Bobokulov Nurullo Asadovich, Abdurahmanov Diyor Shukurullayevich, Kurbaniyazov Zafar Babajanovich
Samarkand State Medical University, Uzbekistan
Correspondence to: Abdurahmanov Diyor Shukurullayevich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Relevance. The problem of varicocele and its impact on male fertility has been the subject of close attention from urologists, andrologists, and reproductive specialists for decades. Varicocele is diagnosed in 15-20% of men in the general population and up to 40% of men with primary infertility, which emphasizes its significant role as a factor associated with reproductive dysfunction. Research objective. To clinically substantiate the effectiveness of microsurgical operations for varicocele based on the dynamics of testicular blood flow and changes in sperm parameters and fertility. Materials and methods. This work is based on the analysis of clinical data and observations of 139 patients with varicocele during the period 2020-2024. The age of the operated patients ranged from 15 to 46 years. Most patients were under 30 years old. It should be noted that patients aged 26 and older constituted 36.0% of the group. This is due to various reasons. Primarily, it is due to late diagnosis. When studying the duration of the disease, it was revealed that patients more frequently sought medical attention after more than 2 years from the onset of the condition. Results and discussion. The results of surgical interventions in 139 patients with varicocele, observed for up to one year or longer, were analyzed. All patients had pathospermia of varying degrees. Four methods of surgical intervention were performe. In each group, patients with grade III varicocele predominated. All surgical interventions were performed by a single surgical team. A WILD operating microscope, a set of micro-instruments, and 8/0 atraumatic sutures were used. The Ivanissevich procedure was performed in its classical form. The Marmar operation was also performed in its classical form, while microsurgical varicocelectomy was performed using a subinguinal approach. The vascularization procedure was performed through an inguinal incision. After isolating the internal epigastric vein and the vein circumflexing the iliac bone, the integrity of the vein valves was checked using a two-forceps test. Conclusions. The results of surgical treatment of varicocele were better after the use of microsurgical interventions, as evidenced by improved testicular blood flow by 10% and 31% respectively after the Marmar-Goldstein procedure and vascularization, positive changes in sperm parameters, and increased fertility.
Keywords:
Varicocele, Hemodynamic type of reflux, Surgical treatment, Microsurgical operations
Cite this paper: Bobokulov Nurullo Asadovich, Abdurahmanov Diyor Shukurullayevich, Kurbaniyazov Zafar Babajanovich, Evaluation of Recurrence Causes After Surgical Treatment of Varicocele, American Journal of Medicine and Medical Sciences, Vol. 15 No. 10, 2025, pp. 3432-3439. doi: 10.5923/j.ajmms.20251510.32.
1. Relevance
The problem of varicocele and its impact on male fertility has been the subject of close attention from urologists, andrologists, and reproductive specialists for decades. Varicocele is diagnosed in 15-20% of men in the general population and up to 40% of men with primary infertility, which emphasizes its significant role as a factor associated with reproductive dysfunction. Despite this, the issue of choosing the optimal surgical treatment method for patients with impaired fertility remains a subject of active scientific debate [1,2].At present, more than ten different methods for surgical treatment of varicocele have been developed and are being applied, including open (according to Ivanissevich, Palomo, Marmar), laparoscopic, endoscopic, and microsurgical interventions. Numerous studies, including meta-analyses [3,4], demonstrate the advantages of microsurgical varicocelectomy in terms of reducing the frequency of recurrence and postoperative complications (hydrocele, arterial damage, persistent pain), as well as improving spermatogenesis parameters [5].Nevertheless, the level of evidence regarding the direct correlation between varicocele treatment and fertility restoration remains moderate. This is due to the heterogeneity of populations, differences in sperm analysis evaluation protocols, and the lack of unified criteria for selecting patients for surgical treatment. According to the European Association of Urology (EAU, 2023), indications for surgery in infertile men with clinically evident varicocele are established only if there are abnormalities in the sperm analysis and other factors of infertility have been excluded [6,7].In recent years, there has been growing interest in personalized approaches to varicocele treatment. Some authors [8] suggest considering parameters such as hormonal profile, sperm DNA fragmentation level, oxidative stress index, and ultrasound characteristics of venous reflux. Despite this, there are still no clearly formulated clinical criteria for selecting the surgical intervention method based on the severity of fertility disorders, patient age, varicocele stage, and preoperative diagnostic results [9].The question of whether surgical treatment is advisable for subclinical varicocele and varicocele in men with normal sperm parameters but unsuccessful conception attempts also remains controversial. Some randomized studies [10] indicate a lack of significant benefits in this group, while other observational studies demonstrate positive changes in sperm quality and pregnancy rates following surgical correction [11].Thus, despite the existence of numerous publications on the surgical treatment of varicocele, the degree of understanding regarding criteria for selecting a specific intervention method in patients with impaired fertility remains insufficient. There is no unified algorithm that accounts for the combination of clinical, laboratory, and instrumental data. This indicates the need for further prospective studies, including a comprehensive assessment of spermatogenesis, hormonal status, and patients' quality of life, as well as the development of individualized clinical recommendations for choosing optimal surgical intervention tactics.Research objective. To clinically substantiate the effectiveness of microsurgical operations for varicocele based on the dynamics of testicular blood flow and changes in sperm parameters and fertility.
2. Materials and Methods
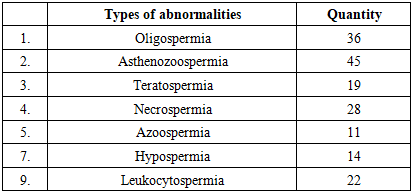
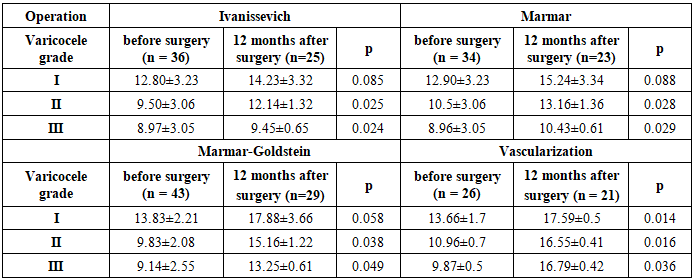
This work is based on the analysis of clinical data and observations of 139 patients with varicocele during the period 2020-2024. The age of the operated patients ranged from 15 to 46 years.Most patients were under 30 years old. It should be noted that patients aged 26 and older constituted 36.0% of the group. This is due to various reasons. Primarily, it is due to late diagnosis. When studying the duration of the disease, it was revealed that patients more frequently sought medical attention after more than 2 years from the onset of the condition.The Dubin and Amelar classification was used to determine the severity of varicocele. According to this classification (WHO, 1993, 1997), all cases of the disease are divided into 2 groups: the first group is clinical varicocele, the second is subclinical. Patients with subclinical varicocele were not included in our study.Depending on the severity of varicocele and the age of the patients, stages II and III of the disease predominated. Patients with stage III varicocele constituted the largest group. Patients over 35 years of age mainly sought surgical intervention due to pain in the testicular region.The most commonly observed symptoms were enlargement of the scrotum, pain, discomfort in the testicular area, and testicular hypotrophy on the left side.When performing semen analysis, special attention was paid to factors contributing to decreased fertility: testicular volume of 12 ml3 or more on one side (based on palpation and ultrasound findings), and the presence of varicocele. In cases of infertility, pathology of the genitourinary system and the inability of wives to conceive within one year without contraception were taken into account. Observation of patients' wives by a gynecologist and the presence of a medical conclusion were required. When interpreting semen analyses, both qualitative and quantitative changes in semen were found in all 139 patients with varicose veins of the spermatic cord. These changes were detected regardless of the degree of varicocele.Table 1 shows changes in semen that were not related to age and varicocele progression characteristics. Not only isolated changes were noted, but also their combinations.Table 1. Types of pathospermia in varicocele (n=139)
 |
| |
|
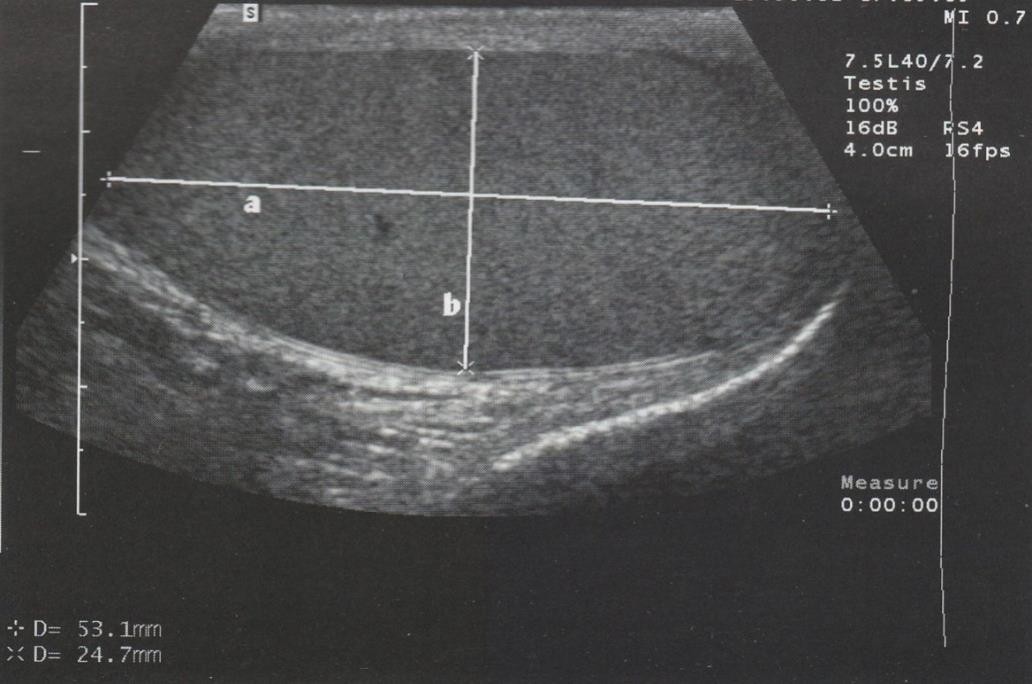
Doppler sonographic studies were conducted to assess testicular blood circulation and determine the hemodynamic type of varicocele. This allows for the identification of qualitative and quantitative characteristics of testicular blood circulation. Visually, it is possible to detect a decrease or increase in blood flow zones.Ultrasound scanning of the testicular vessels is a complex and time-consuming procedure. The difficulties were primarily related to the contraction of the muscle that lifts the testicle, the inability to precisely hold the sensor due to the use of gel, and the variability of the anatomical features of the testicular vessels.This method allows for non-invasive determination of linear blood flow velocity and the viability of anastomoses in dynamics after surgery. It also helps to determine the rate of reverse flow along the spermatic vein using the Valsalva maneuver (Figures 1, 2).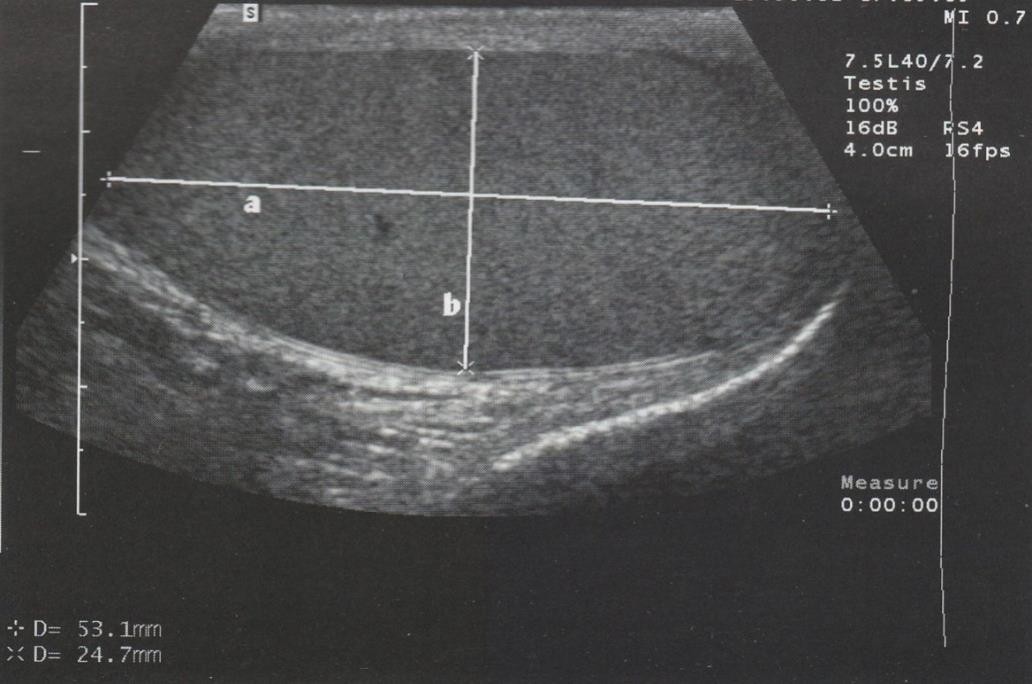 | Figure 1. Testicle in longitudinal section with its dimensions marked: a - length, b - transverse dimension |
 | Figure 2. Blood backflow curve |
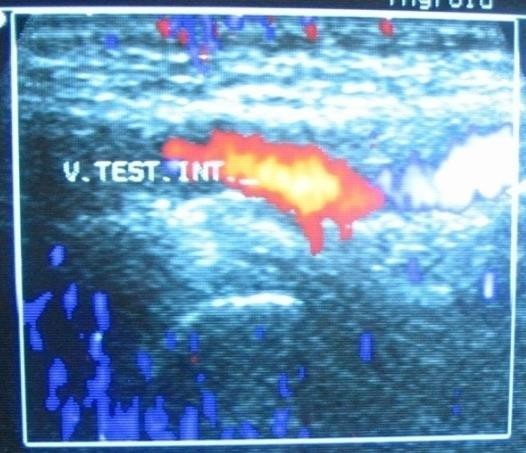
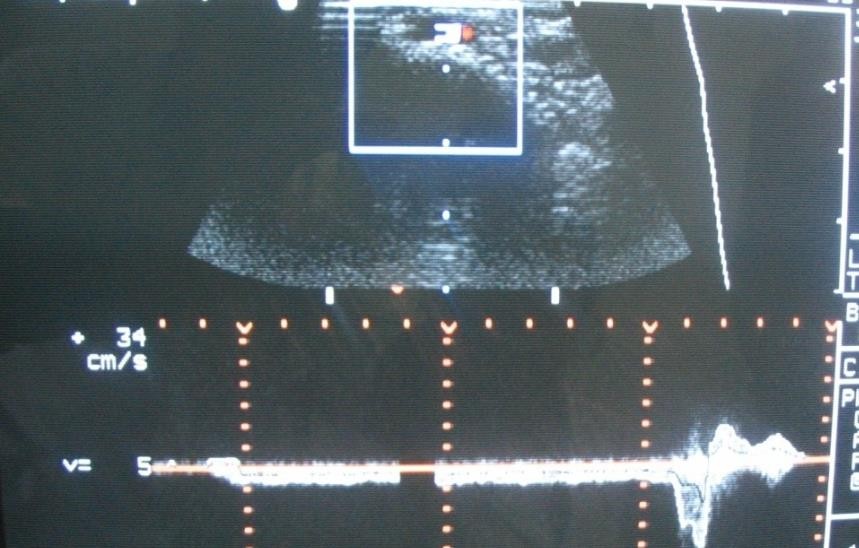
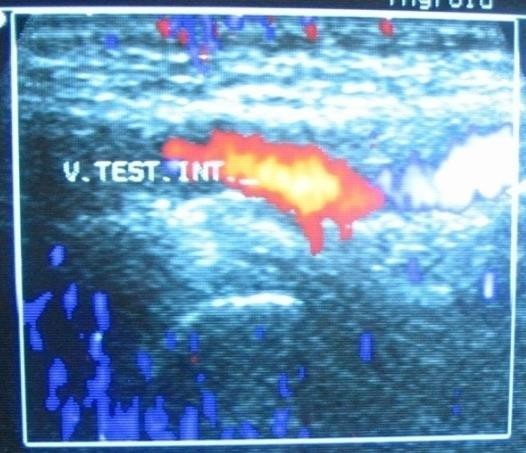
This method allows for the registration of blood flow after the formation of microanastomoses at various periods following surgery. A distinctive feature of this method is that it enables recording blood flow in the restored vessel. The obtained Doppler sonogram allows for an objective analysis of blood flow characteristics.Angioscanning of testicular vessels allows visualization not only of the vessel sizes but also provides their structural characteristics.For a comprehensive examination, studies were conducted on the renal veins, external and internal iliac veins, internal spermatic vein and scrotal veins, the presence of reflux with the Valsalva maneuver, and the condition of the ostial valve of the great saphenous vein. (Fig. 3, 4).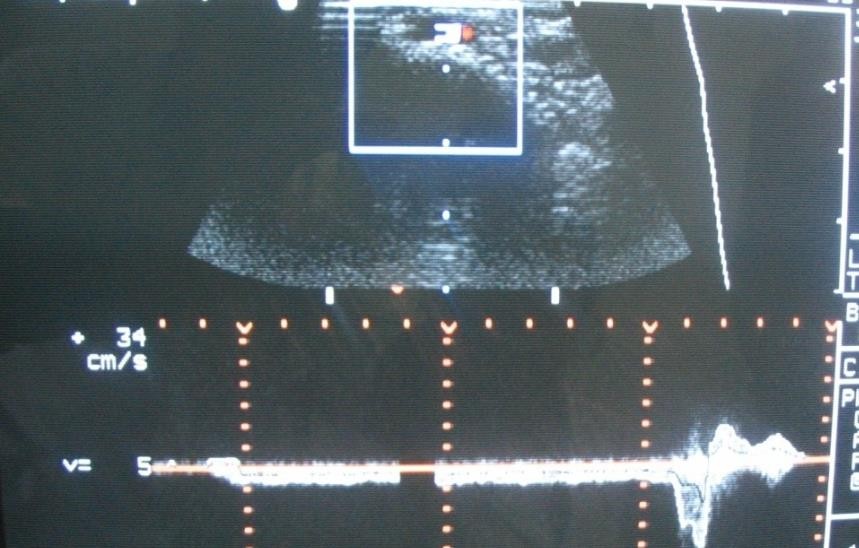 | Figure 3. Duplex spectrogram of blood flow in the internal spermatic vein |
 | Figure 4. Cross-section of the internal spermatic vein |
When using Doppler methods, we considered it important to study the blood flow velocity in the testicular vessels, the degree of blood backflow through the seminal veins in the pampiniform plexus at rest and during straining. Studies were conducted in standing and lying positions. The obtained vascular Doppler waveforms were evaluated qualitatively and quantitatively. Attention was paid to the characteristics of blood flow velocity, while the absolute value of blood flow velocity was not taken into account. We focused on the shape of the Doppler waveform, considering the distribution of Doppler frequencies and the direction of blood flow. It is important to assess the quantitative characteristics of blood flow, and the evaluation of blood flow was informative, taking into account both the true parameters and the calculated indices.
3. Results and Discussion
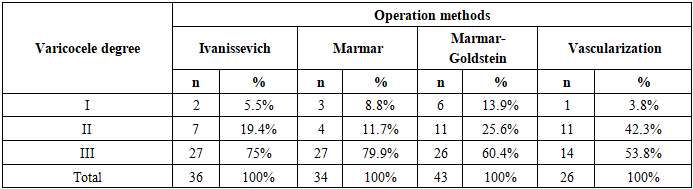
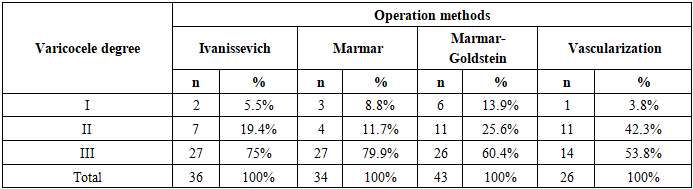
The results of surgical interventions in 139 patients with varicocele, observed for up to one year or longer, were analyzed. All patients had pathospermia of varying degrees. Four methods of surgical intervention were performed (Table 2).Table 2. Number of patients depending on the surgical method and degree of varicocele (n=139)
 |
| |
|
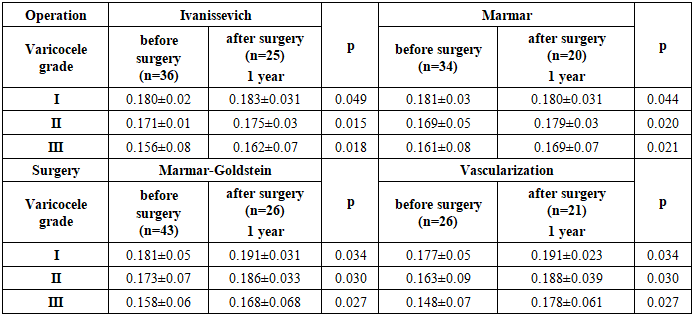
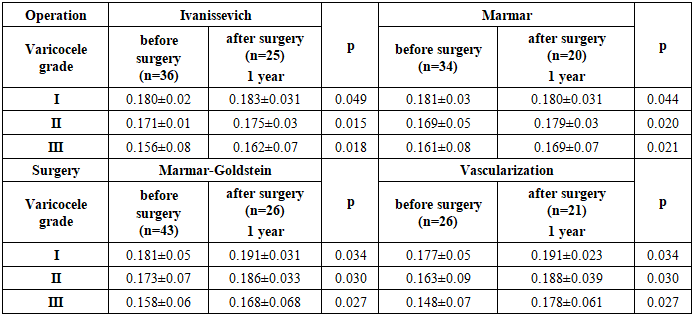
In each group, patients with grade III varicocele predominated. All surgical interventions were performed by a single surgical team. A "WILD" operating microscope, a set of micro-instruments, and 8/0 atraumatic sutures were used. The Ivanissevich procedure was performed in its classical form. The Marmar operation was also performed in its classical form, while microsurgical varicocelectomy was performed using a subinguinal approach. The vascularization procedure was performed through an inguinal incision. After isolating the internal epigastric vein and the vein circumflexing the iliac bone, the integrity of the vein valves was checked using a two-forceps test. The same test was conducted when isolating the great saphenous vein. In cases of valve insufficiency in these veins, the vascularization surgery was abandoned, and microsurgical varicocelectomy was performed instead. Typically, valve insufficiency in the iliac vein tributaries is associated with insufficiency in the great saphenous vein. Among our patients, venous valve insufficiency was observed in 9 cases. Types of vascularization were performed based on the hemodynamic type of varicocele. In the ileospermatic hemodynamic type, distal testicular-epigastric anastomosis was formed in 14 patients, and testicular-saphenous anastomosis in 5 patients. In the renospermatic hemodynamic type of varicocele, a proximal testicular-epigastric anastomosis was formed in 2 patients. In the mixed hemodynamic type of varicocele, after transecting the internal spermatic vein, two anastomoses were formed with tributaries of the iliac vein in 5 patients. One of the main indicators in the diagnosis of varicocele is the rate of blood backflow through the veins of the pampiniform plexus or spermatic cord during straining, which was most often proportional to the severity of the disease. The rate of backflow through the veins is measured in m/s and is considered positive if it lasts longer than 1 second. We considered a positive result to be an amplitude duration of more than 2 seconds. If the backflow rate lasts less than 1-2 seconds and the backflow velocity is less than 0.080 m/s, it can be stated that there is no varicocele. The backflow velocity in varicocele was I grade with straining up to 0.2 m/s, II grade - up to 0.4 m/s, and III grade - above 0.6 m/s. The severity of blood backflow indicates the degree of venous hypertension, testicular insufficiency, and the state of venous collaterals. It should be noted that both the average diameter of the veins and the average rate of blood backflow through the veins of the pampiniform plexus differed between the right and left sides (the average diameter of the veins on the left was 5.1±0.2 mm, on the right - 2.3±0.2 mm). After surgery in patients, with the exception of disease recurrence, the rate of blood backflow was not recorded. When measuring the blood flow velocity in the testicular arteries before surgery, its decrease was recorded depending on the severity of varicocele (table 3).Table 3. Blood flow rate in testicular arteries in patients with varicocele before and after surgery (m/s)
 |
| |
|
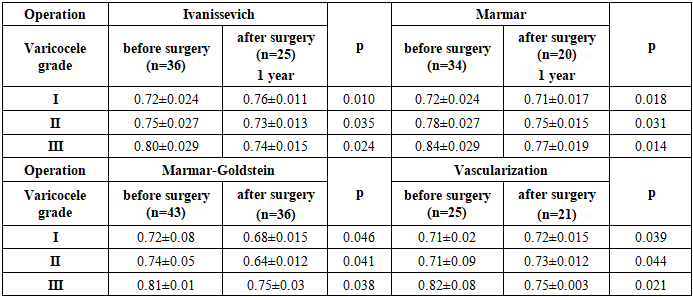
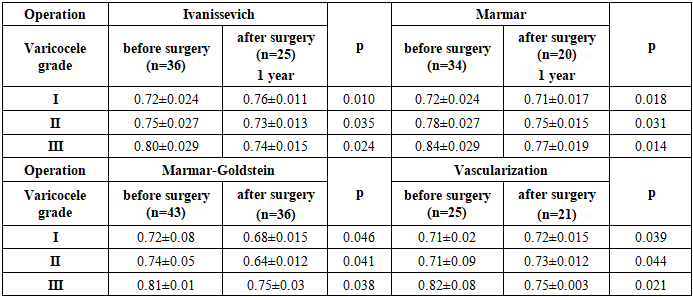
After Ivanissevich and Marmar surgeries, a slight increase in blood flow velocity was observed, although in grade III varicocele, it still remained at relatively low levels (0.162±0.07 m/s). We attribute this to the excessive dilation of the pampiniform plexus veins, which did not regress. These changes were noted in patients without damage to the testicular arteries. In patients who underwent Marmar-Goldstein surgery and vascularization, blood flow velocity was significantly (p<0.05) higher than before surgery, although somewhat lower compared to normal values.When assessing the resistance index in the testicular artery before surgery, a noticeable increase in its values was observed. In the postoperative period, these values decreased significantly but did not reach normal levels after Ivanissevich and Marmar operations. It should be noted that these indicators after surgery were for patients who did not have complications (recurrence, hypotrophy, hydrocele). After microsurgical operations, a noticeable decrease in the resistance index was observed, reaching normal values (Table 4). Table 4. Resistance index in left testicular arteries before and after surgery
 |
| |
|
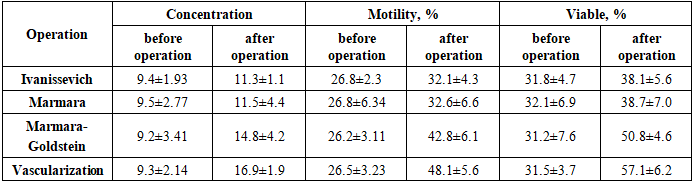
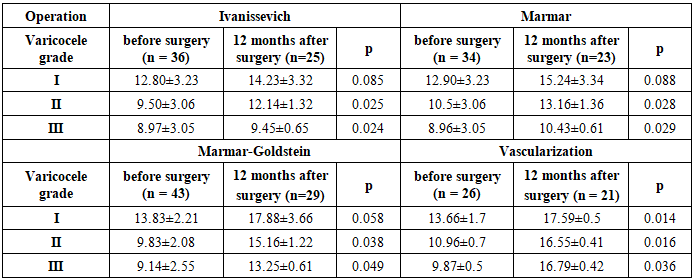
To determine testicular volume, all patients underwent ultrasound examination of the testes. Left testicular hypotrophy was detected in all operated groups. Moreover, the decrease in testicular volume depended on the severity of varicocele and the duration of the disease (Table 5). Table 5. Testicular volume in hypotrophy depending on the severity of varicocele before and after surgery (cm3)
 |
| |
|
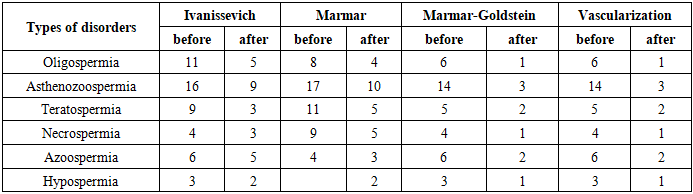
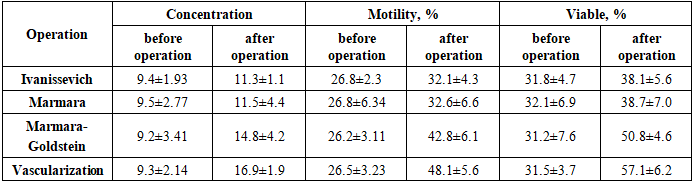
An increase in testicular volume was observed after all surgeries. However, the volume increase after Ivanissevich's and Marmar's surgeries for stage I varicocele reached 14.25±3.32 cm3 and 15.32±3.34 cm3; for stage II - up to 12.16±1.32 cm3 and 13.15±1.36 cm3; for stage III - up to 9.42±0.65 cm3 and 10.42±0.61 cm3 respectively. Despite the increase in testicular volume, these indicators were still below normal values. Testicular enlargement was significantly better after microsurgical varicocelectomy and vascularization surgery: for stage I, it was 17.88±3.66 cm3 and 17.59±0.5 cm3; for stage II - 15.16±1.22 cm3 and 17.53±0.41 cm3; for stage III - 13.25±0.61 cm3 and 16.71±0.42 cm3 respectively. After Ivanissevich's surgery, only two patients had testicular volume reaching the lower limit of normal values (14.20±3.32 cm3). Additionally, 3 patients showed a decrease in testicular volume to 9.45±3.06 cm3.After Marmara's operation, a tendency towards equalization of testicular volume was observed in 6 patients. The other 5 patients showed no improvement. However, in 4 patients who had normal testicular volume values, hypotrophy of this organ was detected, which was associated with testicular artery damage. After microsurgical varicocelectomy and vascularization, no reduction in testicular volume was observed. Nevertheless, due to the wide range of individual data, as indicated by large standard errors of the mean, we did not obtain statistically significant values of volume changes. Despite this, ultrasound examination of the testes remains a valuable indicator for diagnosing and monitoring testicular volume after surgery.When assessing the condition of the ejaculate before and after surgery, within 6 to 12 months, a noticeable quantitative and qualitative improvement in sperm parameters was noted (Table 6).Table 6. Spermogram indicators before and after surgery
 |
| |
|
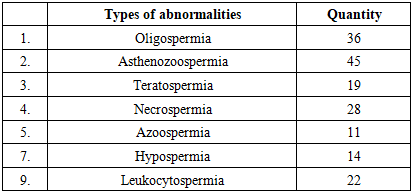
After Ivanissevich's and Marmar's surgeries, sperm parameters showed little improvement: 6 patients showed no improvement, while 3 showed deterioration. In particular, the concentration, motility, and quantity of live sperm increased. After microsurgical varicocelectomy and vascularization, a more significant improvement in sperm parameters was noted. However, this was not observed in all patients. Thus, no improvement in sperm parameters was observed in 3 patients after microsurgical varicocelectomy and in 1 after vascularization, but they did not show deterioration either. Severe changes in sperm parameters were observed in patients older than 26 years and did not depend on the severity of varicocele.With the improvement of the quantitative and qualitative characteristics of sperm after surgery, the types of pathospermia also changed. However, isolated disorders of sperm parameters are rare, and in our cases, they were combined. Therefore, in some patients, all parameters improved, while in others, only some, and it was statistically impossible to draw parallels between them (Table 7). Nevertheless, after surgery, the number of patients with all types of sperm disorders decreased. Among patients who underwent Ivanissevich's surgery, 36 had pathospermia, of which 10 were in married couples. During the observation period, 3 (33%) wives became pregnant.Table 7. Types of pathospermia disorders before and after surgery
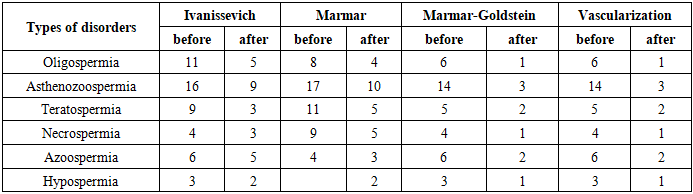 |
| |
|
There were 34 patients with pathospermia who underwent Marmar surgery. Of these, 8 operated patients were in married couples. During the observation period, 2 (25%) wives became pregnant.In the group of patients who underwent microsurgical varicocelectomy, there were 43 people with pathospermia. Of these, 5 operated patients were married. During the observation period, 2 (40%) wives became pregnant.All patients who underwent vascularization surgery (n=26) had pathospermia. Of these, 8 were in married couples. During the observation period, 6 (75%) wives became pregnant. However, these data are not highly reliable, as the operated patients were observed for only one year after surgery. Furthermore, the female factor of infertility was not fully considered, as the examination of wives by gynecologists was not conducted according to a standard algorithm.When analyzing the data obtained from treating varicocele through the formation of microvascular anastomoses, it should be noted that decompression of the venous system is the optimal pathogenetically justified method. Indications for choosing a particular anastomosis are determined intraoperatively after performing a two-forceps test. The main requirement for selecting an anastomosis during surgery was sufficient outflow through the internal spermatic vein with the patient in a supine position, as this ensured the patency of anastomoses in the immediate postoperative period. Improvement of clinical symptoms, increase in testicular size in cases of atrophy, and restoration of blood circulation after surgery demonstrate the pathogenetic validity of this treatment method. The absence of postoperative hydrocele and lymphostasis, along with the minimization of varicocele recurrence, indicate the effectiveness of microvascular surgeries. Prevention of sperm parameter disorders and their improvement in cases of pathospermia are important. The obtained results showing improved sperm parameters and pregnancies among the wives of these patients support the validity of the performed surgical interventions.Analysis of varicocele recurrence rates revealed their dependence on the type of surgical intervention performed. Specifically, disease recurrence after the Ivanissevich procedure was observed in 9 (25%) cases, after Marmara surgery in 6 (17.6%), and after Marmara-Goldstein surgery in 2 (4.6%). Following vascularization surgery, no disease recurrence was observed. Recurrence in the first days after Ivanissevich's surgery was noted in 9 patients, which we consider to be a false recurrence. In these patients, the hemodynamic type of varicocele was not taken into account. In the remaining 5 patients, disease recurrence developed within 3 months, with a positive Valsalva test. This primarily indicates unnoticed additional veins that expanded over time. Clinical manifestations such as discomfort and pain in the scrotal area and dilated veins persisted in all patients. Moreover, three patients developed testicular hypotrophy, and four developed hydrocele. Left scrotal hyperthermia did not decrease in 4 patients, while hypothermia was noted in 5 patients, indicating ligation of the testicular artery. The recurrence of the disease after Marmar surgery was caused by the gradual dilation of small veins in the spermatic cord that were not detected during the operation, as well as the iliospermatic hemodynamic type of varicocele. It should be noted that all these patients experienced lymphostasis of the spermatic cord in the immediate postoperative period, which required long-term conservative treatment. Discomfort and pain in the scrotum were reported by all patients, and the enlarged size of the scrotum remained unchanged after surgery. Testicular hypotrophy of varying degrees was present in 2 patients, and hydrocele in 1 patient. Hypothermia of the left side of the scrotum was observed in 1 patient, while hyperthermia was seen in 3 patients. It should be noted that Marmar's operation is subject to all the shortcomings inherent in Ivanissevich's operation. The Marmar-Goldstein operation using microsurgical technique proved to be more advanced. The recurrence of the disease in 2 patients is mainly attributed to unnoticed small veins that were not ligated during the operation. All these patients were operated on using a magnifying glass, which has limited magnification capability. However, these patients did not develop lymphostasis, hypotrophy, or hydrocele after surgery. Patients who underwent surgery using an operating microscope (10-15 times magnification) showed no recurrence of the disease. Overall, the Marmar-Goldstein operation is more progressive compared to the aforementioned operations. However, this operation is only effective for the renospermatic hemodynamic type of varicocele.In all cases of varicocele recurrence, the blood flow velocity in the testicular arteries did not show positive dynamics. There was also a tendency towards a decrease in testicular volume. This indicator must be monitored over time, as ultrasound examination can reliably identify changes in volume measurements.Changes in the testicular artery resistance index were also detected 6 months after surgery: in the 1st degree - 0.71±0.04 vs. 0.74±0.04; in the 2nd degree - 0.76±0.06 vs. 0.77±0.06; in the 3rd degree - 0.80±0.04 vs. 0.83±0.004.In the period from 6 to 12 months after surgery, when assessing the condition of the ejaculate, quantitative and qualitative changes in sperm parameters were revealed. Specifically, the concentration of spermatozoa decreased from 8.2 million/ml to 7.7 million/ml (after surgery). A decrease in sperm motility from 24.7 to 21.1% and a reduction in the number of live sperm from 20.6 to 17.2% were observed. However, these qualitative and quantitative changes in semen parameters did not depend on the severity of varicocele and were not equally pronounced in all patients. With the deterioration of sperm parameters after surgery, the types of pathospermia also remained unchanged.Thus, the number of varicocele recurrences is related to the type of surgical intervention performed. According to the obtained results, they were more frequently noted after Ivanissevich and Marmar surgeries, as these methods are less advanced and the hemodynamic type of varicocele was not taken into account when selecting the surgery. Marmar-Goldstein surgery and microsurgical vascularization are more progressive interventions, after which pronounced positive dynamics are observed, improving the quality of life of patients.
4. Conclusions
1. When choosing a method for surgical correction of varicocele, it is necessary to consider the hemodynamic type of reflux according to ultrasound dopplerography. In the renospermatic type of varicocele, occlusive operations are pathogenetically justified.2. Indications for "high ligation" type surgical interventions in the treatment of varicocele should be limited. The Marmar-Goldstein procedure is the method of choice for the renospermatic hemodynamic type. The formation of intervenous anastomoses is indicated for ileospermatic and mixed hemodynamic types of varicocele.3. Performing microsurgical operations, taking into account the hemodynamic type of reflux, is justified by a significant decrease in the recurrence rate of varicocele from 23% to 3%, hydrocele from 7% to 3%, and the mitigation of testicular hypotrophy.4. The results of surgical treatment of varicocele were better after the use of microsurgical interventions, as evidenced by improved testicular blood flow by 10% and 31% respectively after the Marmar-Goldstein procedure and vascularization, positive changes in sperm parameters, and increased fertility.
References
| [1] | Agapov Y.S., Shcheglov A.V. Modern aspects of diagnosis and treatment of varicocele in men with impaired fertility // Urology. - 2020. - No. 2. - P. 33–39. |
| [2] | Eliseev Y.V., Ovchinnikov A.V. Varicocele: pathogenesis, clinical features, diagnosis, treatment // Andrology and Genital Surgery. - 2019. - Vol. 20, No. 3. - P. 45–50. |
| [3] | Morozov A.V., Selivanov P.Yu. Surgical correction of varicocele: modern methods and criteria for selection // Bulletin of the Russian Academy of Medical Sciences. - 2018. - No. 6. - P. 72–76. |
| [4] | Saveliev S.V., Ivanov A.Yu. Influence of varicocelectomy methods on semen analysis parameters // Issues of Andrology. - 2021. - Vol. 27, No. 1. - P. 41–47. |
| [5] | Barmejo C., Rodríguez J., Alcaraz A. Surgical management of varicocele in the era of assisted reproduction // Current Urology Reports. - 2020. - Vol. 21, No. 4. - P. 15–22. |
| [6] | Kantartzi P.D., Goulis C.D., Goulis D.G. et al. Varicocele and male fertility: myths and reality // Hippokratia. - 2007. - Vol. 11, No. 3. - P. 99–104. |
| [7] | Potapov V.A., Lapshin K.V. Laparoscopic varicocelectomy: effectiveness and safety in men with impaired fertility // Surgery. Journal named after N.I. Pirogov. - 2022. - No. 5. - P. 59–63. |
| [8] | Ramasamy R., Schlegel P.N. Microdissection varicocelectomy: a review // BJU International. - 2011. - Vol. 108, No. 11. - P. 1703–1712. |
| [9] | Baazeem A., Belzile E., Ciampi A., Dohle G. et al. Varicocele and male infertility: systematic review and meta-analysis of randomized controlled trials // European Urology. - 2011. - Vol. 60, No. 3. - P. 448–460. |
| [10] | Nikitin D.O., Korchagin N.N. Comparative characteristics of varicocelectomy methods in patients with infertility // Andrology. - 2020. - Vol. 21, No. 2. - P. 53–58. |
| [11] | Erdanovich, R. K., Sulaymonovich, D. S., & Chorievich, M. M. (2020). Modern methods of surgical treatment of varicocele (literature review). Bulletin of Science and Education, (23-2 (101)), 66-70. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML