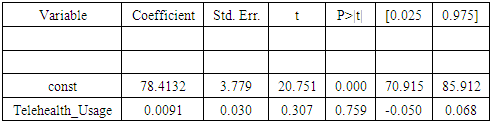
- IntroductionBuilding upon the comprehensive data analysis conducted beofre, this chapter seeks to interpret the findings within the broader landscape of healthcare management. It is timely to revisit the research problem and reemphasize the need for this research. Explore the impact of telehealth and AI (Artificial Intelligence) on healthcare management competencies—and the objectives initially set out to achieve a deeper understanding of the implications these technological advancements have for the field.Data InterpretationThe integration of telehealth and AI into healthcare delivery was accelerated by recent global events, notably the COVID-19 pandemic. This acceleration not only transformed patient care but has also necessitated a reevaluation of healthcare management competencies. From the data, it is evident digital patient engagement and the use of AI in healthcare are no longer futuristic ideals but current realities that require immediate attention and adaptation by healthcare managers.Observations from the thematic analysis suggest a pivotal shift in healthcare delivery models. Telehealth, once considered a supplementary form of patient care, has emerged as a revolutionary approach, fundamentally altering the patient-provider interaction landscape. This shift underscores the necessity for healthcare managers to possess a robust understanding of digital health technologies and to develop strategies that effectively integrate these technologies into patient care.Moreover, the analysis highlights a growing consensus on the importance of AI in enhancing diagnostic processes and personalizing patient care. However, it also brings to light concerns regarding the implementation of AI, including ethical considerations, patient trust, and the potential for AI to supplement rather than replace human medical practitioners.The insights gathered from Observers A and B further enrich our understanding of these themes, presenting a spectrum of perspectives on the role and implications of telehealth and AI in healthcare. While there is enthusiasm for the potential of these technologies to improve healthcare delivery, there is also caution regarding their integration and the ongoing need for human touch and judgment in healthcare.In synthesizing these observations, it becomes clear healthcare management is at a crossroads. The field must navigate the challenges and opportunities presented by telehealth and AI, balancing technological innovation with the intrinsic human elements of healthcare.Regression OutputA linear regression analysis was conducted to examine the relationship between the number of telehealth sessions and healthcare management competency scores. The dataset consisted of 100 hypothetical observations.
|
 Additional Tests
Additional Tests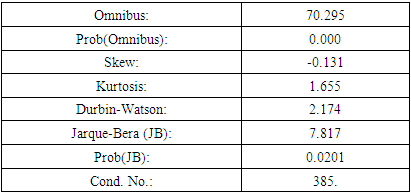
8. Conclusions
- The analysis leads to several key conclusions regarding the integration of telehealth and AI in healthcare settings and its implications for healthcare management.
|
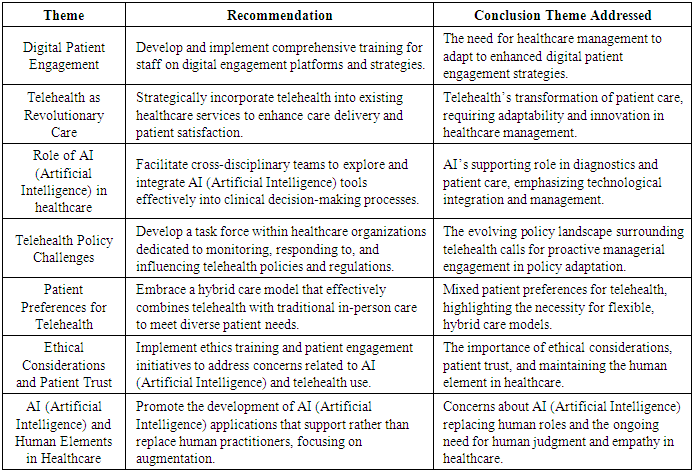
9. Recommendations Based on Conclusions
- In response to these conclusions, a series of recommendations are suggested to support healthcare managers in navigating the changing dynamics of healthcare delivery.
|
10. Limitations
- This study's limitations stem from its reliance on selected articles for thematic analysis, potentially introducing bias in the interpretation of themes. Furthermore, the perspectives of Observers A and B may not fully capture the diversity of opinions within the field. The rapidly evolving nature of telehealth and AI technologies also means the findings may quickly become outdated as new advancements and policies emerge.
11. Discussion – Summary
- The central problem this study aims to address is the need for healthcare management to evolve in response to the rapid integration of telehealth and AI technologies in healthcare delivery. The goals were to identify the competencies required for effective healthcare administration in this new digital era and to understand the broader implications for healthcare management practices. The identified study problem and supporting goals were successfully addressed, lending further clarity, understanding, insights, and potential management directions. The findings highlight a clear shift toward more digitally focused healthcare management practices, underscoring the importance of technological competencies, adaptability to policy changes, and the integration of AI and telehealth into patient care strategies. These discoveries reflect a broader trend in healthcare towards more personalized, efficient, and accessible care delivery models, driven by technological innovation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML