Khaydarov No`monjon Bozor o`g`li1, Rakhmanov Kosim Erdanovich1, Davlatov Salim Sulaymonovich2
1Samarkand State Medical University, Uzbekistan
2Bukhara State Medical Institute, Uzbekistan
Correspondence to: Rakhmanov Kosim Erdanovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Introduction. Differentiated surgical tactics in acute cholecystopancreatitis with the use of minimally invasive interventions is an urgent and intensively studied area of modern surgery. In recent decades, there has been a significant increase in interest in developing optimal algorithms for the treatment of this disease, given the high prevalence of pathology and the complexity of patient management. The purpose of the research. Improving the results of surgical treatment of acute cholecystopancreatitis using minimally invasive technologies. Research materials and methods. 103 patients with acute cholecystopancreatitis (ACP) who were examined and operated on at the SamSMU clinic from 2019-2024 were under observation. We divided all the patients into 2 groups. The control group (group I) consisted of 46.6% patients who underwent traditional open surgical procedures. The remaining 53.4% patients who made up the main group (group II) underwent minimally invasive surgical interventions. The results and their discussion. As can be seen from the table below, laparoscopic cholecystectomy was performed in 34 (56.6%) cases in patients with ACP; Laparoscopic cholecystectomy with assisted EPST using the Rendezvouz technique – in 11 (20%) cases, and EPST and Laparoscopic cholecystectomy – in 7 (12.7%) cases with ACP combined with choledocholithiasis. In 10 (16%) cases of ACP in patients with concomitant somatic diseases and in elderly and senile patients, puncture interventions with drainage of the gallbladder under visual ultrasound control were performed at the first stage, followed by laparoscopic cholecystectomy at the second stage after improvement of the general condition of patients and indicators of endotoxemia, as well as adequate preoperative preparation, Of these, 4 have EPST supplemented at the 2nd stage. Conclusions. Differentiated surgical tactics using laparoscopic hybrid and puncture-draining minimally invasive technologies in the treatment of acute cholecystopancreatitis reduced the number of postoperative complications from 20.8% to 7.3% and mortality from 4.1% to 1.8%.
Keywords:
Acute cholecystopancreatitis, Surgical tactics, Minimally invasive technologies
Cite this paper: Khaydarov No`monjon Bozor o`g`li, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich, Optimization of Surgical Tactics in the Treatment of Acute Cholecystopancreatitis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 10, 2025, pp. 3407-3411. doi: 10.5923/j.ajmms.20251510.27.
1. Introduction
Differentiated surgical tactics in acute cholecystopancreatitis with the use of minimally invasive interventions is an urgent and intensively studied area of modern surgery. In recent decades, there has been a significant increase in interest in developing optimal algorithms for the treatment of this disease, given the high prevalence of pathology and the complexity of patient management [1,5,6].There is a significant amount of research in the existing literature on surgical treatment of acute cholecystopancreatitis [1]. The authors of many studies have noted the advantage of minimally invasive surgical procedures such as laparoscopic cholecystectomy, endoscopic papillosphincterotomy, and ultrasound-guided puncture and drainage procedures. However, to date, there is no single standardized approach to the choice of surgical tactics, due to the variety of clinical manifestations and the severity of the disease [3,4].The purpose of the research. Improving the results of surgical treatment of acute cholecystopancreatitis using minimally invasive technologies.
2. Research Materials and Methods
103 patients with acute cholecystopancreatitis (ACP) who were examined and operated on at the SamSMU clinic from 2019-2024 were under observation. We divided all the patients into 2 groups. The control group (group I) consisted of 48 (46.6%) patients who underwent traditional open surgical procedures. The remaining 55 (53.4%) patients who made up the main group (group II) underwent minimally invasive surgical interventions. The total number of male patients among all the patients we observed was 42 (40.8%), female patients were 61 (59.2%). It was found that in 64 (62.1%) cases, the age of patients was considered to be able-bodied, i.e. up to 60 years old. The remaining 39 (37.8%) patients were over 60 years old. 47 patients had concomitant pathology of the cardiovascular, respiratory and endocrine systems, which affected their overall health.It should be noted that the clinical and morphological forms of cholecystitis and the presence of complications are of great importance for determining the tactics of treatment of patients with ACP. According to the Atlanta classification adopted in 1992, the development of mild acute pancreatitis was observed among patients with phlegmonous and gangrenous forms of acute cholecystitis. There were no cases of moderate to severe pancreatitis among our patients upon admission.All patients in both the main and control groups had various forms of calculous cholecystitis. Catarrhal form was noted in 33.9%, phlegmonous form – in 34.9% and gangrenous form – in 31.1% of patients with pancreatitis. In 40 (38.3%) cases, acute calculous cholecystitis was complicated by choledocholithiasis.Emergency surgery was performed in 23 (47.9%) patients from the control group and in 26 (47.3%) patients from the main group, and delayed surgery was performed in 25 (52.1%) patients from the control group and in 29 (52.7%) patients from the main group.
3. The Results and Their Discussion
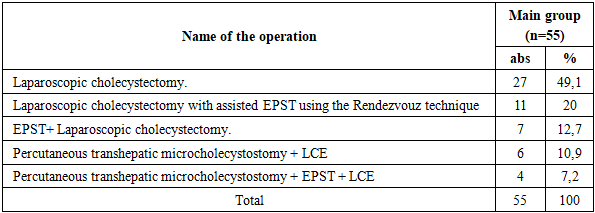
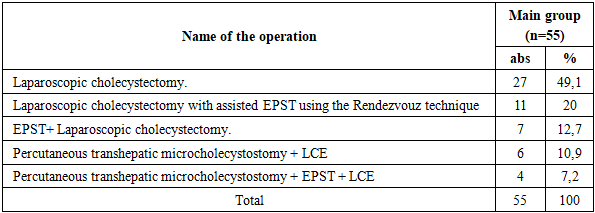
The observed patients with ACP underwent various surgical procedures (Table 1).Table 1. The nature of surgical interventions for ACP in patients of the main group (n=55)
 |
| |
|
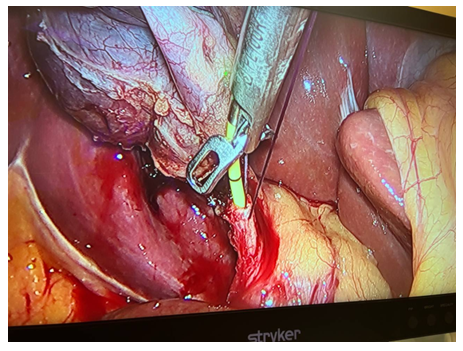
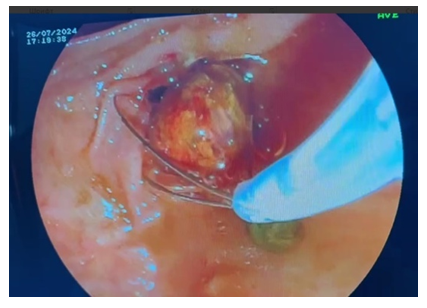
As can be seen from the table above, laparoscopic cholecystectomy was performed in 34 (56.6%) cases in patients with ACP; Laparoscopic cholecystectomy with assisted EPST using the Rendezvouz technique (LERV) – in 11 (20%) cases, and EPST and Laparoscopic cholecystectomy – in 7 (12.7%) cases with ACP combined with choledocholithiasis. In 10 (16%) cases of ACP in patients with concomitant somatic diseases and in elderly and senile patients, puncture interventions with drainage of the gallbladder under visual ultrasound control were performed at the first stage, followed by laparoscopic cholecystectomy at the second stage after improvement of the general condition of patients and indicators of endotoxemia, as well as adequate preoperative preparation, Of these, 4 have EPST supplemented at the 2nd stage.When performing LERV in patients of the first group (11 patients), the gallbladder was removed laparoscopically and the common bile duct was sanitized by endoscopic access through the Large duodenal papilla (LDP). At the first stage, after the cystic artery was isolated, it was clipped with a 5 mm titanium clip and crossed using an U-shaped hook using monopolar cutting. Next, the cystic duct was isolated at its maximum extent. After applying a 5 mm titanium clip to the cystic duct in its distal part, closer to the neck of the gallbladder, an incision of the cystic duct was performed below the applied clip to perform intraoperative direct cholangiography (Fig. 1, 2). 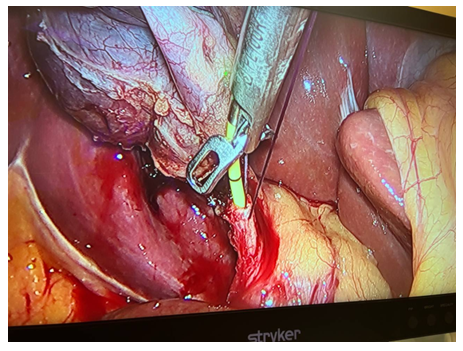 | Figure 1. Intraoperative cholangiography using forceps |
 | Figure 2. Intraoperative cholangiography |
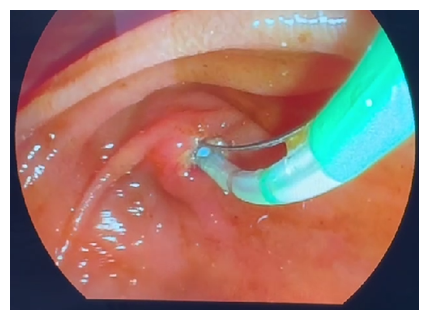
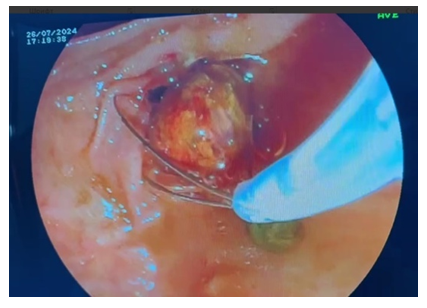
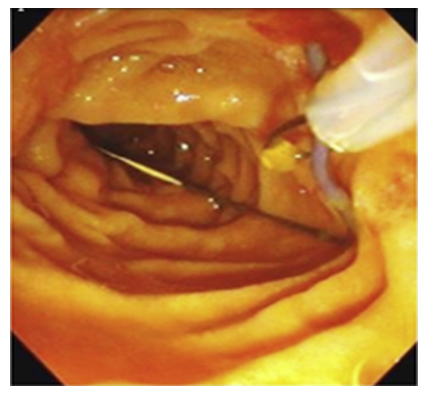
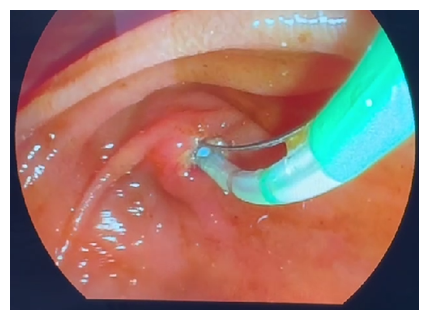
During the second stage of surgery (Rendezvous), joint work of surgical and endoscopic teams is necessary. The surgeon performed an incision of the cystic duct just below the previously applied clip and inserted a 0.035 Fr endoscopic string 450 cm long into the cystic duct through a 3 mm diameter trocar. Then he conducted it antegradely through the LDP into the lumen of the duodenum. After the string was passed through the LDP, the endoscopist conducted a video duodenoscope in the duodenum in the usual way and visualized the LDP in the lumen of which the string was located. From the side of the lumen of the duodenum, the string was captured with a modified hollow endoscopic bougie (Fig. 3).At the third endoscopic stage of the hybrid surgical intervention, the papillot was lowered along the string and inserted into an ampoule of LDP, thus performing selective intubation of the choledochus. Retrograde endoscopic papillosphincterotomy (EPST) was performed using the standard method (Fig. 4).Then the papilloma was removed, leaving an endoscopic string in the biliary tract. Depending on the diameter of the common bile duct and the size of the stones, lithoextraction was performed with four-string Dormia baskets of various sizes and stiffness (Fig. 5). 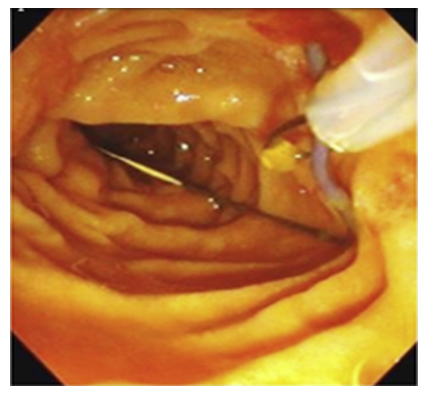 | Figure 3. Capturing the string in the lumen of the duodenum |
 | Figure 4. Papillosphincterotomy |
 | Figure 5. Choledocholithoextraction |
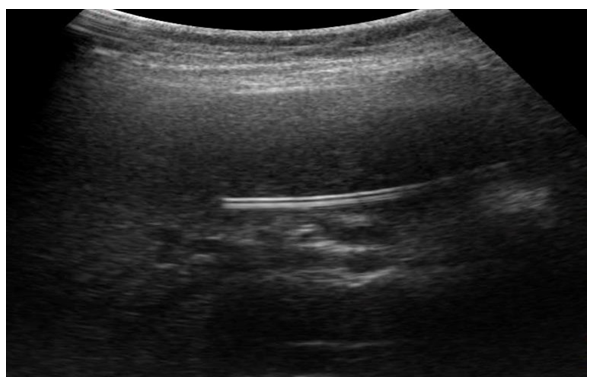
During the fourth stage, laparoscopic cholecystectomy was performed "from the neck".After laparoscopic cholecystectomy is completed, the paraumbilical trocar wound expands, and a 2-3 cm long skin incision is made with dissection of the subcutaneous tissue. At the end of the stage of isolating the round hepatic ligament and determining the umbilical vein, it is recanalized using a button probe, through which a subclavian catheter is inserted, up to the proximal sections of the portal vein, after which the catheter is fixed with a nylon thread.In the postoperative period, broad–spectrum antibiotics are injected into the bloodstream through an installed catheter: cephalosporini – ceftriaxone 1.0 + drugs that suppress pancreatic function - sandostatin 300-600 mg + antioxidants – mexidol 200 mg - for up to 7 days. As the indicators of endotoxemia, cytokine status and lipid peroxidation in the blood decrease and the patient's general condition improves (7-8 days), the catheter is removed.On the 3rd-5th day after administration of the drugs through the round hepatic ligament, patients with ACP showed a decrease in endotoxemia: the CRP level decreased to 115.1±12.8 mg/l, the number of leukocytes decreased to 6.3±0.8 x109/l, the LII values averaged 3.5±0.3 conl.units, MWS (medium molecular weight substances) - 674.25±40.5 micrograms/ml, lipid peroxidation - DC - 0.85±0.25 units, MDA - 2.2±0.3 micromol/l, cytokine profile - IL-6 - 103.4±9.2 pg/ml and TNF-α - 15.3±1.7 pg/ml. It should be noted that the above indicators after the usual, traditional intravenous and intramuscular administration of drugs in patients with ACP were significantly worse.This treatment strategy was successfully used in 11 patients with acute cholecystopancreatitis.In 10 (15.0%) cases of the main group, indications for urgent percutaneous drainage interventions were indicated due to the pronounced picture of ACP, there were indications for the imposition of a cholecystostomy under ultrasound control (Fig. 6, 7). | Figure 6. The stages of puncture with drainage of the gallbladder under ultrasound control |
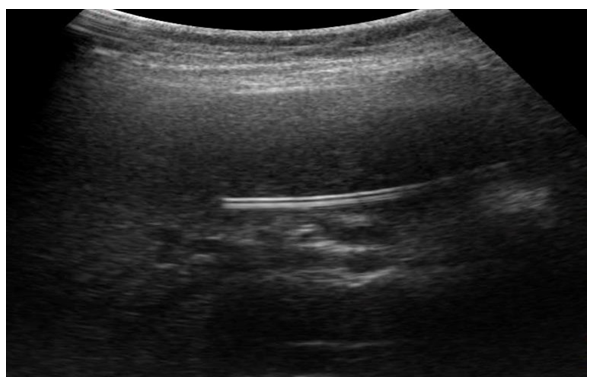 | Figure 7. Ultrasound. Puncture with drainage of the gallbladder under ultrasound control |
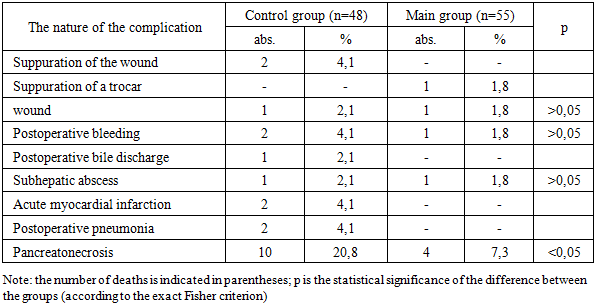
It should be noted that after performing percutaneous drainage interventions on the gallbladder under ultrasound control, there is a noticeable improvement in the general condition of patients against the background of a decrease in endotoxemia.2-3 days after percutaneous drainage procedures on the gallbladder under visual ultrasound control, a decrease in the main indicators of endotoxemia was noted: the LII level averaged 2.39±0.9 units, the MWS values were 654.15±48.3 micrograms/ml, and the average leukocyte level was 6.5±0.4 x109/L.Puncture-draining surgical methods performed under ultrasound control subsequently made it possible to perform radical surgical interventions, i.e. laparoscopic cholecystectomy, after improving the general condition of patients.In patients of the control group, traditional open cholecystectomy and drainage of the subhepatic space were performed in 36 (75%) cases. In 12 (25%) cases, traditional cholecystectomy with open methods, choledocholithotomy, Robson drainage of the common bile duct, and drainage of the subhepatic space were performed.Based on our research, we have developed an algorithm for the diagnosis and surgical treatment of patients with ACP.The essence of the developed algorithm is that the more severe the condition of a patient with ACP, the less he needs to be subjected to surgical aggression. To do this, at the diagnostic stage, along with complaints, medical history, objective and clinical manifestations of the disease, it is necessary to analyze the results of laboratory and instrumental research methods. At the same time, the stages of the diagnostic algorithm should cover such important indicators as the levels of LPO products and cytokine profile. Radiation (ultrasound, CT) and endoscopic (FGDS) research methods play an important role in determining the choice of surgical treatment tactics.Naturally, with uncomplicated forms of ACP, preference should be given to LCE. ACP, accompanied by a picture of choledocholithiasis, taking into account the severity of the patients' condition, is subject to LERV, and in some cases, a two-stage tactic is preferable: EPST + LCE.A special contingent of patients are those at "high" risk, where surgical aggression is fraught with death. In such situations, we strongly recommend minimally invasive decompressive interventions (cholecyst/cholangiostomy) under ultrasound control. After the stabilization of the patients' condition, the second stage is performed by LCE.Table 2 shows an analysis of postoperative complications in the patients we observed.Table 2. Postoperative complications in patients with acute cholecystopancreatitis
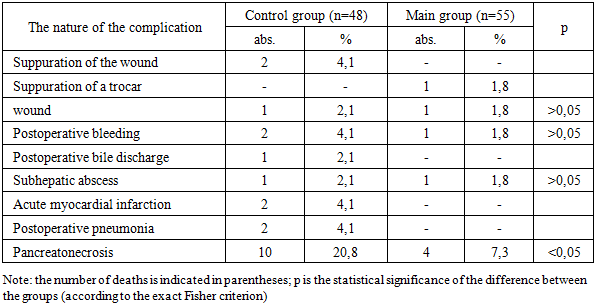 |
| |
|
Among the 48 patients in the control group, 10 (20.8%) patients developed complications after surgery in the immediate postoperative period. At the same time, suppuration of the laparotomy wound occurred in 2 (4.1%) patients, postoperative bile discharge - in 2 (4.1%), bleeding – in 1 (2.1%), subhepatic abscess - in 1 (2.1%), acute myocardial infarction - in 1 (2.1%), postoperative pneumonia – in 2 (4.1%) of patients and 2 (4.1%) more patients developed pancreatic necrosis. Fatal outcome in this group of patients was observed in 1 (4.1%) cases, the causes of which in 1 case was the development of multiple organ failure, in the other case – the development of severe pancreatic necrosis. In the remaining 8 (16.6%) cases, complex conservative treatment proved effective.After performing various surgical interventions in patients of the main group, the development of complications in the immediate postoperative period was observed in 4 (7.3%) cases, while in 1 (1.8%) case, trocar wound suppuration occurred, and in 1 (1.8%) case, postoperative bleeding developed, and in 1 (1.8%) patient, postoperative bile discharge. 1 (1.8%) patient developed an acute myocardial infarction, which caused death.Thus, the results of our study showed that the use of minimally invasive surgical interventions in patients with ACP in combination with developed and improved methods of surgical treatment of acute cholecystopancreatitis, as well as with local administration of drugs through the circular ligament of the liver, help reduce the intensity of inflammatory changes in the pancreatobiliary zone after cholecystectomy, and also increase the effectiveness of preventing the progression of acute pancreatitis.
4. Conclusions
The developed methods of LCE with assisted EPST and LCE with the administration of drugs through the circular ligament of the liver can significantly improve the results of treatment of patients with acute cholecystopancreatitis. Navigation and puncture interventions in acute cholecystopancreatitis in patients with severe somatic status make it possible to stop the destructive process and perform LCE in more favorable conditions. Differentiated surgical tactics using laparoscopic hybrid and puncture-draining minimally invasive technologies in the treatment of acute cholecystopancreatitis reduced the number of postoperative complications from 20.8% to 7.3% and mortality from 4.1% to 1.8%.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
References
| [1] | van Brunschot S., van Grinsven J., van Santvoort H.C., Bakker O.J., Bollen T.L., Boermeester M.A., Besselink M.G., Fockens P., Gooszen H.G. Endoscopic or surgical step-up approach for infected necrotising pancreatitis: a multicentre randomised trial // The Lancet. – 2018. – Vol. 391, № 10115. – P. 51–58. |
| [2] | Trikudanathan G., Tawfik P., Amateau S.K., Munigala S., Arain M., Attam R., Beilman G.J., Freeman M.L., Mallery S., Papachristou G.I. Early (<4 weeks) versus standard (≥4 weeks) endoscopically centered step-up interventions for necrotizing pancreatitis // The American Journal of Gastroenterology. – 2018. – Vol. 113, № 10. – P. 1550–1558. |
| [3] | van Santvoort H.C., Bakker O.J., Bollen T.L., Besselink M.G., Ahmed Ali U., Schrijver A.M., Boermeester M.A., van Goor H., Dejong C.H., van Eijck C.H., van Ramshorst B., Schaapherder A.F., van der Harst E., Hofker H.S., Gooszen H.G. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome // Gastroenterology. – 2011. – Vol. 141, № 4. – P. 1254–1263. |
| [4] | Bang J.Y., Arnoletti J.P., Holt B.A., Sutton B., Hasan M.K., Navaneethan U., Hawes R.H., Varadarajulu S. An endoscopic transluminal approach, compared with minimally invasive surgery, reduces complications and costs for patients with necrotizing pancreatitis // Gastroenterology. – 2019. – Vol. 156, № 4. – P. 1027–1040. |
| [5] | van Dijk S.M., Hallensleben N.D.L., van Santvoort H.C., Fockens P., van Goor H., Bruno M.J., Besselink M.G., Dutch Pancreatitis Study Group. Acute pancreatitis: recent advances through randomised trials // Gut. – 2017. – Vol. 66, № 11. – P. 2024–2032. |
| [6] | Wang X., Cui Z., Li J., Chen Y., Liu Y., Wang C., Wang Y., Zhang Y., Wang X., Li Y. Percutaneous catheter drainage in combination with endoscopic necrosectomy for infected pancreatic necrosis: a single-center experience // World Journal of Gastroenterology. – 2018. – Vol. 24, № 2. – P. 223–232. |





 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML