-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2026; 16(1): 5-9
doi:10.5923/j.ajmms.20261601.02
Received: Nov. 25, 2025; Accepted: Dec. 20, 2025; Published: Jan. 5, 2026

Optimization of Surgical Treatment of Postoperative Ventral Hernias
Bakhriyev Bakhrom Lapasovich 1, 2, Davlatov Salim Sulaymonovich 2, Rakhmanov Kosim Erdanovich 3, Shirinova Shakhinabonu Bobirovna 2
1Zafarabad District Medical Association, Jizzakh, Uzbekistan
2Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan
3Samarkand State Medical University, Uzbekistan
Correspondence to: Davlatov Salim Sulaymonovich , Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan.
| Email: |  |
Copyright © 2026 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Incisional ventral hernias (IVHs) represent a significant problem in surgical practice, and their incidence varies depending on various factors, including the type of surgery, patient age, gender, and the presence of comorbidities. The aim of the study was to evaluate the results of surgical treatment of patients with postoperative ventral hernias. Materials and methods of research. A retrospective analysis of surgical treatment outcomes was conducted for 149 patients with postoperative hernias treated in the surgical department of the Zafarabad district medical association in the Jizzakh region from 2021 to 2024. Patients were divided into two groups: a study group (n=75), which utilized advanced hernioplasty techniques, and a comparison group (n=74), which utilized traditional methods. Study results. Patients in the first comparison group underwent hernioplasty using local tissues and hernioplasty using a polypropylene prosthesis. According to the indications, combined interventions were performed: cholecystectomy, hernioplasty Inguinal hernia. In 19 (35.2%) patients, omental resection was performed due to severe adhesions, viscerolysis, to prevent adhesive intestinal obstruction, and to reduce the volume of the abdominal cavity to prevent increased intra-abdominal pressure. Conclusion. The obtained results emphasize that the success of surgical intervention for anterior ventral hernia depends not only on the quality of the technique used but also on comprehensive diagnostics, competent planning, and a personalized approach to each patient. Implementation of these principles contributes to increased safety, improved functional outcomes, and a reduced risk of reoperation.
Keywords: Ventral hernias, Hernial defect, Laparoscopy, Hernioplasty, Surgery
Cite this paper: Bakhriyev Bakhrom Lapasovich , Davlatov Salim Sulaymonovich , Rakhmanov Kosim Erdanovich , Shirinova Shakhinabonu Bobirovna , Optimization of Surgical Treatment of Postoperative Ventral Hernias, American Journal of Medicine and Medical Sciences, Vol. 16 No. 1, 2026, pp. 5-9. doi: 10.5923/j.ajmms.20261601.02.
1. Introduction
- Incisional ventral hernias (IVHs) represent a significant problem in surgical practice, and their incidence varies depending on various factors, including the type of surgery, patient age, gender, and the presence of comorbidities [1].According to various studies, the incidence of PIH ranges from 10% to 20% in patients undergoing abdominal surgery. Some meta-analyses report higher rates, reaching 30% or more, especially in high-risk patients (e.g., those undergoing repeat surgeries or in obese patients) [2,3,4].Ventral hernia treatment involves the use of various surgical techniques, which are selected based on the hernia characteristics, the patient's condition, and the surgeon's experience. The main methods are open surgery and laparoscopy.In an open operation, an incision is made in the area of the hernial orifice, after which the hernial sac is removed, the contents are returned to the abdominal cavity, and the defect in the abdominal wall is closed with sutures or mesh implantation. The laparoscopic technique involves making several small incisions (usually 0.5–1 cm) through which a camera and instruments are inserted. The hernial opening is closed using mesh implants under video guidance [5,6,7].The choice of surgical treatment method depends on many factors: hernia size, the presence of adhesions, the patient's general condition, and the surgeon's experience. Open surgery remains a reliable method for large or complex hernias, while laparoscopy is the preferred option for small and medium-sized hernias to minimize trauma and speed recovery [8,9]. One of the key elements of modern hernia surgery is the use of mesh implants (meshes) to strengthen the abdominal wall and reduce the risk of hernia recurrence. The correct choice of mesh type and its characteristics significantly impacts the surgical outcome and the patient's quality of life [10].The aim of the study was to evaluate the results of surgical treatment of patients with postoperative ventral hernias.
2. Materials and Methods of Research
- A retrospective analysis of surgical treatment outcomes was conducted for 149 patients with postoperative hernias treated in the surgical department of the Zafarabad district medical association in the Jizzakh region from 2021 to 2024. Patients were divided into two groups: a study group (n=75), which utilized advanced hernioplasty techniques, and a comparison group (n=74), which utilized traditional methods.The key factors determining the choice of surgical approach are the location of the hernia, the size of the hernia defect, and the presence of recurrences in the patient's medical history. According to the classification of Chervel JP and Rath AM (1999), 62 patients (41.6%) had large (W3) and giant (W4) hernias.
3. Study Results
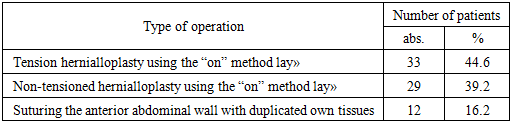
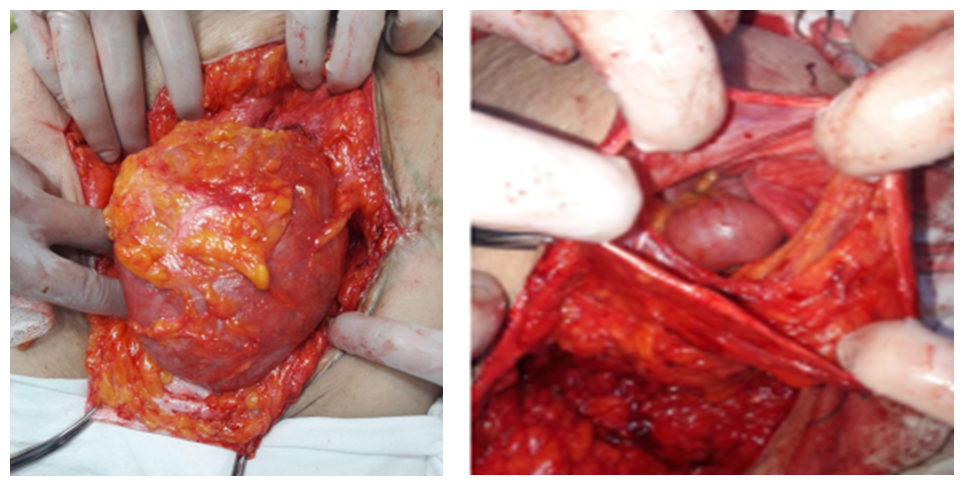
- Patients in the first comparison group underwent hernioplasty using local tissues and hernioplasty using a polypropylene prosthesis.According to the indications, combined interventions were performed: cholecystectomy, hernioplasty Inguinal hernia. In 19 (35.2%) patients, omental resection was performed due to severe adhesions, viscerolysis, to prevent adhesive intestinal obstruction, and to reduce the volume of the abdominal cavity to prevent increased intra-abdominal pressure.In patients in the comparison group, hernioplasty was performed using tension and non-tension methods, both local tissues and polypropylene implants (Table 1).
|
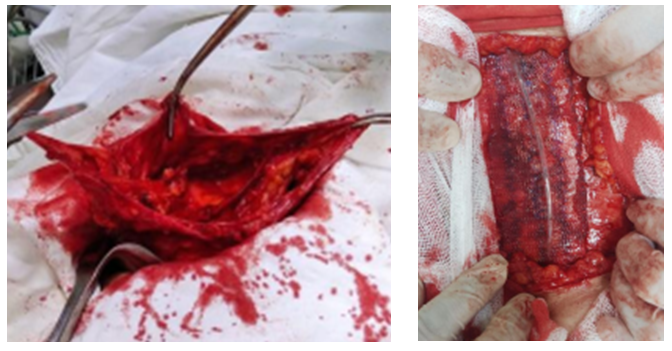
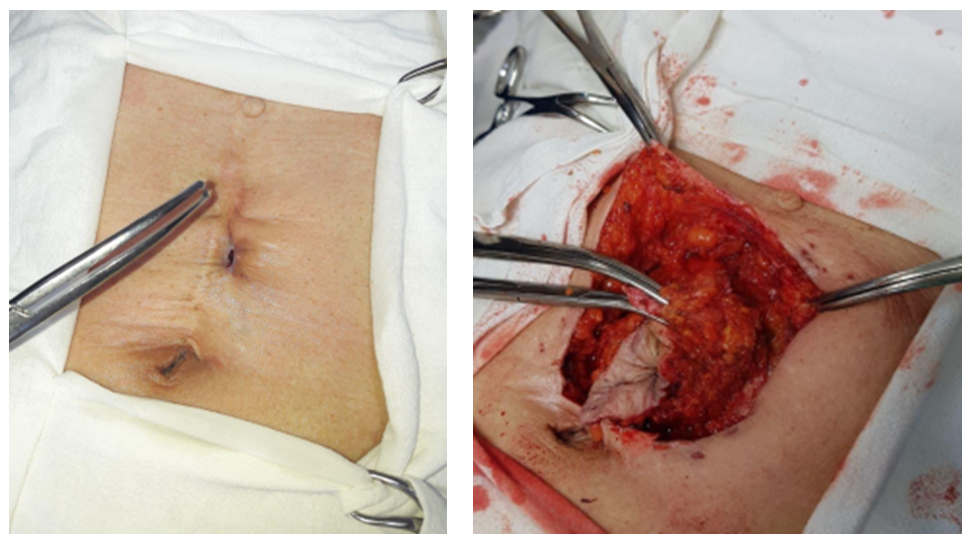 | Figure 1. Excision of a postoperative scar with altered subcutaneous fat |
 | Figure 2. Isolation of the hernial sac while maintaining tissue integrity in order to eliminate the hernial defect |
 | Figure 3. Separation of adhesions between the hernial sac and contents |
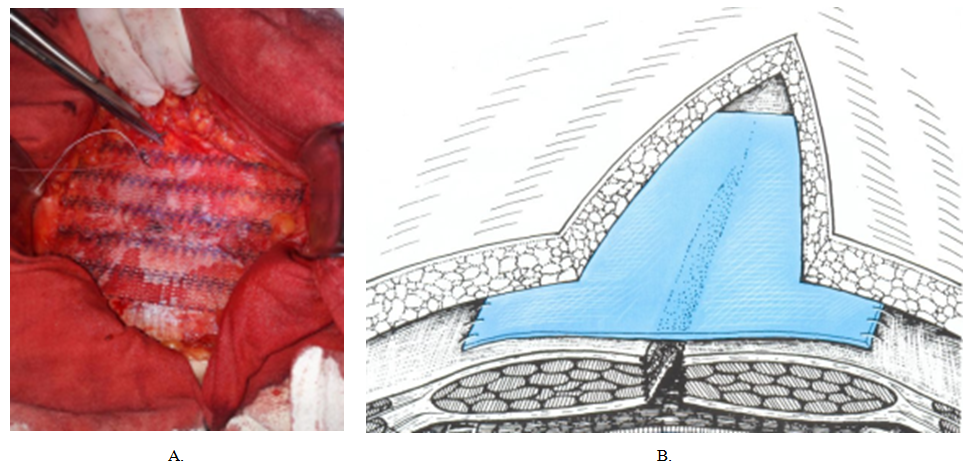 | Figure 4. a. Placement of the explant in front of the muscular-aponeurotic layer, b. Schematic representation according to V.V. Zhebrovsky, F.N. Ilchenko, 2004 |
 | Figure 5. CTGA of patient R., 49 years old, No. IB 2965/268 |
 | Figure 6. Implantation of the “onlay” endoprosthesis without suturing the defect |
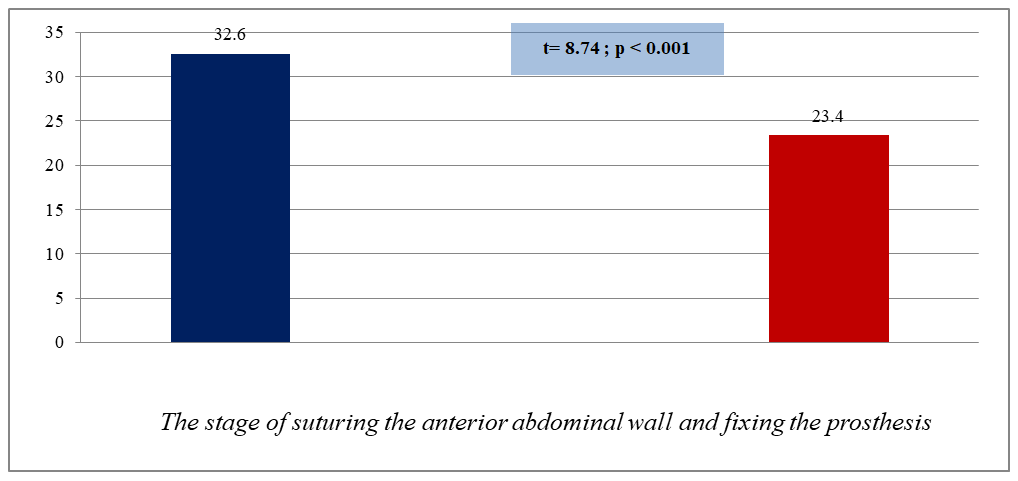 | Figure 7. Time period for suturing the anterior abdominal wall and fixing the prosthesis using modernized technical aspects |
4. Conclusions
- Overall, technical improvements implemented in the study group significantly enhanced intraoperative control, ensured anatomically sound restoration of the anterior abdominal wall layers, and provided more stable fixation of the prosthetic implant. In contrast to the comparison group, where standard onlay and sublay techniques were used without modification, the study group employed optimized stages of hernioplasty, including refined dissection planes, improved mesh positioning, and enhanced methods of fixation aimed at reducing dead space and tissue tension. These modifications contributed to a lower incidence of postoperative complications-particularly seromas, hematomas, and inflammatory reactions at the implantation site-and resulted in a shorter postoperative recovery period.The absence of laparoscopic hernia repair in this study is explained by the predominance of large and complex postoperative ventral hernias, extensive scar tissue, and previous multiple abdominal surgeries in the examined patient cohort, which limited the feasibility and safety of minimally invasive approaches. Under these conditions, open reconstructive techniques allowed for better visualization, adequate excision of scar tissue, precise anatomical reconstruction, and reliable mesh fixation.The obtained results emphasize that successful surgical treatment of postoperative ventral hernias depends not only on the technical execution of the procedure but also on comprehensive preoperative diagnostics, careful surgical planning, and a personalized approach to each patient. Implementation of these principles improves surgical safety, enhances functional outcomes, and reduces the risk of reoperation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML