-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(10): 3389-3393
doi:10.5923/j.ajmms.20251510.23
Received: Sep. 7, 2025; Accepted: Sep. 28, 2025; Published: Oct. 15, 2025

Endoscopic Approach to the Diagnosis and Treatment of Erosive-Ulcerative Infections in the Gastrointestines in Burns
Khaitov Laziz Millionerovich1, Khakimov Erkin Abdikhalilovich1, 2, Mamatov Farrukh Shavkatovich3, Khotamov Ikhtiyor Eshmurotovich4, Davlatov Salim Sulaymonovich5
1Samarkand State Medical University, Samarkand, Uzbekistan
2Samarkand Branch of Republican Scientific Emergency Center
3Head of the Endoscopy Department, Zarmed Pratiksha
4Faculty of General Medicine, Navoi State University
5Bukhara State Medical Institute named after Abu Ali ibn Sino
Correspondence to: Khaitov Laziz Millionerovich, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. According to the latest data from the World Health Organization (WHO), 11-12 million people suffer from burns annually. About half of them, about 6-7 million, require inpatient treatment, more than 200 thousand victims die due to severe complications and consequences of burns. Objective of the study: Assessment of the effectiveness of endoscopic examination and treatment in the early diagnosis, treatment, and prevention of complications of diseases (erosions, ulcers, bleeding, and perforations) with functional and organic changes in the mucous membrane of the gastrointestinal tract with severe burns. Materials and methods. The study included 105 patients with erosions, ulcers, and bleeding complications of the stomach and duodenum, who were treated in the Combustology department of the Samarkand branch of Republican scientific emergency center in the period from 2022 to 2024. Of these, 82.8% were men and 17.2% were women. Research results. Out of 105 patients, 64 patients underwent EGDS once, 20 patients underwent EGDS twice, and 21 patients underwent EGDS 3-5 times. Conclusions and results of single and multiple EGDS. Gastric erosions in 6% patients, duodenal erosions in 8.5% patients, uncomplicated acute and chronic gastric ulcers in 14% patients, duodenal ulcers in 22.1% patients, combined ulcers in 10.4% patients, Complicated bleeding ulcers FIa - 2% patients, Fib - 3.8% patients, FIIa- 4.7% patients, FIIb - 3.8% patients, FIIc - 5.7% patients, FIII - 17.1% patients with the above-mentioned ulcers but without complications, wound perforation in 1.9% patients. Conclusion. Timely use of endoscopic examination and treatment of patients with severe burns led to a decrease in the lowest mortality rate associated with pathologies in the gastrointestinal tract and their severe complications from 38% to 19.2%. The time taken to eliminate complications associated with the gastrointestinal tract was reduced from 3 to 1.5 days in the early period and from 7 to 5 days in the late period.
Keywords: Severe burns, Gastrointestinal tract, EGDS, Erosion, Ulcers, Bleeding, Perforation
Cite this paper: Khaitov Laziz Millionerovich, Khakimov Erkin Abdikhalilovich, Mamatov Farrukh Shavkatovich, Khotamov Ikhtiyor Eshmurotovich, Davlatov Salim Sulaymonovich, Endoscopic Approach to the Diagnosis and Treatment of Erosive-Ulcerative Infections in the Gastrointestines in Burns, American Journal of Medicine and Medical Sciences, Vol. 15 No. 10, 2025, pp. 3389-3393. doi: 10.5923/j.ajmms.20251510.23.
Article Outline
1. Relevance
- According to the latest data from the World Health Organization (WHO), 11-12 million people suffer from burns annually [1,2,3,4]. About half of them, about 6-7 million, require inpatient treatment, more than 200 thousand victims die due to severe complications and consequences of burns [5,6,7]. In Uzbekistan, approximately 12-15 thousand people suffer from burn disease annually [8]. Changes in the gastrointestinal tract in burn disease are directly related to the stage and severity of the disease, and in 3rd-4th degree burns, gastrointestinal dysfunction (perforation, bleeding and septic complications) increases the occurrence, and the combination of these changes worsens the course of the disease, increasing the risk of complications and mortality to 15-25% [9,10,11,12]. Acute lesions and dysfunctional changes in the gastrointestinal tract are detected in 0.2-1.8% of total losses, but in the group of severe burns, these indicators increase by 2.5-3 times. According to endoscopic examination results, acute erosions and ulcers of the gastrointestinal tract in patients with extensive and deep burns are detected in 25-80% of cases, of which 20-25% are complicated by bleeding [13,14,15].Objective of the study: Assessment of the effectiveness of endoscopic examination and treatment in the early diagnosis, treatment, and prevention of complications of diseases (erosions, ulcers, bleeding, and perforations) with functional and organic changes in the mucous membrane of the gastrointestinal tract with severe burns.
2. Materials and Methods
- The study included 105 patients with erosions, ulcers, and bleeding complications of the stomach and duodenum, who were treated in the Combustology department of the Samarkand branch of Republican scientific emergency center in the period from 2022 to 2024. Of these, 87 (82.8%) were men and 18 (17.2%) were women. The age of the patients ranged from 18 to 75 years, the average age was 45 years. Depending on the width and depth of the burn site, it was divided into two groups. In the first group, 72 (68.5%) victims with a frequency of 15-25%, in the second group - 33 (31.4%) victims with a frequency of 30-50%.For endoscopic diagnosis of the gastrointestinal tract and individual assessment of the intensity of bleeding, the classification proposed by J.A. Forrest in 1974 was used (Fig. 1).Ia - pulsating arterial hemorrhageIb - bleeding seeping under a blood clotIIa - visible blood vessel at the bottom of the woundIIb - blood clot firmly attached to the wound bottomIIc - flat hematin at the base of the ulcerIII - absence of signs of bleeding
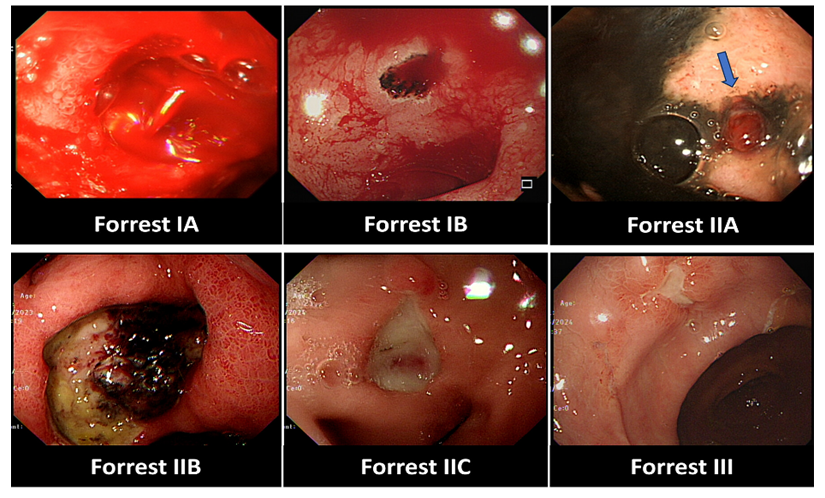 | Figure 1. Forrest classification endoscopic picture of bleeding intensity |
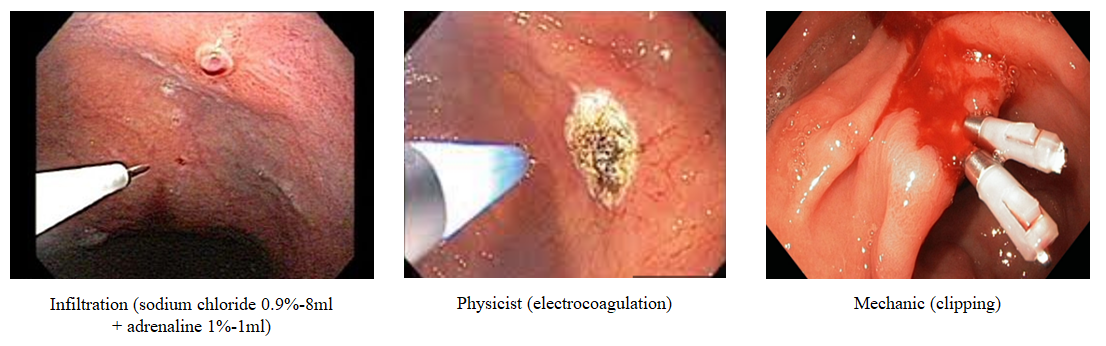 | Figure 2. Types and photo of endoscopic hemostasis |
3. Research Results
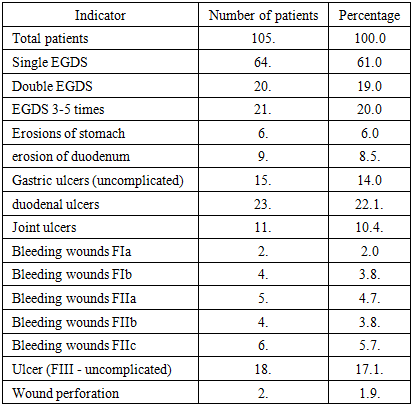
- Out of 105 patients, 64 patients underwent EGDS once, 20 patients underwent EGDS twice (for suspected bleeding and for monitoring in dynamics), and 21 patients (with bleeding complications) underwent EGDS 3-5 times. Conclusions and results of single and multiple EGDS. Gastric erosions in 6 (6%) patients, duodenal erosions in 9 (8.5%) patients, uncomplicated acute and chronic gastric ulcers in 15 (14%) patients, duodenal ulcers in 23 (22.1%) patients, combined ulcers in 11 (10.4%) patients, Complicated bleeding ulcers FIa-2 (2%) patients, FIb-4 (3.8%) patients, FIIa-5 (4.7%) patients, FIIb-4 (3.8%) patients, FIIc-6 (5.7%) patients, FIII - 18 (17.1%) patients with the above-mentioned ulcers but without complications, wound perforation in 2 (1.9%) patients (Table 1).
|
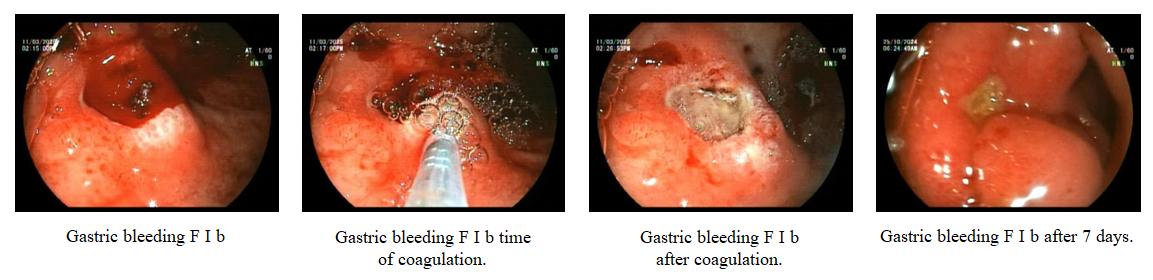 | Figure 3. Image and effect of endoscopic hemostasis |
4. Discussion of Results
- Diseases (erosions and ulcers, perforations) of the gastrointestinal tract in patients with severe burns, accompanied by organic changes in the mucous membrane, are one of the urgent and complex problems of medicine, and acute gastroduodenal erosions and ulcers are etiopathogenetically associated with the use of ulcerative drugs and psycho-emotional stress observed in burn disease. Disruption of local blood circulation contributes to the development of hypoxia and reduces the resistance of the gastroduodenal mucosa to acid-peptic aggression. In the last decade, acute gastroduodenal erosions and ulcers have become the leading cause of gastrointestinal bleeding in patients with severe burns [3-6]. Prophylactic EGDS, continuous prophylactic use of gastric secretion blockers, antacids, and cytoprotective agents are used from the first hours after the patient's admission.The results of the study show that in the acute period of burn disease, effective elimination of hemodynamic disorders, fluid and protein balance reduces the risk of dysproteinemia and intoxication, which leads to trophic disorders of the gastrointestinal tract wall. It is very important to ensure adequate perfusion of organs to prevent the development of acute ulcers and bleeding [4-5].Our studies have shown that the endoscopic approach in the early prevention and treatment of complications (acute gastroduodenal erosions and ulcers, bleeding, perforation) that develop in patients in the early period within the first 24-48 hours and in the late 3-5 days allows in 70-80% of cases to prevent severe complications associated with the gastrointestinal tract and reduce the number of deaths [10-12]. Using new endoscopic diagnostic and treatment techniques in patients with gastrointestinal dysfunction (acute gastroduodenal erosions and ulcers, bleeding, perforation), especially when active bleeding is detected, allows for immediate endoscopic hemostasis to achieve 90-95% positive results and effectiveness. As a result, the lowest mortality rate associated with this complication decreased from 38% to 19.2%. A positive result was achieved by reducing the time taken to eliminate these complications from 3 to 1.5 days in the early period and from 7 to 5 days in the late period (fig 4).
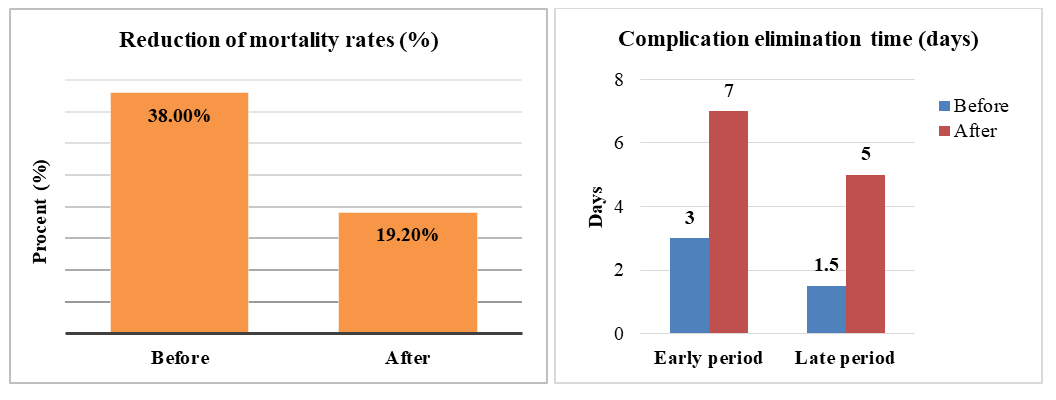 | Figure 4. Effectiveness of the endoscopic approach in the elimination of pathologies in the gastrointestinal tract |
5. Conclusions
- 1. The endoscopic approach plays an important role in the early prevention, treatment, and prevention of severe complications of pathologies in the gastrointestinal tract in patients with severe burns.2. Timely use of endoscopic examination and treatment of patients with severe burns led to a decrease in the lowest mortality rate associated with pathologies in the gastrointestinal tract and their severe complications from 38% to 19.2%.3. The time taken to eliminate complications associated with the gastrointestinal tract was reduced from 3 to 1.5 days in the early period and from 7 to 5 days in the late period.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML