-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Applied Mathematics
p-ISSN: 2163-1409 e-ISSN: 2163-1425
2017; 7(1): 1-4
doi:10.5923/j.am.20170701.01

Mathematical Modeling of Coronary Artery Disease (CAD): Analysis Reveals HbA1c and Total Cholesterol to be Significant Risk Predictors
Padma Murali1, P. R. Deepa2, Raghavan Subramanyan3, Farida Farzana A. J.3, Nithya Lakshmi M.3, Murali Raman4
1Dept. of Mathematics, Birla Institute of Technology & Science (BITS), Pilani, India
2Dept. of Biological Sciences, Birla Institute of Technology & Science (BITS), Pilani, India
3Dept. of Cardiology, Frontier Lifeline Hospital & Dr. KM Cherian Heart Foundation, Chennai, India
4Pharmaceutical Consultant, Chennai, India
Correspondence to: Padma Murali, Dept. of Mathematics, Birla Institute of Technology & Science (BITS), Pilani, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The increasing prevalence of CAD (Coronary Artery Disease) calls for early detection of risk factors and effective clinical management. The predictive potential of commonly estimated clinical variables on CAD incidence was assessed using mathematical modeling and analysis. A random sample of 50 patients with CAD and a control group of 50 subjects without CAD were drawn from a cardiac specialty hospital in Chennai, India during 2011-2012 (mean age = 50.2 years, SD = 11.2 years). Medical data included age, gender, height, weight, body mass index, presence/absence of hypertension, systolic blood pressure, diastolic blood pressure, presence/absence of diabetes mellitus, fasting blood sugar, post-prandial blood sugar, HbA1c, total cholesterol, family history of CAD. Mathematical modeling using discriminant analysis was performed to understand significant contributors leading to CAD. The discriminant analysis resulted in a mathematical model using parameters, HbA1c and cholesterol. The model was found to be statistically significant and this was demonstrated by computing the F value. HbA1c and total cholesterol were found to be significant in predicting the occurrence of CAD.
Keywords: Mathematical Modeling, CAD, HbA1c, Cholesterol, Hypertension, Risk Factors, Discriminant Analysis
Cite this paper: Padma Murali, P. R. Deepa, Raghavan Subramanyan, Farida Farzana A. J., Nithya Lakshmi M., Murali Raman, Mathematical Modeling of Coronary Artery Disease (CAD): Analysis Reveals HbA1c and Total Cholesterol to be Significant Risk Predictors, Applied Mathematics, Vol. 7 No. 1, 2017, pp. 1-4. doi: 10.5923/j.am.20170701.01.
Article Outline
1. Introduction
- In the emerging healthcare scenario in developing countries, urbanized lifestyle changes are resulting in increased prevalence of cardiovascular risk factors (diabetes, obesity, hypertension, and hypercholesterolemia). These in turn result in cardiovascular diseases (CVD) that include coronary heart disease and stroke [1]. Ferrari et al [2] found that the prevalence of some of the important CVD risk factors in CAD varied quite significantly across the seven geographical zones (Western / Central Europe; Canada / South Africa / Australia / UK; Eastern Europe; Central / South America; Middle East; East Asia; and India) categorized in a 5-year observational longitudinal cohort study – CLARIFY. Important observations on this varied prevalence were: (i) obesity ranged from 20% (East Asia) to 42% (Middle East), (ii) hypertension from 28% (Central/South America and East Asia) to 48% (Eastern Europe), (iii) increased LDL cholesterol levels from 24% (Canada/South Africa/ Australia/UK) to 65% (Eastern Europe), (iv) increased heart rate (≥70 bpm) from 38% (Western/Central Europe) to 78% (India), (v) diabetes from 17% (Eastern Europe) to 60% (Middle East), and (vi) smoking from 6% (Central/South America) to 19% (Eastern Europe). It is well recognized that diabetes with other co-morbidities places the patient at potential risk of developing CVD. Still, there is greater need to step-up medical management of co-morbidities - hypertension and hyperlipidemia in patients with type 2 diabetes [3]. Avogaro et al., [4] reported that hyperglycemia and hypertension (particularly in men), and diabetic dyslipidemia (particularly in women), are risk factors of coronary heart disease (CHD) that can be modified with aggressive medical treatment. These risk characteristics point to vital implications in clinical management, wherein effective controls of glycemia, hypertension, and hyperlipidemia have been suggested to prevent CHD in diabetic patients. Diabetes induces a higher CHD risk in women, and higher ischemic stroke risk in men [5].Interestingly, the link between glucose levels and cardiovascular disease/risk is not limited to diabetic patients. In fact, it is reported that non-diabetic individuals with higher baseline blood glucose levels (after adjustment for covariant) may carry a significantly high risk for developing CAD [6]. Kim et al [7] recently reported that when the mean HbA1c levels were above 6.2%, the CAD risk was higher and that HbA1c level can be one of the predictors for CAD even in the absence of diabetes.In the present study, we have used discriminant analysis to model and determine the biochemical variables that show close correlations in the development of CAD. Clinical values of common risk parameters such as glycosylated hemoglobin, glucose, cholesterol, blood pressure, body mass index and body weight were used to develop the model.
2. Study Design and Methodology
- Medical data of 50 patients with CAD and a control group of 50 people without CAD were collected from a cardiac specialty hospital in Chennai, India between October 2011 and June 2012. The average age of the cohort was 50.2 years with a standard deviation of 11.2 years. The study cohort characteristics were as follows: Group I : Patients with abnormal values of risk factors with Coronary Artery Disease (Male: Female ratio was 44: 24, average age was 53.4 ± 9.77 years (age range: 32- 78 years); Group II : Subjects with controlled risk factors/ no risk factors without Coronary Artery Disease (Male: Female ratio was 39: 14, average age was 46.04 ± 11.54 years (age range: 21- 75 years). The study was approved by the Institutional Ethics Committee of Frontier Lifeline Hospital. CAD means patients with acute coronary syndrome (ACS) and / or positive Treadmill test (TMT) and / or angiographically proven CAD. Without CAD means patients with negative TMT or normal coronaries by angiogram (< 6 months ago).The inclusion criteria included all patients who were diagnosed with CAD during the last six months. Patients with symptoms of chest pain with or without risk factors but not proved either by ACS or TMT or Coronary Angiogram were excluded from the study. Further, patients who have been diagnosed with CAD over a period greater than six months were excluded from the study as this group would have been on medication for significant period of time which would have resulted in impacting the medical parameters.The risk factors taken into consideration for the study were weight, body mass index, presence/absence of hypertension, systolic blood pressure, diastolic blood pressure, presence/absence of diabetes mellitus, fasting blood sugar, post prandial blood sugar, HbA1c, total cholesterol, and family history of CAD. Fasting total cholesterol > 200mg/dl was considered abnormal. A patient was considered as uncontrolled diabetic if the fasting blood glucose > = 126 mg/dl or if the two hour (post-prandial) blood glucose level was > =200 mg/dl, or if the HbA1c (Glycosylated Hb) was 6.5% or above. Family history of premature CAD in first degree relatives was defined as IHD or sudden cardiac death before 55 years of age (in men) or 65 years of age (in women). BMI (Body mass index)> 30 was considered as obese. A patient was considered as hypertensive if the systolic blood pressure was 140 mm Hg and above or the diastolic blood pressure was 90 mmHg or higher [8].Discriminant analysis was performed with all risk parameters. Each iteration resulted in the removal of the least significant variable. The statistical significance of the model was determined using the F values. The observed F value was compared with the tabulated F value and the statistical significance of the model was arrived at [9, 10].
3. Mathematical Modeling and Discussion
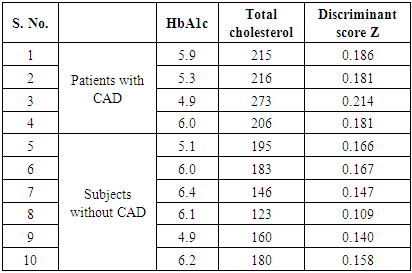
- In a review of CHD and its risk burden in India, [11] pointed out that the measures should be implemented to screen for common risk factors such as high blood pressure, dyslipidemia, diabetes, and to provide for their mitigation in a cost-effective manner, in order to lessen the CHD deaths. Suitable lifestyle changes (including physical activity) and nutritious diet (balanced intake of fruits and vegetables) would complement these preventive steps in the control of CHD burden. Our previous mathematical model and analysis of CVD burden in diabetic population, clearly indicated the effective control of associated co-morbidities (hypertension and hyperlipidemia) substantially reduced the incidence of CVD [12]. In the present study, the routinely assessed clinical/biochemical parameters of each patient/ subject were analysed and correlated with the presence/absence of CAD. The modeling was carried out with a set of 50 patients and a set of 50 subjects without CAD as control. Step wise discriminant analysis led to equations (1) and (2).
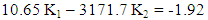 | (1) |
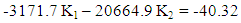 | (2) |
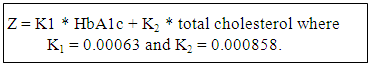 The discriminant criteria value Z was computed for each person from the control group and for each patient with CAD which is presented in figure 1.
The discriminant criteria value Z was computed for each person from the control group and for each patient with CAD which is presented in figure 1.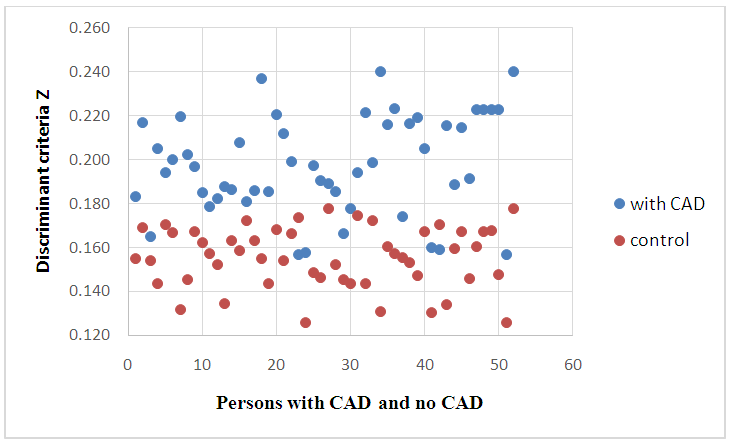 | Figure 1. Discriminant criteria using parameters HBA1C and total cholesterol |
|
4. Conclusions
- The results of our study indicate mathematical modeling using discriminant analysis serves to predict presence/absence of CAD. Here, CAD was found to be a function of total cholesterol and HbA1c. The model was successfully validated using a sample set of cases. This model can be used to predict presence of CAD and can be a useful tool for physicians.
ACKNOWLEDGMENTS
- The presented work was funded by a research grant from the University Grants Commission (UGC), New Delhi, India.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML