-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Polymer Science
p-ISSN: 2163-1344 e-ISSN: 2163-1352
2023; 12(1): 17-21
doi:10.5923/j.ajps.20231201.03
Received: Jun. 6, 2023; Accepted: Jun. 26, 2023; Published: Jul. 8, 2023

Findings of Air Quality Monitoring in Special Hospital Indoors to Detect SARS-COV-2 Virus (COVID-19)
B. K. Nurmatov, B. B. Rakhimov., G. Sh. Tashmetova
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Indoor air quality are the important factors influencing the infectious diseases such as SARS-COV-2 virus. This study is aimed to explore the associations between air quality and spreading of COVID-19 virus indoor condition. The study was conducted from February 20 to March 3, 2020, at the Zangiota-2 in-patient unit specializing in the treatment of COVID-19 patients. 100 air samples were taken in Hospital from various departments. And also, indoor air quality parameters (microclimate factors, amount of fine dust particles, carbon monoxide (II) concentration, and amount of formaldehyde) were studied simultaneously with sampling. Two out of 100 air samples taken at different locations in hospital wards tested positive for the presence of SARS-CoV-2. In conclusion, hospital room air and its quality can be a potential source of SARS-CoV-2 infection.
Keywords: Indoor air quality, SARS-COV-2 virus, Spreading of COVID-19
Cite this paper: B. K. Nurmatov, B. B. Rakhimov., G. Sh. Tashmetova, Findings of Air Quality Monitoring in Special Hospital Indoors to Detect SARS-COV-2 Virus (COVID-19), American Journal of Polymer Science, Vol. 12 No. 1, 2023, pp. 17-21. doi: 10.5923/j.ajps.20231201.03.
1. Introduction
- On December 31, 2019, a new type of coronavirus causing severe pneumonia with acute respiratory syndrome was discovered in Wuhan of China, and quickly spread worldwide. The World Health Organization had declared a pandemic. As of May 7, 2020, it was reported that 3.5 million people worldwide had been infected and about 250,000 people had died from the disease (WHO, 2020a; WHO, 2020b; Noorimotlagh, 2021). The first case of infection in our country was detected on March 15, 2020, in a woman who had been arrived from France; the laboratory examination confirmed COVID-19 disease.High level of COVID-19 spread in the world required serious research to determine clinical characteristics of the new coronavirus infection, its complications and possible ways of its transmission, including airborne. According to previous studies and WHO guidelines, the main route of transmission of the new coronavirus disease is human-to-human transmission (prolonged and unprotected exposure), and there is much discussion about other routes of transmission, such as airborne transmission (Guan et al, 2020; Van Doremalen et al., 2020; Sohrabi et al., 2020; WHO, 2020b; Holshue et al., 2020; Ghinai et al., 2020; Morawska and Cao, 2020; Noorimotlagh et al., 2020). The transmission and epidemiology of the two zoonotic coronaviruses, Middle East respiratory syndrome (MERS-CoV) and SARS-CoV-1, are known to science, and airborne transmission has played an important role in their spread.In view of the limited and unevidenced-based data on airborne transmission of SARS-CoV-2, researchers are encouraged to conduct additional research in this area. Detection of airborne transmission of SARS-CoV-2 is one of the most important debates among researchers to better understand and manage the SARS-CoV-2 pandemic and to protect the health of both medical professionals and the public. Therefore, we sought to investigate air quality indicators within hospital rooms treating patients with confirmed COVID-19 disease to determine the potential spread of SARS-CoV-2 in the hospital.
2. Material and Methods
- The study was conducted from February 20 to March 3, 2020, at the Zangiota-2 in-patient unit specializing in the treatment of COVID-19 patients. Air samples were taken from the intensive care unit, treatment room, doctor’s office and waiting room. In this research It was used an imager containing DMEM (Dulbecco’s Modified Eagle’s Medium) nutrient medium, which traps airborne microorganisms. A high-efficiency indoor air sampling pump (Gil Air Plus Personal air sampler) was used to collect and transfer air samples to the special nutrient medium. Air samples were taken at a distance of 1.5 m from the patient’s bed at a height of 1.5 m above the ground for one hour at a flow rate of 4 l/min-1. Pump calibration was performed twice, before and after analysis, using a Gilibrator 2 Wet Cell Calibrator. Samples were transported to the laboratory for real-time reverse transcription polymerase chain reaction (RT-PCR) in a special thermostable bag. In addition, indoor air quality parameters (microclimate factors, amount of dust particles, carbon (II) oxide concentration, and amount of formaldehyde) were studied simultaneously with sampling.The samples were immediately transported to the laboratory of the same hospital for SARS-CoV-2 RNA analysis by real-time reverse transcription-polymerase chain reaction (RT-PCR). The analysis was performed using the SARS-CoV-2 nucleic acid detection kit according to the manufacturer’s instructions (Bio-Rad, Feldkirchen, Germany). All samples were analyzed according to WHO recommendations.Statistical analysis: Statistical analysis was performed using SPSS software version 26.0 (SPSS Inc.). The interquartile range distribution was completed in descriptive statistics.
3. Result and Discussion
- The virus (COVID-19) appeared suddenly, spread rapidly in all developed and developing countries and caused a worldwide pandemic. In this study, we investigated the quality of viral air in the hospital to determine the possibility of airborne transmission of SARS-CoV-2. In this regard, Table 1 provides specific information about the condition of the indoor environment of hospital rooms and the concentration of particles of different aerodynamic diameters, chemical substances (CO2, HCHO), microclimate (temperature, relative humidity, and air speed) during bioaerosol sampling. Tables 2 and 3 show the characteristics of air samples (bioaerosols) for the detection of SARS-CoV-2 in hospital room air. As shown in Table 1, there were 62 patients with confirmed COVID-19, ranging from severe and acutely severe to mild. Two out of 100 air samples taken at different locations in hospital wards tested positive for the presence of SARS-CoV-2. Our results contradict those of Faridi et al (2020) in a hospital complex in Tehran, where no positive samples were found among the air samples. Furthermore, Ong et al (2020) reported that airborne transmission of SARS-CoV-2 is not a pandemic causative agent. Moreover, in contrast to the above, Iranian scientists Azra Kenarkuhi et al. (2020) in a scientific study conducted at Shahid Mustafa Khomeini Hospital found SARS-CoV-2 virus RNA in 2 of 14 air samples. In addition, Santarpia et al. (2020) reported the presence of viral RNA in eleven air samples from isolation units and the common room at the University of Nebraska Medical Center. Santarpia et al. (2020) had a small limitation: the distance from the air sampling equipment to the patients’ beds was not considered, which could certainly affect the interpretation of the results (Santarpia et al., 2020). Therefore, we took all samples as described above, at a distance of 1.5 m from the patient's bed, 1.5 m above ground level, for one hour. Another experimental study (Van Doremalen et al. (2020)) reported the possibility of aerosol transmission of SARS-CoV-2 in their experiments using a spray laboratory (Van Doremalen et al., 2020). The authors used a Collison nebulizer to create an aerosol and showed that viable SARS-CoV-2 virus could remain in the aerosol for up to 3 hours after spraying.
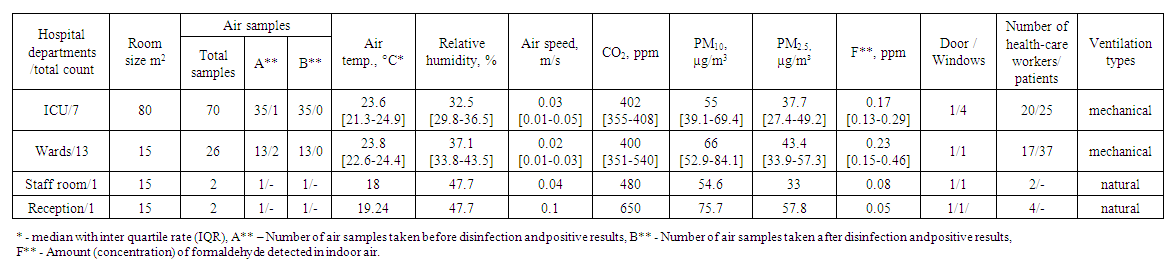 | Table 1. Indicators of air quality in hospital wards |
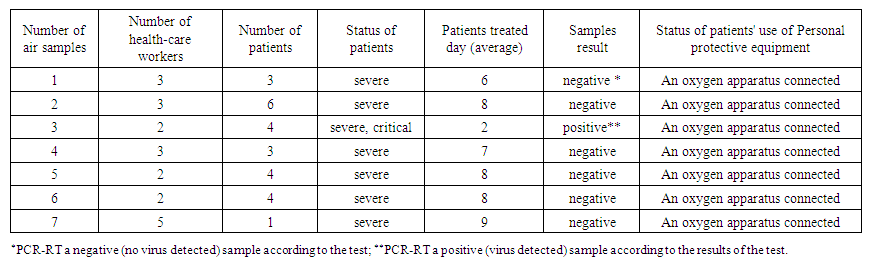 | Table 2. Location of sampling points in the ICU |
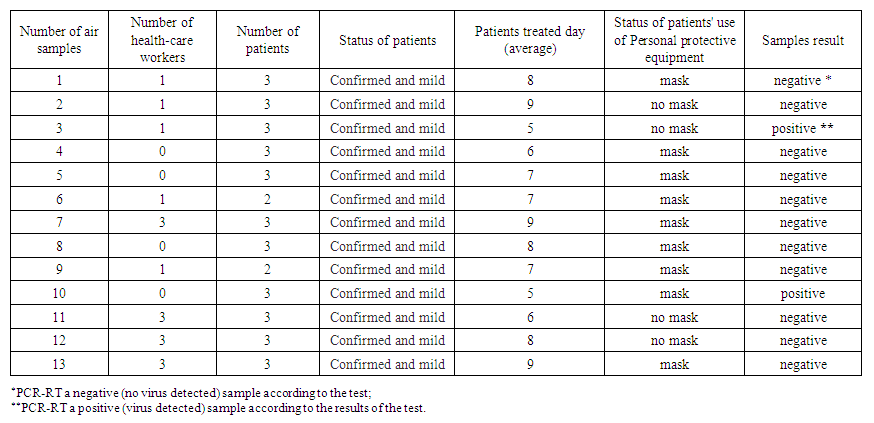 | Table 3. Location of sampling points in the general wards |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML