Iskandarov Yusuf Nazimovich, Abdurahmanov Diyor Shukurullayevich
Samarkand State Medical University, Uzbekistan
Correspondence to: Abdurahmanov Diyor Shukurullayevich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Relevance of the problem. Lumbar and lateral abdominal hernias remain a relatively rare but extremely clinically significant pathology, especially in the context of their occurrence after urological interventions such as nephrectomy, ureterolithotomy, cystectomy and reconstructive interventions. The aim of the study is to develop and substantiate the clinical effectiveness of separation hernioalloplasty for postoperative lumbar and lateral abdominal hernias. Material and methods of the study. This work is based on the analysis of a comprehensive examination and surgical treatment of 102 patients with PAH and POLH hernias who were treated in the surgical and urological departments of the multidisciplinary clinic of the Samarkand State Medical University from 2019 to 2024. Of these, 68 (66.6%) patients had PAH, and 34 (33.3%) had POLH. Results and their discussion. To select the method and volume of surgery for POL and POAH abdominal hernias, we followed a differentiated surgical tactic, which was based on objective data and the results of instrumental research methods. According to the objective criteria given, various volumes of POL and POAH hernias were performed and the nature of surgical interventions. Conclusions. Selection of the method and technique of hernioplasty in case of postoperative lateral and lumbar hernias it should be carried out on the basis of developed objective criteria. The use of tension-free separation hernioalloplasty made it possible to reduce the frequency of postoperative complications from 27.7% to 8.9%, and the frequency of relapse from 16.6% to 2.1%.
Keywords:
Postoperative lumbar and postoperative anterolateral abdominal hernias, Endoprosthetics, Separation plastic surgery
Cite this paper: Iskandarov Yusuf Nazimovich, Abdurahmanov Diyor Shukurullayevich, Rationale for Separation Hernialloplasty in Postoperative Lumbar and Anter-Lateral Abdominal Hernias, American Journal of Medicine and Medical Sciences, Vol. 15 No. 10, 2025, pp. 3365-3371. doi: 10.5923/j.ajmms.20251510.18.
1. Relevance of the Problem
Lumbar and lateral abdominal hernias remain a relatively rare but extremely clinically significant pathology, especially in the context of their occurrence after urological interventions such as nephrectomy, ureterolithotomy, cystectomy and reconstructive interventions. Despite the low prevalence, their treatment causes significant difficulties due to the anatomical localization of the defect, the disrupted muscular-aponeurotic framework and the high probability of recurrence [1,2,3,4].Modern approaches to surgical treatment of lumbar and lateral hernias include both traditional (onlay, sublay) and laparoscopic and robot- assisted techniques using mesh implants. However, despite advances in hernioplasty, the recurrence rate remains high - up to 20-35%, especially with significant defects and the presence of concomitant risk factors such as obesity, chronic cough, severe muscle atrophy and infection of the postoperative wound [5,6,7,8].An analysis of international literature shows that the issues of preventing such hernias are at the intersection of urological and herniological surgery. Preventive measures, including a rational choice of surgical approach, minimization of intraoperative trauma to muscular-aponeurotic structures, as well as early physical rehabilitation and planned reconstruction of the posterior abdominal wall, are just beginning to be developed. In recent years, some researchers (e.g., MS Patel, 2018; C. Fortes, 2021) have focused on the introduction of preventive mesh plastic surgery at high risk of hernia formation [9,10,11].The problem is presented in limited terms in the literature. There are isolated clinical observations and case series, mainly describing complicated forms after nephrectomies with lateral access. There is no unified classification of such hernias, which complicates the standardization of approaches to their treatment and prevention. In addition, clear algorithms for choosing a method of plastic surgery depending on the size of the defect, muscle dysfunction and anatomical type of hernia have not yet been formulated.The aim of the study is to develop and substantiate the clinical effectiveness of separation hernioalloplasty for postoperative lumbar and lateral abdominal hernias.
2. Material and Methods of the Study
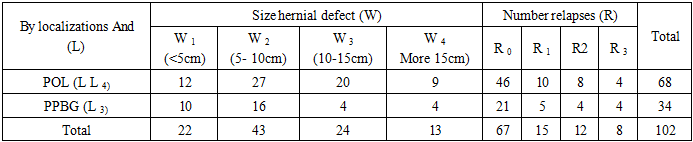
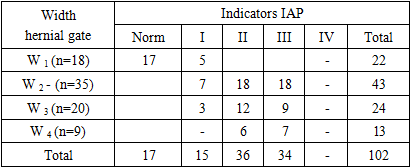
This work is based on the analysis of a comprehensive examination and surgical treatment of 102 patients with postoperative anterolateral hernia (PAH) and postoperative lumbar hernia (POLH) who were treated in the surgical and urological departments of the multidisciplinary clinic of the Samarkand State Medical University from 2019 to 2024. Of these, 68 (66.6%) patients had PAH, and 34 (33.3%) had POLH.There were 62 (60.8%) female patients suffering from PAH and PAHB, and 40 (39.2%) male patients. In 83 (81.4%) observations, patients were in the most mature working age (from 18 to 60 years). Patients with PAH and PAH hernias were classified according to the classification JPChevrel and AMRat (Table 1).Table 1. Distribution of patients according to the JPChevrel and AMRat classification
 |
| |
|
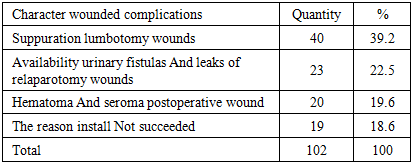
Thus, the sizes of the hernial orifices in patients with PAH were as follows: W1 (up to 5 cm) in 12 (17.6%), W2-(5-10 cm) – in 27 (39.7%), W3- (10-15 cm) – in 20 (29.4%) and W4-(more than 15 cm) – 9 (13.2%). At the same time, the number of relapses of this contingent of patients was as follows: there were no relapses of the disease in 46 (67.6%) patients, R1 – in 10 (14.7%), R2- in 8 (11.7%) and R3- in 4 (5.9%).In patients with PPBG hernias, the hernial defect sizes were W1– in 10 (29.4%), W2– in 16 (47.1%), W3– in 4 (11.7%), and W4– in 4 (11.7%). The number of disease recurrences was absent in 21 (61.7%), R1– in 5 (14.7%), R2– in 4 (11.7%), and R3– in another 4 (11.7%). In general, in both groups of patients with PAH (LL4) and PAHB (L3), the sizes of the hernial orifices were as follows: W1 - (up to 5 cm) in 22 (21.5%), W2- (5-10 cm) - in 43 (42.1%), W3- (10-15 cm) - in 24 (23.5%) and W4- (more than 15 cm) in 13 (12.7%) patients. By the number of relapses: there were no relapses of R0- in 67 (65.7%), R1- in 15 (14.7%), R2- e 12 (11.7 %) and R4- in 8 (7.8%).All patients with postoperative lumbar (POL) and postoperative anterolateral abdominal hernias (POAAH) had previously undergone surgery for surgical diseases of the kidneys and ureter. In 75 (73.5%) cases, surgical interventions were are given in the presence of stones in various parts of the kidneys and ureter; in 27 (26.5%), surgical interventions were performed due to purulent-septic diseases.Of lumbotomy accesses was noted in 40 (39.2%) cases after urological interventions, urinary wound fistulas and leaks were noted in 23 (22.5%), hematomas and seromas of wounds were noted in 20 (19.6%), and the cause of the development of PAH and POAAH hernias could not be determined from the medical documentation provided in 19 (18.6%) cases.Table 2. The nature of previously suffered wound complications in patients with POL and PPBG (n=102)
 |
| |
|
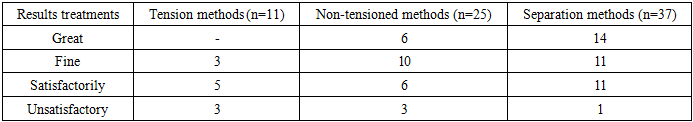
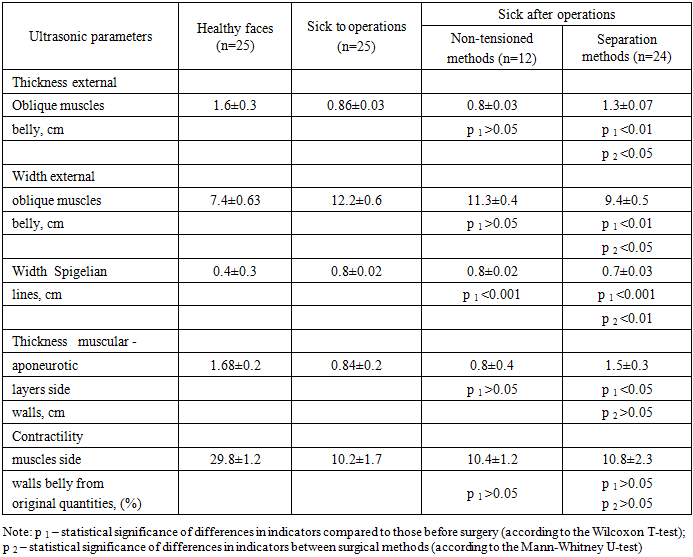
In the studies conducted, the clinical manifestation POL and PPB hernias were characterized by complaints about the presence of a tumor-like formation of the lumbar (n=68) And anterior -lateral areas (n=34) belly With trend to a gradual increase in its size (Fig. 1, 2).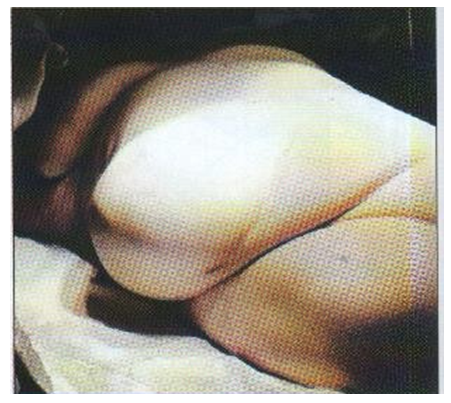 | Figure 1. Postoperative lumbar hernia after lumbotomy (W3 –W4) |
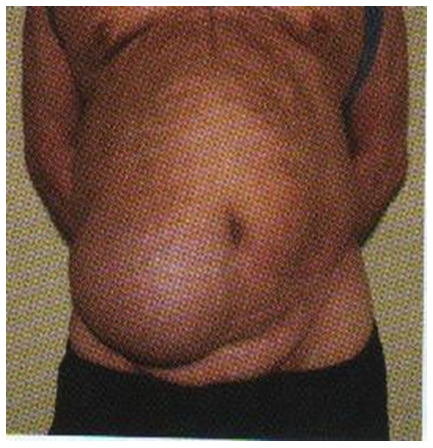 | Figure 2. Postoperative anterolateral hernia after surgery on the ureter |
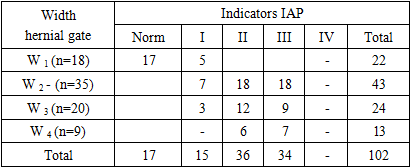
In 58 (56.8%) observations, patients with POL and POAH hernias complained of the presence of a protrusion and the appearance of pain, and 21 (20.6%) patients worried sharp thinning skin V areas hernial protrusion. In 3 (2.9%) observations, patients were concerned about the presence of trophic ulcers in the area of an extensive lateral hernia.For forecasting possible development of early postoperative complications All patients underwent measurement IAP. Assessment indicators The IAP was carried out depending on the size of the hernial orifice (Table 3).Table 3. Indicators of IAP depending on the width of the hernial orifice (n=102)
 |
| |
|
Thus, in postoperative hernias of the I degree in 5 patients W 1, W 2 -7, W 3 -3. Then, how By measure increases widths hernial gate and the duration of hernia in 36 (35.2%) patients, grade II hernia occurred, in 34 (33.3%) intra-abdominal pressure (IAP) IAP- III degree. Complex Ultrasound examination of patients with PAH and PAHB was performed in 67 (65.6%) observations in order to identify the degree of severity of the shape of the hernial orifice, hernial contents, and also to select the most pathogenetically justified method of hernioplasty. (Fig. 3-4). | Figure 3. Ultrasonography in POL. In the lumen of the hernial sac there are loops of small intestine |
 | Figure 4. Ultrasonography in POL. Thinning of the thickness of the external oblique abdominal muscle |
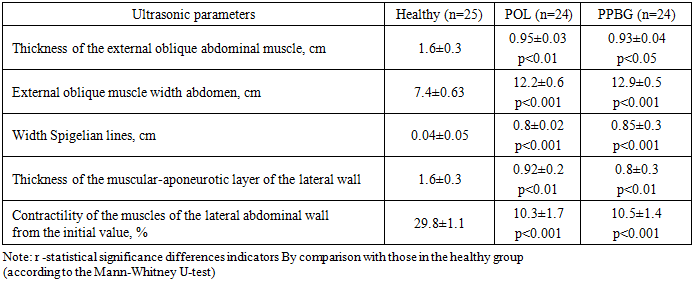
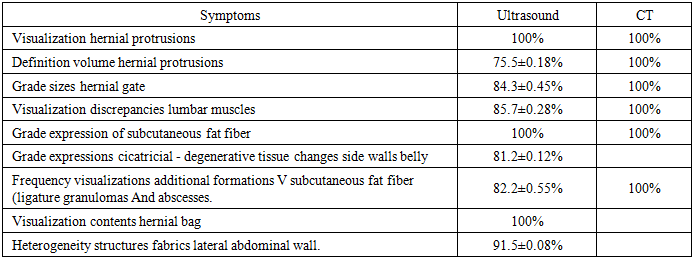
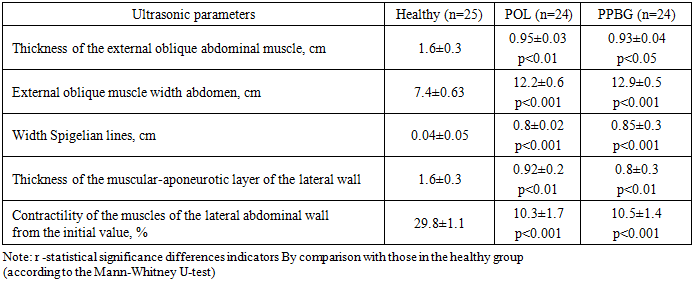
To identify anatomical and functional insufficiency of the lateral abdominal walls, ultrasound and CT were performed before the operation. The results of ultrasound examination of the abdominal wall condition in The numbers of patients with POL and postoperative anterolateral hernia (POAH) are presented in table 4.Table 4. Ultrasound characteristics of the anatomical and functional state of the lateral walls belly at POL and PPBG (M±m)
 |
| |
|
Among patients with small hernias share having degenerative the changes were 33.1%, with average -53%, with large ones - 92%, with giant ones -100%.Atrophic changes of varying severity were detected in all 48 patients examined by ultrasound. It should be noted that with short terms of hernia carriage, and also its small size during ultrasound revealed a weak degree atrophy muscle tissue (n=9) - 18.7%, moderate atrophy - in 27 (56.2%) and severe - in 12 (25%) patients.Among the radiation methods for diagnosing POL and POAAH, a special place is occupied by complex computed tomography (CT) performed according to indications 13 patients with PAH (n=8) and POLH (n=5). In CT of the lumbar region, abdominal wall, this contingent of patients, changes depending, as a rule, on the localization of the hernia, its size, the contents of the hernial sac.For a comparative study of the information content of ultrasound and CT in the diagnosis of features anatomical and functional To determine the structure of the lumbar and anterolateral abdominal wall around the hernial protrusion, as well as to determine the size of the hernial protrusion and hernial orifice in patients with PAH and PAH, an analysis of the study results was conducted in 48 patients (table 5).Table 5. Comparative analysis of ultrasound and CT data in assessing changes in the lateral abdominal wall in patients with postoperative lumbar and lateral hernias (in%)
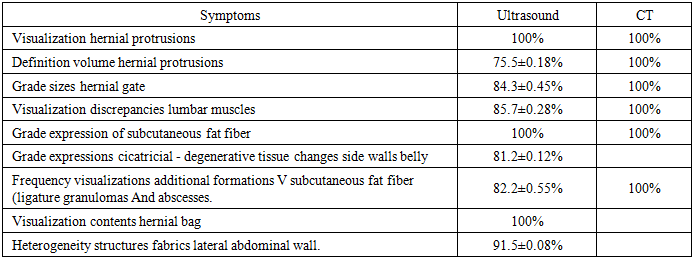 |
| |
|
Thus, anatomical and functional insufficiency side wall belly I-II degrees at sick With urological diseases, and also the presence postoperative specific wound complications (urinary leaks, fistulas) are the cause of the development of postoperative lumbar and lateral hernias.
3. Results and Their Discussion
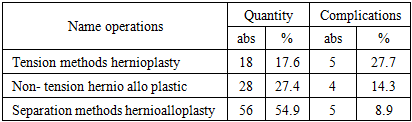
To select the method and volume of surgery for POL and POAH abdominal hernias, we followed a differentiated surgical tactic, which was based on objective data and the results of instrumental research methods.According to the objective criteria given, various volumes of POL and POAH hernias were performed and the nature of surgical interventions (Table 6).Table 6. The nature of surgical interventions for PAH and POAAH hernias (n=102)
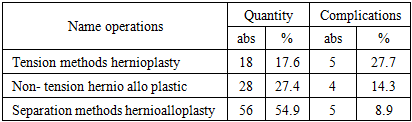 |
| |
|
As can be seen from the table presented, the separation method of hernioplasty was most frequently performed in 56 (54.9%) cases, non-tension methods in 28 (27.4%) and tension methods of hernioplasty in 18 (17.6%) cases. In the postoperative period, after tension methods of hernioplasty, complications occurred in 27.7% (n = 5) cases, whereas after " non-tension " and combined methods of hernioplasty, they amounted to 14.3% (n = 4) and 8.9 % (n = 5).According to the proposed separation method of hernioplasty, recovery integrity of the muscular- aponeurotic layer of the lateral abdominal wall, elimination of deformation and asymmetry of the abdomen due to the use of endoprostheses “Vipro Ethocon” and “Esfil” Lintex. Polypropylene mesh endoprosthesis were placed and fixed into one formed retromuscular space between the outer and inner oblique muscles - from the Spigelian line to the lumbar muscles and from the lower edge of the costal arch to the iliac crest According to the “ tension - free ” principle, insufficient space was necessarily drained.After excision of the old postoperative scar bordering cuts layer by layer separated external and the internal oblique muscles, as well as the transverse muscle and fascia (Fig. 5, 6).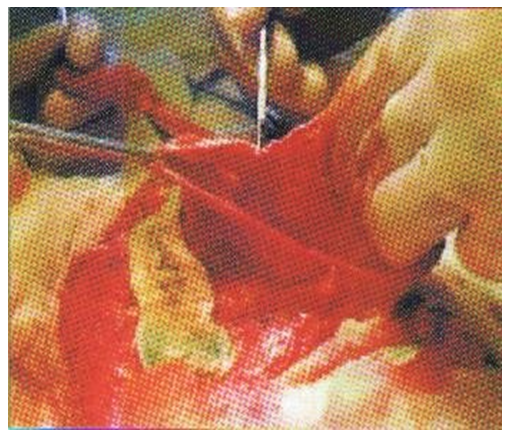 | Figure 5. Separation external and internal oblique muscles, as well as the transverse muscle and fascia |
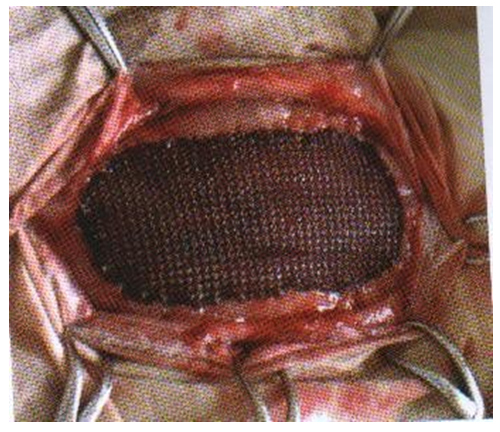 | Figure 6. Fixation of the endoprosthesis |
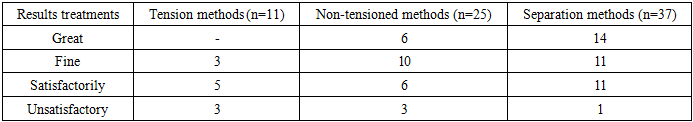
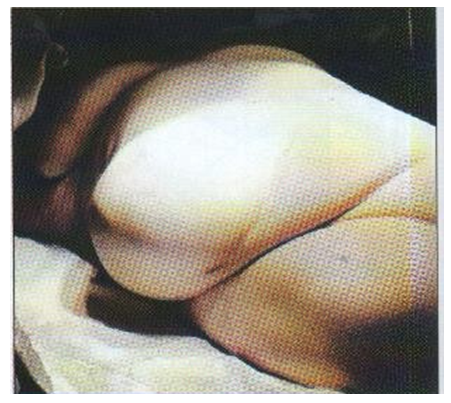
Necessary separate and highlight interfacial lateral structures abdominal walls within the entire anatomical region, from the lower edge of the costal arch to the iliac crest bones and from the Spigelian line (pararectal) line to the longitudinal muscles of the back and lumbar muscles. This stage was carried out carefully, without allowing excessive damage to the agrophilic and flabby muscles of the lateral abdominal wall. After this The hernial sac was submerged, and the transverse fascia and muscles, as well as the internal oblique muscle above the hernial sac, were sutured.These anatomical structures were sutured along their entire length without tension. A flat area was formed so as to achieve the elimination of the existing deformation and asymmetry of the abdomen by adequately matching the interfacial layers of the lateral region with each other, as well as uniform invagination, application or displacement and matching of muscle bundles with each other, if necessary. Then, a polypropylene was placed and fixed over the internal oblique muscle of the abdomen endoprosthesis: from the lower edge costal arch to the iliac crest and from the Spigelian line to the longitudinal muscles of the back and lumbar muscles.The prosthesis was fixed with a polypropylene thread continuously or with interrupted sutures, stepping back from each of its edges by 4-5 cm. supra-reticular space drained with silicone perforated with a pipe within 5 days. After which the external oblique muscle was sutured.In patients after separation techniques, serous-hemorrhagic fluid was released from surgical wounds during the first 5-6 days, and then serous fluid within 7-10 days. In the group of patients who underwent tension-free hernioplasty techniques, the volume of fluid released from the wound ranged from 26.5 ± 1.2 ml in the first day before 5.2±1.3 ml on the tenth day, and in the group of patients operated by a combined method, respectively, from 25.3±2.1 ml up to 3.6±1.2 ml. The peak value of the exudative reaction occurred on the third day of the postoperative period, when in patients with " non-tension " hernioplasty the amount of secreted fluid was 56.7±4.3 ml, and in the group of patients with combined hernioplasty - 45.5±4.2 ml. The conducted study of the course of the inflammatory reaction in response to the implantation of prostheses did not reveal significant differences.In the immediate postoperative period after performing tension methods of hernioplasty, postoperative complications were noted in 5 (27.7%) observations. In 4 cases, wound complications were noted in the form of: suppuration (n=2), seroma (n=1) and hematoma (n=1). Only In one observation, postoperative pneumonia was diagnosed. Complex conservative therapy with the use of antibacterial agents allowed this patient to be treated. In the presence of postoperative wound complications, local treatment was performed using 2-3-4 punctures under ultrasound control.In the group of patients who underwent tension-free hernioplasty techniques (4; 14.3%), the presence of seroma was diagnosed in 2 observations using ultrasound. The presence infiltrate at 1 And at 1 suppuration wounds.After performing the separation technique of hernioalloplasty, postoperative wound complications were diagnosed in 5 (8.9%) patients. In 5 observations, the presence of hematoma (n=2) and seroma (n=2) and infiltrates were diagnosed by ultrasound (n=1).Remote results over a period of 1 to 6 years were studied in 73 patients out of 102. At the same time, 11 (15.1%) patients had previously undergone tension methods of hernioplasty, 25 (34.2%) non-tension and (37 50.7%) separation methods (Table 7).Table 7. Indicators of remote results of surgical treatment of postoperative lumbar and lateral hernias (n=73)
 |
| |
|
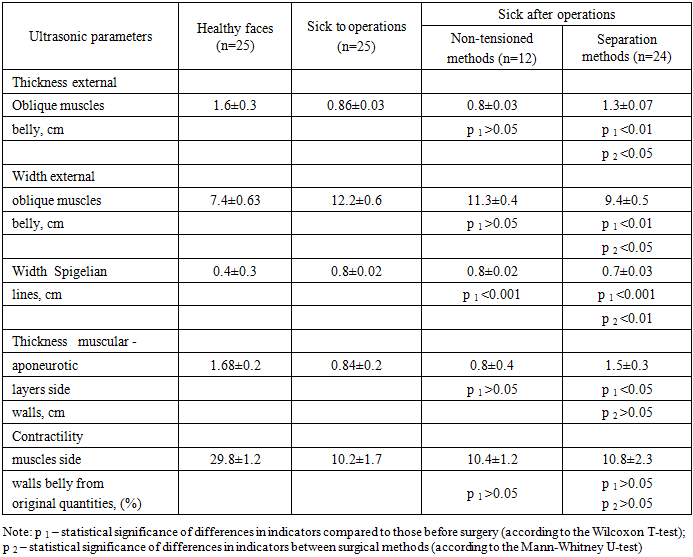
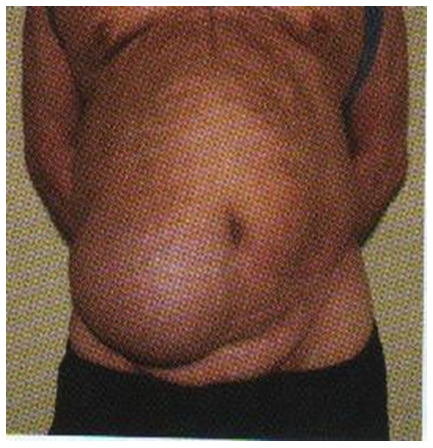
When assessing long-term results, great importance was attached to the results of ultrasound examination concerning the anatomical and functional state of the muscles of the lateral wall (Table 8).Table 8. Ultrasound characteristics of the anatomical and functional state of the lateral abdominal wall before and after surgery (M±m)
 |
| |
|
In the long term after tension and non-tension methods, negative dynamics of ultrasound indicators were noted. side wall abdomen. The amount has increased connective tissue layers in the subcutaneous fat fiber, the width and thickness of the external oblique muscle amounted to 11.3 ±0.3 cm And 0.9±0.2 cm respectively, A thickness muscle layer was 0.92±0.3 cm. Defects in the muscular-aponeurotic layer were noted in 7 patients against the background of sharp decreased contractility of the lateral abdominal wall (11.3±1.1%).In patients operated using the separation method, the following was observed: tangible positive dynamics. Thus, the width of the Spigel line is 0.04±0.03 cm reached 0.7±0.02 cm, the width of the external oblique The abdominal muscles were 9.4±0.4 cm, and the thickness was 1.5±0.2 cm. No defects were found in the muscular-aponeurotic layer.Excellent and good results after separation hernioplasty were noted in 25 (67.5%) of 37 patients examined, after non-tensioned – in 16 (64%) and after tensioned – in 3 (27.3%) patients. Satisfactory results were recorded in 11 patients after separation hernioplasty, in 6 after non-tensioned hernioplasty and in 5 after tension methods. Unsatisfactory long-term results were found in 7 patients after tension (n=3) and non-tension (n=3) methods and in 1 observation after separation hernioplasty.Thus, the analysis of the results of surgical treatment of POL and POAHG showed that after performing the separation technique of hernioalloplasty immediate and remote results significantly better compared to tension-free and tension methods of hernioplasty.
4. Conclusions
1. The causes of occurrence and development of postoperative lumbar and lateral abdominal hernias after urological interventions are the implementation of extended and traumatic approaches with intersection of muscles and vascular -nerve formations, local purulent-inflammatory complications, as well as insufficiency lateral abdominal wall and associated metabolic diseases.2. Developed by And improved methods of intraoperative ultrasound diagnostics of anatomical and functional insufficiency side walls belly with preventive endoprosthetics allow to reduce the frequency of formation of postoperative hernias and their recurrence.3. Selection of the method and technique of hernioplasty in case of postoperative lateral and lumbar hernias it should be carried out on the basis of developed objective criteria. The use of tension-free separation hernioalloplasty made it possible to reduce the frequency of postoperative complications from 27.7% to 8.9%, and the frequency of relapse from 16.6% to 2.1%.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
References
| [1] | Szczęsny W., Kaska Ł., et al. "Surgical treatment of incisional hernias: Techniques and outcomes." Hernia Journal. 2021; 25(3): 345–354. |
| [2] | Davlatov S, Navruzov R, Sanoyeva M, Xudoykulov D, Gaziev K. Case of laparoscopic treatment recurrent obturator hernia. InBIO Web of Conferences 2024 (Vol. 121, p. 04003). EDP Sciences. DOI: 10.1051/bioconf/202412104003. |
| [3] | Abduraxmanov DS, Kurbaniyazov ZB, Davlatov SS, Rakhmanov KE. Criteria for choosing surgical treatment of patients with ventral hernias and obesity. International Journal of Pharmaceutical Research (09752366). 2020 Jul 1; 12(3). DOI: 10.31838/ijpr/2021.13.01.598. |
| [4] | Deerenberg E. B., Timmermans L., et al. "Small bites versus large bites for closure of abdominal midline incisions (STITCH): A double-blind, multicentre, randomised controlled trial." Lancet. 2015; 386(10000): 1254–1260. |
| [5] | Mardanov B, Kurbaniyazov Z, Davlatov S, Rakhmanov K. Rationale for Simultaneous Operations on The Abdominal Organs and The Abdominal Wall in Patients with A Ventral Hernia. International Journal of Pharmaceutical Research (09752366). 2020 Jul 2. DOI: 10.31838/ijpr/2020.SP2.339. |
| [6] | Gurusamy K. S., Vaughan J., et al. "Mesh versus suture repair for incisional hernias." Cochrane Database of Systematic Reviews. 2022; (3): CD007781. |
| [7] | Сайінаєв Ф, Курбаніязов З, Рахманов К, Давлатов С, Усаров Ш. Innovations in laparoscopic hernioplasty of ventral hernias. Неонатологія, хірургія та перинатальна медицина. 2025 Jul 16; 15(2 (56)): 103-7. DOI: https://doi.org/10.24061/2413-4260.XV.2.56.2025.14. |
| [8] | Sauerland S., Walgenbach M., et al. "Laparoscopic versus open surgical techniques for ventral or incisional hernia repair." Cochrane Database of Systematic Reviews. 2020; (10): CD007781. |
| [9] | Palladino E., Turra F., et al. "Postoperative complications after mesh-based abdominal wall hernia repair." Annals of Surgery. 2020; 271(5): 862–869. |
| [10] | Carbonell A. M., Warren J. A., et al. "Trends in incisional hernia repair: Emerging techniques and patient outcomes." Surgical Clinics of North America. 2022; 102(5): 901–915. |
| [11] | Kurbanyazov Z, Yuldashov P, Rakhmanov K, Davlatov S, Khamdamov B, Yanchenko S. Enhancement of Surgical Treatment Methods for Postoperative Ventral Hernia: Experience of Laparoscopic Prosthetic Hernioplasty. "Surgery Eastern Europe", 2025, volume 14, No. 2, 268 - 277. DOI: https://doi.org/10.34883/PI.2025.14.2.027. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML