-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(10): 3412-3416
doi:10.5923/j.ajmms.20251510.28
Received: Sep. 16, 2025; Accepted: Oct. 9, 2025; Published: Oct. 15, 2025

Comparative Analysis of Immunobiochemical Indicators in Biological Fluids in Patients with Acute Purulent-Destructive Orchoepididymitis
Rakhimov F. F.1, Khamdamov B. Z.1, Rashidov Z. R.2
1Bukhara State Medical Institute, Bukhara, Uzbekistan
2Tashkent State Medical University, Tashkent, Uzbekistan
Correspondence to: Rakhimov F. F., Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

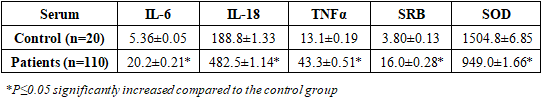
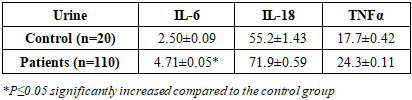
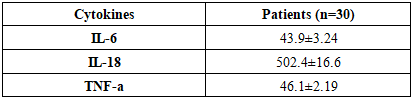
Acute purulent-destructive orchiepididymitis (APDOE) is a severe inflammatory disease of the male reproductive system with complex immune pathogenesis. Objective: to study the role of immunobiochemical and antioxidant markers in the development of acute purulent orchiepididymitis. Methods: 110 patients were examined. Concentrations of immunological markers were measured (IL-6, IL-18, TNF-α, CRP, SOD) by ELISA (Verctor Best). Results: In patients with acute purulent-destructive orchiepididymitis, the levels of IL-6, IL-18, TNF-α and C-reactive protein in the blood serum were significantly higher than the control values (2.5–4.2 times; p < 0.05), while the activity of superoxide dismutase decreased by 1.6 times (p < 0.05). In urine, IL-6 and IL-18 significantly increased (by 1.3–1.9 times; p < 0.05), while TNF-α increased insignificantly. Conclusion: Acute purulent-destructive orchiepididymitis is characterized by pronounced activation of proinflammatory cytokines and systemic imbalance of antioxidant defense, which confirms their diagnostic and prognostic significance.
Keywords: Orchiepididymitis, Cytokines, IL-6, IL-18, TNF-α, Ejaculate, Urine, Systemic inflammation, Local immunity, Immune markers
Cite this paper: Rakhimov F. F., Khamdamov B. Z., Rashidov Z. R., Comparative Analysis of Immunobiochemical Indicators in Biological Fluids in Patients with Acute Purulent-Destructive Orchoepididymitis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 10, 2025, pp. 3412-3416. doi: 10.5923/j.ajmms.20251510.28.
Article Outline
1. Introduction
- Acute purulent-destructive orchiepididymitis (APDOE) is a severe inflammatory lesion of the male reproductive system, characterized by severe tissue damage, intense pain syndrome, fever and a high risk of reproductive dysfunction. The pathology often develops against the background of ascending urogenital infections and is a complex interaction between microbial factors and the host's immune response. Despite surgical interventions and antibacterial therapy, some patients continue to have inflammation and develop complications, including testicular atrophy and infertility [2,5,8,10].In recent years, interest in the role of proinflammatory cytokines in the pathogenesis and progression of APDOE has increased significantly. Mediators such as interleukin-6 (IL-6), interleukin-18 (IL-18), and tumor necrosis factor-alpha (TNF-α) are involved in leukocyte recruitment, increased vascular permeability, and tissue destruction. However, their diagnostic and prognostic value is largely determined by the biological environment in which they are measured. While serum analysis reflects systemic inflammation, local biofluids, such as urine, more accurately indicate the intensity and localization of the immune response in the reproductive tract. This emphasizes the need for comparative analysis of the cytokine profile in various biological fluids for a comprehensive understanding of inflammatory processes in APDOE [1,4,7,13].Another important aspect of APDOE is oxidative stress. Excessive production of reactive oxygen species (ROS) at the site of inflammation leads to lipid peroxidation, DNA damage, and additional cellular damage. The body's antioxidant defense system, in particular the enzyme superoxide dismutase (SOD), plays a key role in counteracting these processes. A decrease in SOD activity reflects a systemic imbalance in oxidative processes and can serve as an indicator of the severity of inflammation and the body's ability to recover. Evaluation of SOD levels in combination with cytokines provides a more complete picture of the immune-oxidative status of patients and can be used to justify therapeutic approaches [3,6,9,12].
2. Purpose of the Research
- Purpose of the study is to study the role of immunobiochemical and antioxidant markers in the development of acute purulent orchitis epididymitis.
3. Materials and Methods
- The study included 110 men aged 18 to 85 years with a confirmed diagnosis of APDOE, who were treated in the surgical department of the Bukhara branch of emergency medical care, which was the base of the Department of Urology of the Bukhara State Medical Institute. Inclusion criteria: confirmed diagnosis of APDOE, no previous immunosuppressive therapy, consent to participate. Exclusion criteria: chronic renal or hepatic failure, systemic autoimmune pathologies, oncological processes, decompensated metabolic disorders. The control group for immunological studies consisted of 20 healthy men of the same age.Concentrations of IL-6, IL-18, TNF-α and CRP in blood serum and urine were determined by ELISA (Vector Best, Russian Federation). Determination of the level of superoxide dismutase (SOD) in blood serum was carried out by ELISA using ELISA-SOD test systems (OOO Cytokine, St. Petersburg, Russia).Statistical data processing was performed using the standard Microsoft Excel 2016 package (Microsoft Corp, USA). During the analysis, the arithmetic mean (M), standard deviation (m), standard error of the mean (m) and Student's criterion (t) with calculation of the significance level (p) were calculated. Differences were considered statistically significant at p<0.05.
4. Results and Discussion
- Studying serum cytokine concentrations in patients with AGDOE allows assessing the nature of the systemic immune response and identifying immunological markers associated with the severity of the disease, the degree of tissue destruction, and the prognosis of the course. However, it should be taken into account that serum indices do not always fully reflect the local destructive process, since blood cytokine levels may depend on many factors: concomitant diseases, endocrine status, age and sex differences, and the general reactivity of the body. Nevertheless, in combination with local inflammation markers determined in urine, serum analysis provides a comprehensive picture of the development and activity of the inflammatory process, complementing the clinical and diagnostic assessment with the systemic immune background. Studying the IL-6 level in acute purulent-destructive orchiepididymitis (APDOE) is important, since this marker reflects the intensity of the inflammatory response, the degree of destructive changes, and the potential risk of systemic complications. The study found that in patients with OGDOE, the concentration of IL-6 in the blood serum was 20.2 ± 0.21 pg/ml, which is statistically significant (p < 0.05) and 3.77 times higher than the same indicator in the control group, where the level of IL-6 was 5.36 ± 0.05 pg/ml.IL-18 in acute purulent-destructive orchiepididymitis (APDOE) is involved in the initiation of purulent inflammation, tissue destruction and the development of a systemic inflammatory response, and can also serve as a marker of the severity of immune activation. The results of this study showed that the level of IL-18 in the blood serum of patients with APDOE was 482.5 ± 1.14 pg/ml, which was significantly (p < 0.05) higher than the control group indicator by 2.55 times (188.8 ± 1.33 pg/ml).TNF-α is involved in the formation of purulent inflammation and tissue destruction, and can also serve as a biomarker of the severity of the immune response and the severity of the condition. The study revealed that in patients with OGDOE, the level of TNF-α in the blood serum was 43.3 ± 0.51 pg / ml, which is significantly higher by 3.30 times (p < 0.05) than in the control group, where this indicator was 13.1 ± 0.19 pg / ml.In acute purulent-destructive orchiepididymitis, determination of the CRP level in the blood serum has diagnostic and prognostic value, since its increase reflects the intensity of inflammation, the degree of tissue destruction and the risk of systemic complications. According to the data obtained, in patients with APDOE, the CRP level in the blood serum was 16.0 ± 0.28 mg / l, which is statistically significant (p < 0.05) 4.21 times higher than the values of the control group - 3.80 ± 0.13 mg / l.Superoxide dismutase (SOD) is a key antioxidant enzyme that protects cells from the toxic effects of superoxide anion, one of the main active forms of oxygen [11]. The concentration of superoxide dismutase (SOD) in patients with pathology was 949.0 ± 1.66 pg/ml, which is significantly lower compared to the control group, in which this indicator reached 1504.8 ± 6.85 pg/ml (Table 1). A 1.59-fold decrease in the SOD level (p < 0.05) reflects a pronounced inhibition of the activity of the enzymatic link of the antioxidant system, which is probably associated with increased production of active forms of oxygen against the background of inflammation and tissue destruction.
|
|
|
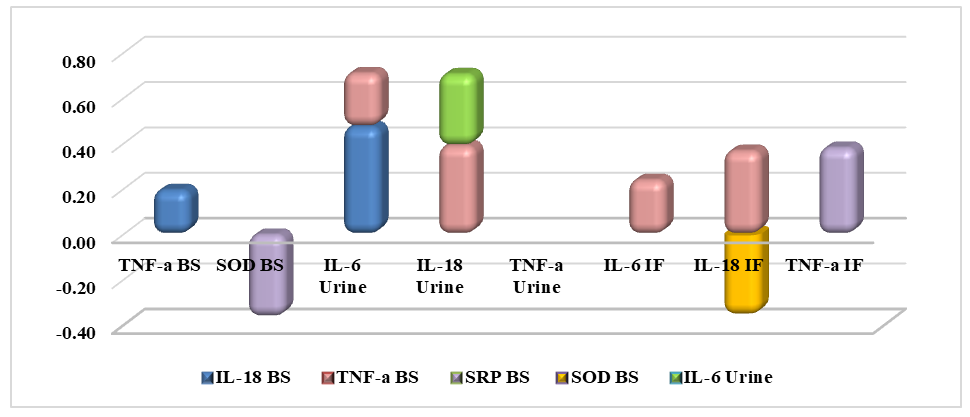 | Figure 1. Correlation analysis of markers of general blood analysis and immunological parameters in patients with APDOE |
5. Conclusions
- Based on the obtained data, it was established that patients with acute purulent-destructive orchiepididymitis have a reliable increase in the levels of the studied markers in the blood serum, indicating a pronounced systemic activation of innate immunity and intensity of the inflammatory response, possibly associated with concomitant pathology, age factors underlying destructive processes in the tissues of the testicle and epididymis. The analysis of the cytokine profile in the urine of patients with acute purulent-destructive orchiepididymitis showed the presence of local immunoinflammatory activity reflected by a reliable increase in the levels of IL-6 and IL-18 compared to the control group. At the same time, the level of TNF-α in the urine did not demonstrate significant differences, which may be due to its predominantly systemic production and limited excretion through the urinary tract.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML