Khashimov Rustam Uktamjanovich1, Rizayev Jasur Alimdjanovich1, Rakhmanov Kosim Erdanovich1, Davlatov Salim Sulaymonovich2
1Samarkand State Medical University, Uzbekistan
2Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan
Correspondence to: Rakhmanov Kosim Erdanovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Relevance. Inguinal hernias remain one of the most common pathologies requiring surgical intervention, which determines the high social and economic significance of this problem in modern clinical practice. The purpose of this study is to increase the effectiveness of surgical treatment of patients with inguinal hernias by improving the technical aspects of hernioalloplasty. Research materials. 303 patients with inguinal hernias were selected for a prospective dynamic active study. The first group, the comparison group, consisted of 126 (41.6%) patients with inguinal hernias, the second, the main group consisted of 177 (58.4%) patients. Research results. In the main group, the overall incidence of wound complications was 6.2%, while in the comparison group, this indicator reached 19.8%. Of the 234 patients examined in the long term, recurrence of inguinal hernia was registered in 10 (4.3%) patients. In the comparison group, the recurrence rate was 9.8% (9 patients), while in the main group it was only 1.7% (1 patient). In the comparison group of patients who underwent Lichtenstein surgery, testicular atrophy (in 3 cases) and impaired reproductive function (in 4 cases) were noted in 7 (7.6%) cases. Conclusions. Based on the data obtained and clinical experience, the developed and proposed algorithm of surgical treatment of inguinal hernias makes it possible to optimize the choice of hernioplasty method depending on the clinical situation and individual characteristics of the patient. The implementation of this algorithm contributes to improving the quality of medical care, reducing the incidence of complications and relapses, as well as increasing patient satisfaction with treatment results.
Keywords:
Inguinal hernia, Hernioplasty, Complication, Relapse
Cite this paper: Khashimov Rustam Uktamjanovich, Rizayev Jasur Alimdjanovich, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich, Development of an Algorithm for Surgical Treatment of Inguinal Hernias Based on a Comparative Analysis of Modern and Traditional Hernioplasty Techniques, American Journal of Medicine and Medical Sciences, Vol. 15 No. 10, 2025, pp. 3358-3364. doi: 10.5923/j.ajmms.20251510.17.
1. Relevance
Inguinal hernias remain one of the most common pathologies requiring surgical intervention, which determines the high social and economic importance of this problem in modern clinical practice. Despite the many hernioplasty techniques developed, the issues of optimizing the choice of surgical tactics remain relevant due to the variety of clinical manifestations, anatomical and physiological characteristics of patients and possible postoperative complications [6,9,11,13]. Traditional hernioplasty methods, despite their proven effectiveness, are associated with a number of limitations, including a long recovery period, the risk of relapses and complications affecting the reproductive function of men [3,5,12,15].In recent years, considerable attention has been paid to the introduction of modified and minimally invasive endovideosurgical techniques, which demonstrate advantages in reducing postoperative traumatism and improving the quality of life of patients. However, choosing the optimal treatment strategy requires an integrated approach and in-depth analysis of the results of using various techniques in clinical practice [1,7,10,14].The development of a sound algorithm for the surgical treatment of inguinal hernias, based on a comparative analysis of modern and traditional hernioplasty methods, is an important step towards standardizing the treatment process, reducing the incidence of complications and relapses, and improving the overall effectiveness of surgical intervention [2,4,8,16]. The present study is aimed at solving this problem and is of high practical importance for specialists in the field of surgery and urology.The purpose of this study is to increase the effectiveness of surgical treatment of patients with inguinal hernias by improving the technical aspects of hernioalloplasty.
2. Research Materials
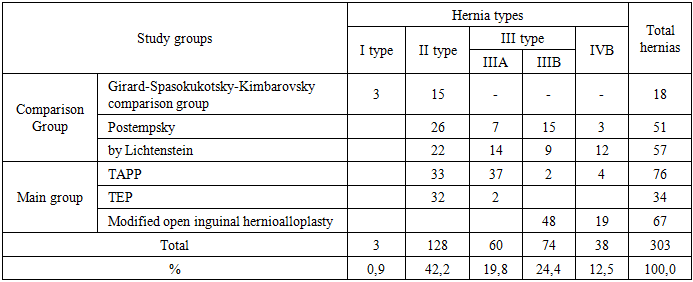
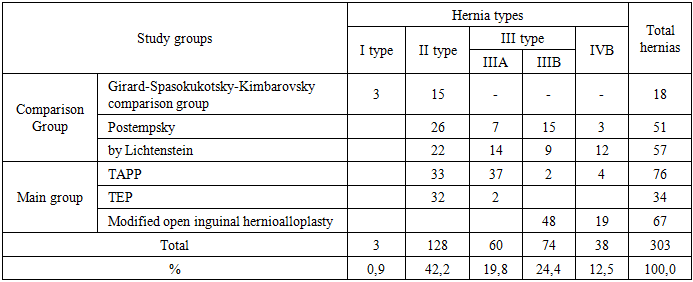
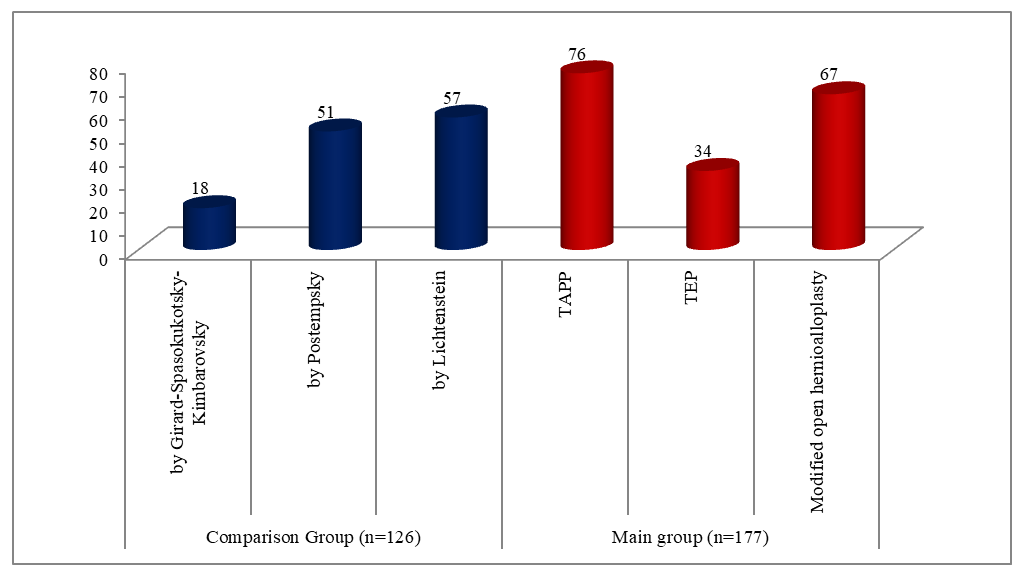
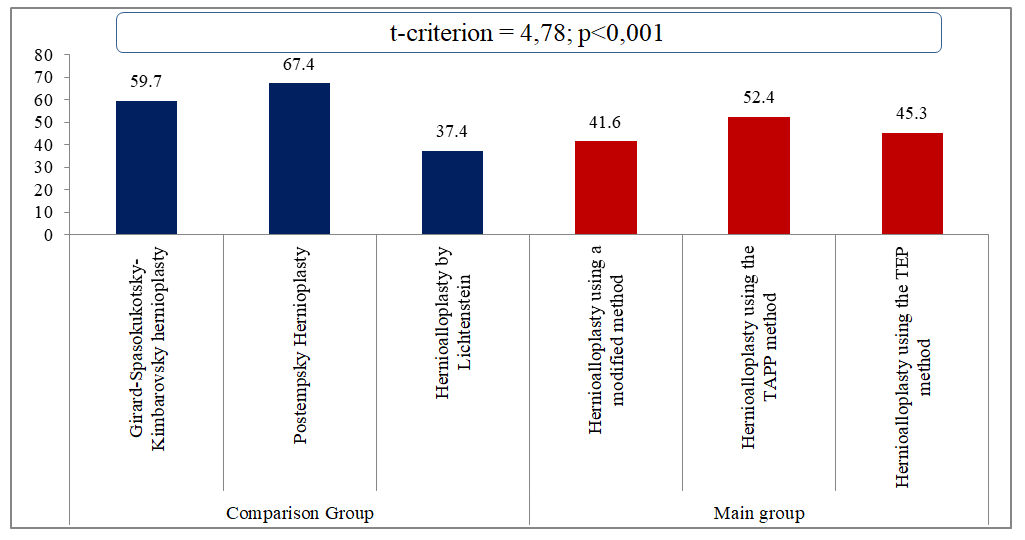
The study is based on the results of examination and treatment of patients with inguinal hernias who underwent surgery in the surgical department of the multidisciplinary clinic of Samarkand State Medical University in the period from 2016 to 2025. 303 patients with inguinal hernias were selected for a prospective dynamic active study. These were male patients with inguinal hernias of various types.The patients were operated on both as planned and as an emergency, and depending on the choice of treatment tactics, the patients were divided into two groups (Fig. 1).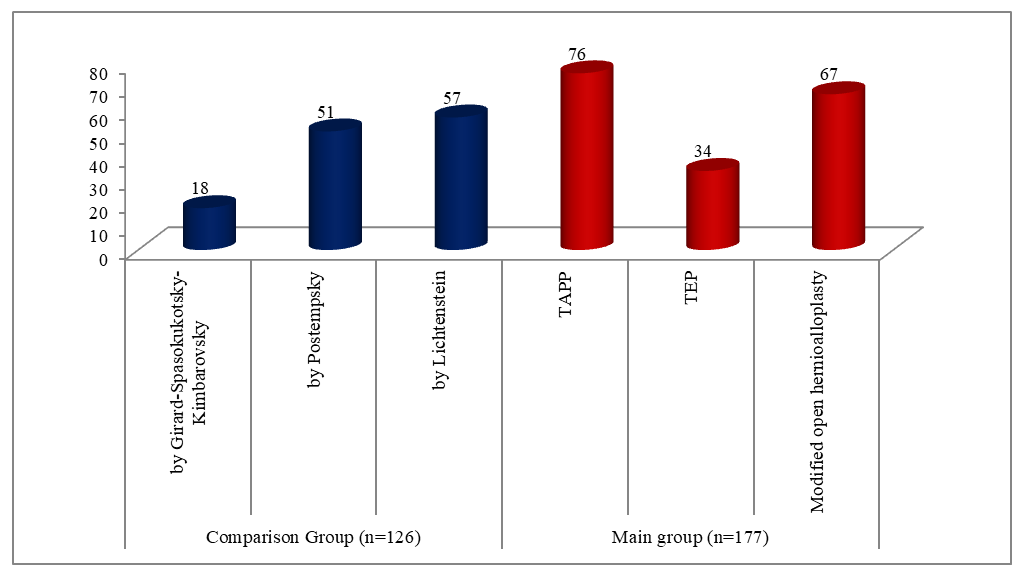 | Figure 1. Distribution of patients by study groups (n=303) |
The comparison group included 126 patients (41.6%) with inguinal hernias who underwent hernioplasty using traditional surgical methods. The main group consisted of 177 patients (58.4%) who underwent open hernioalloplasty using our modified technique and underwent hernioalloplasty using endovideosurgical techniques.According to the types of hernias (L.M. Nyhus classification), the distribution in groups is shown in Table 1. The total number of oblique inguinal hernias was 243 cases, which corresponds to 80.2% of the total number of observations. Type III A hernias (direct inguinal hernias) were reported in 60 patients (19.8%). Recurrent inguinal hernias were detected in 38 cases, which is 12.5% of the total sample. According to the results of the statistical analysis, the distribution of hernia types in both groups had no statistically significant differences (χ2-test, p > 0.05), which allows us to consider the studied groups homogeneous in this parameter.Table 1. Distribution of inguinal hernias according to the classification of L. M. Nyhus hernias
 |
| |
|
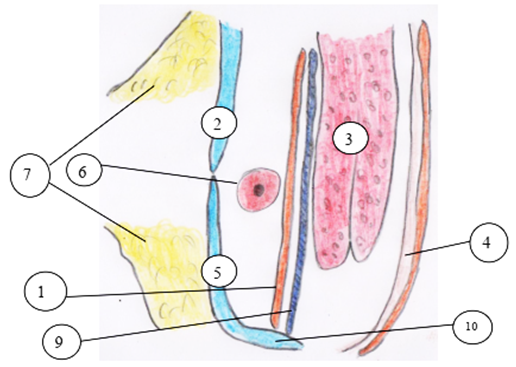
In order to minimize the likelihood of adverse outcomes in the postoperative period after open inguinal hernioalloplasty, which was observed in patients in the comparison group, 67 patients in the main group underwent open hernioalloplasty using our modified technique.The technique includes a layer-by-layer opening of the anterior wall of the inguinal canal with the identification and mobilization of the spermatic cord, which is taken onto a holder and withdrawn. The hernial sac, after its careful dissection in the thickness of the cord, is carefully isolated, opened and its contents are inserted into the abdominal cavity.The bag is mobilized in the direction of the inner inguinal ring with separation from the surrounding elements. The base of the bag is hermetically sealed with a pouch seam using absorbable atraumatic material (Vicryl 3/0). A flap is formed from the remaining part of the hernial sac, a section of the parietal peritoneum, intended for the subsequent concealment of the implant.At the next stage, a polypropylene mesh implant is modeled and laid (the average size is 10×12 cm), taking into account individual anatomical parameters: the size of the posterior wall of the inguinal canal and the height of the hernial defect. The implant is positioned along the posterior wall of the canal in such a way as to reliably overlap the inner inguinal ring without compressing the structures of the spermatic cord. Graft fixation is performed with U-shaped sutures (Prolene 4/0) along its upper and lower edges.A pre-formed flap of the parietal peritoneum is placed on top of the mesh graft, which is fixed to the upper and lower walls of the inguinal canal with 6-8 nodular sutures (Vikril 4/0). This ensures reliable biological isolation of the synthetic material from the surrounding tissues, including the structures of the spermatic cord.The spermatic cord is placed on the formed "biological bed" — a flap of the parietal peritoneum, excluding its direct contact with the implant (Fig. 2). The final stage of the operation is suturing the aponeurosis of the external oblique abdominal muscle without tension, "edge to edge", over the spermatic cord, followed by a standard skin suture.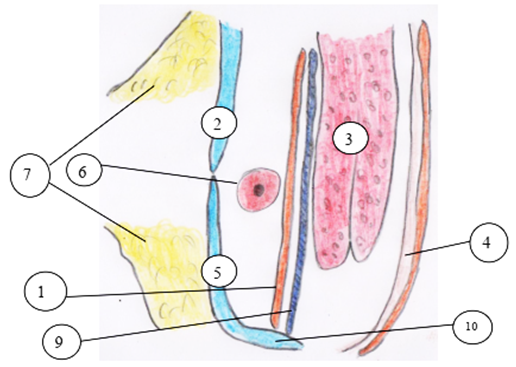 | Figure 2. Schematic image of the modified method, sagittal section: 1-hernial sac; 2-upper flap of aponeurosis of the external oblique abdominal muscle; 3-free edges of the internal oblique and transverse abdominal muscles; 4-transverse fascia; 5-lower flap of aponeurosis of the external oblique abdominal muscle; 6-spermatic cord; 7-subcutaneous adipose tissue; 8-allograft with pre-applied U-shaped sutures; 9-fixed allograft to the posterior wall of the inguinal canal; 10-lower wall of the inguinal canal, inguinal ligament |
3. The Results of the Research
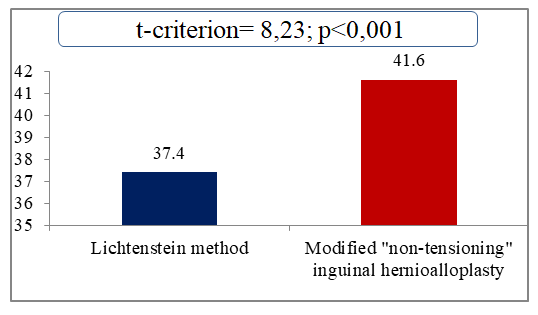
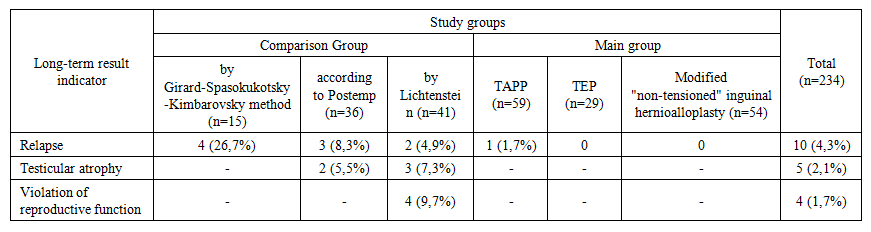
A comparative analysis of the duration of operations showed that our modified inguinal hernioalloplasty technique is comparable in time to classical hernioalloplasty using the Lichtenstein technique. Thus, the average duration of the operation according to the Lichtenstein method was 37.4 ± 0.5 minutes, whereas using the modified technique it was 41.6 ± 3.8 minutes (Fig. 3).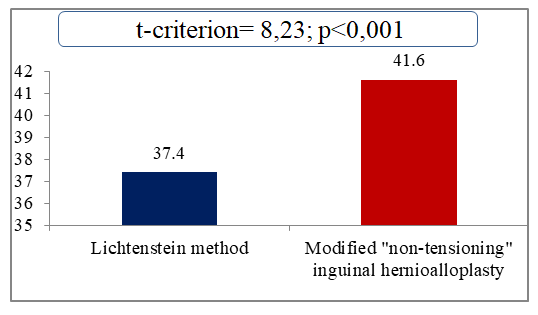 | Figure 3. Comparative indicators of the duration of open inguinal hernioalloplasty (min.) |
As part of our study, a comparative assessment of the duration of endovideosurgical and open interventions was carried out. It should be emphasized that the time of the operation was largely determined by the level of professionalism and clinical experience of the operating surgeon. Nevertheless, despite the fact that in some cases the duration of endovideosurgical interventions exceeded that for open operations, the overall quality of treatment and the clinical outcome with laparoscopic techniques turned out to be more favorable.Thus, the average duration of the operation using the TAPP method was 52.4 ± 0.8 minutes, while using the TEP method it was 45.3 ± 3.8 minutes (p < 0.001), as shown in Fig. 4. Despite the statistically significant time difference, both methods demonstrated high efficiency, minimal intraoperative complications, and good tolerability of the intervention.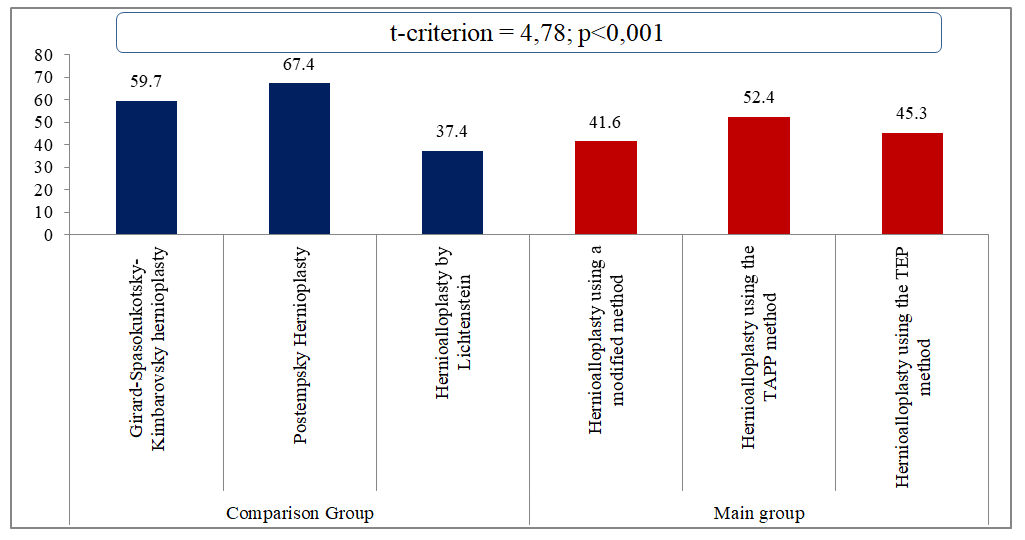 | Figure 4. Comparative indicators of operation duration (min.) |
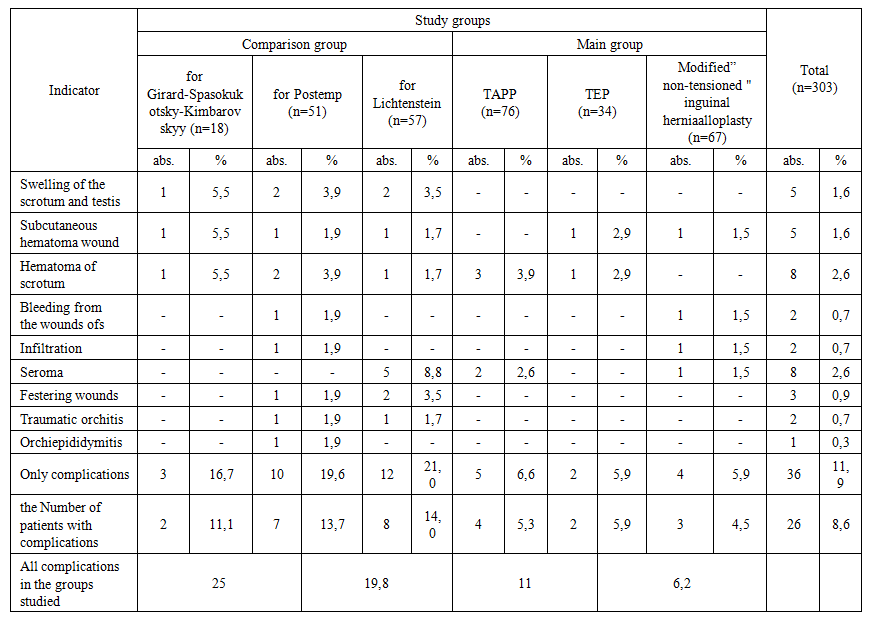
Thus, endovideosurgical interventions, subject to compliance with all stages of the technique and the proper level of qualification of the surgeon, are preferable in the context of reducing postoperative pain, accelerating recovery and improving the quality of life of patients in the early postoperative period.The analysis of the data presented in Table 2 indicates a significant difference in the frequency of early postoperative complications between the main observation groups. So, in the main group, the overall incidence of wound complications was 6.2%, while in the comparison group this indicator reached 19.8%. These data indicate a significantly lower risk of complications when using modern modified and minimally invasive hernioplasty techniques.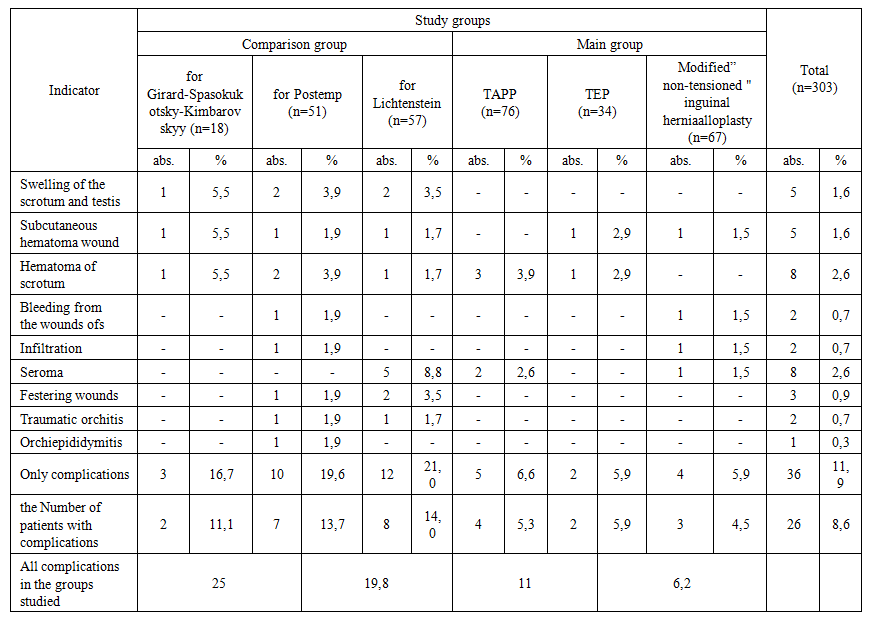 | Table 2. Early complications after inguinal hernioplasty |
Three years after surgery, the long-term results were analyzed in 234 patients (77.2%) out of 303 who underwent inguinal auto- and allogernioplasty. Of the 234 patients examined in the long term, recurrence of inguinal hernia was registered in 10 (4.3%) patients. In the comparison group, the recurrence rate was 9.8% (9 patients), while in the main group it was only 1.7% (1 patient) (Table 3).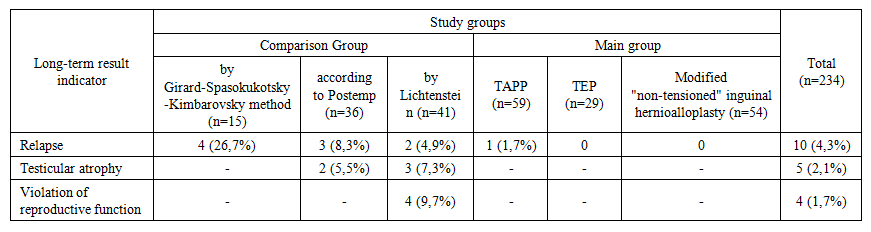 | Table 3. Frequency of non-satisfactory results in the long-term postoperative period |
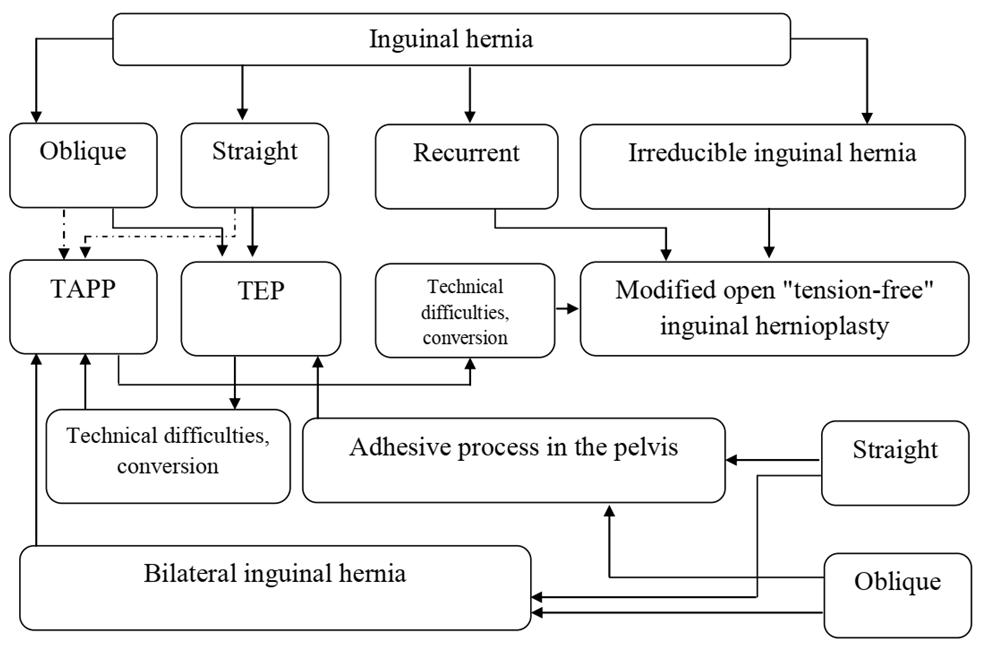
The use of endovideosurgical techniques TAPP and TEP, as well as the placement of a mesh implant using a hernial sac flap, significantly reduced the recurrence rate of inguinal hernia from 9.8% to 1.7%. The only case of recurrence in the main group was noted in a patient after TAPP surgery, which is associated with the patient's hypersthenic physique and incomplete closure of the hernial defect with a mesh prosthesis.Due to the presence of a biological barrier between the mesh implant and the spermatic cord, no complications affecting the structures of the spermatic cord and testis were reported in the main group of patients. In contrast, patients in the comparison group who underwent Lichtenstein surgery had testicular atrophy (in 3 cases) and impaired reproductive function (in 4 cases) in 7 (7.6%) cases. These complications, in our opinion, are caused by the formation of fibrous-cicatricial adhesions between the mesh implant and the spermatic cord, which led to venous congestion, lymphatic edema and subsequent testicular atrophy with impaired functional activity. Similarly, 2 (2.2%) patients after Postempsky surgery had testicular atrophy associated with infringement of the spermatic cord between the upper and lower flaps of the aponeurosis of the external oblique abdominal muscle.Based on the generalized clinical and surgical experience and analysis of the results of treatment of patients with inguinal hernias, we have developed a well-founded algorithm for the management of this group of patients, visualized in Figure 5.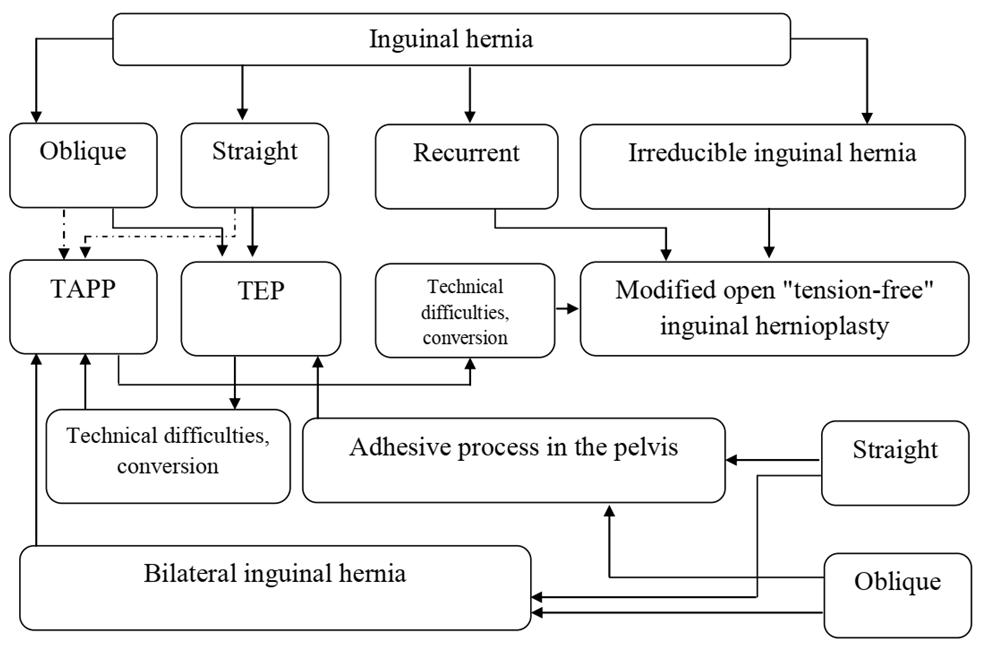 | Figure 5. Algorithm of tactics for choosing prosthetic hernioplasty for inguinal hernias |
4. Conclusions
The study found that the incidence of early postoperative complications using these techniques significantly decreased from 19.8% to 6.2% compared with traditional open methods. The minimal invasiveness and high physiology of these approaches ensure a more favorable course of postoperative rehabilitation, as well as contribute to reducing the risk of adverse effects on male reproductive function. In addition, in the long-term postoperative period, there is a significant decrease in the frequency of recurrence of the disease from 9.8% to 1.7%, which underlines the high efficiency and clinical feasibility of introducing modern minimally invasive and modified open techniques into the practice of surgical treatment of inguinal hernias.Modified open, non-tensioning inguinal hernioplasty using a hernial sac flap to cover a mesh implant demonstrated high clinical efficacy in reducing the frequency of postoperative seromas from 8.8% using the classical Lichtenstein technique to 1.5%. The formation of a biological barrier between the implant and the structures of the spermatic cord significantly reduces the risk of fibrotic scarring, minimizes the likelihood of compression of the vasospinal bundle, which, in turn, ensures the preservation of reproductive function in men (with a decrease in complications from 7.6% to 0%) and contributes to a more favorable course of the early postoperative period.Based on the data obtained and clinical experience, the developed and proposed algorithm of surgical treatment of inguinal hernias makes it possible to optimize the choice of hernioplasty method depending on the clinical situation and individual characteristics of the patient. The implementation of this algorithm contributes to improving the quality of medical care, reducing the incidence of complications and relapses, as well as increasing patient satisfaction with treatment results. Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
References
| [1] | Ivanov YV, Panchenkov DN, Afonina NS, Chugunov VS, Zinovsky MV. The Medical Economic Approaches to the Choice of Method of Surgical Treatment of Inguinal Hernias in Modern Conditions of Insurance Medicine. Journal of Experimental and Clinical Surgery. 2016; 9(1): 10-8. DOI: 10.18499/2070-478X-2016-9-1-10-18 (in Russian) |
| [2] | Ivanov YV, Avdeev AS, Panchenkov DN, Smirnov AV, Porkhunov DV, Mamoshin AV, Zinovsky MV. The choice of surgical treatment of inguinal hernia (literature review). Journal of experimental and clinical surgery. 2019 Oct 28; 12(4): 274-81. DOI:10.18499/2070-478x-2019-12-4-274-281. |
| [3] | Davlatov S, Rakhmanov K, Usarov S, Yuldoshev F, Xudaynazarov U, Tuxtayev J. Inguinal Hernia: Modern Aspects of Etiopathogenesis And Treatment. International Journal of Pharmaceutical Research (09752366). 2020 Jul 2. DOI: 10.31838/ijpr/2020.SP2.338. |
| [4] | Imangazinov SB, Kairkhanov EK, Kazangapov RS. Postoperative ventral hernias. Postoperative ventral hernia. Surgery and prevention of wound complications. Literature review. Literature review. Science & Healthcare. 2019(1): 29-41. (in Russian) |
| [5] | Chen K, Zhang J, Beeraka NM, Sinelnikov MY, Zhang X, Cao Y, Lu P. Robot-assisted minimally invasive breast surgery: recent evidence with comparative clinical outcomes. Journal of Clinical Medicine. 2022 Mar 25; 11(7): 1827. |
| [6] | Qiu Z, Li S, Tang J, Fang L, Pang Y, Chen L. Measurements of abdominal wall defect and hernia sac volume for the treatment of incisional hernia: Application of the ultrasonic volume auto-scan in 50 cases. Asian Journal of Surgery. 2023 Sep 1; 46(9): 3601-6. |
| [7] | Hori T, Yasukawa D. Fascinating history of groin hernias: Comprehensive recognition of anatomy, classic considerations for herniorrhaphy, and current controversies in hernioplasty. World Journal of Methodology. 2021 Jul 7; 11(4): 160. |
| [8] | Watanabe J, Izumi N, Kobayashi F, Miki A, Sata N. Efficacy and Safety of Transcutaneous Electrical Nerve Stimulation in Patients Undergoing Inguinal Hernia Repair: A Systematic Review and Meta-Analysis. JMA journal. 2023 Oct 16; 6(4): 371-80. |
| [9] | Jung S, Lee JH, Lee HS. Early outcomes of robotic transabdominal preperitoneal inguinal hernia repair: a retrospective single-institution study in Korea. Journal of Minimally Invasive Surgery. 2023 Sep 9; 26(3): 128. |
| [10] | Holland C, Numata K, Rnjak‐Kovacina J, Seib FP. The biomedical use of silk: past, present, future. Advanced healthcare materials. 2019 Jan; 8(1): 1800465. |
| [11] | Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014 Apr; 18: 151-63. |
| [12] | Reinpold W. Risk factors of chronic pain after inguinal hernia repair: a systematic review. Innovative surgical sciences. 2017 May 24; 2(2): 61-8. |
| [13] | Bittner JG, Clingempeel NL. Hernia repair in the United States: current situation and trends. The Art of Hernia Surgery: A Step-by-Step Guide. 2018: 115-22. |
| [14] | Perez AJ, Strassle PD, Sadava EE, Gaber C, Schlottmann F. Nationwide analysis of inpatient laparoscopic versus open inguinal hernia repair. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2020 Mar 1; 30(3): 292-8. |
| [15] | Engbang JP, Essola B, Fouda B, Baakaiwe LD, Chichom AM, Ngowe MN. Inguinal hernias in adults: epidemiological, clinical and therapeutic aspects in the city of Douala. Journal of Surgery and Research. 2021; 4(1): 95-118. |
| [16] | Ndong A, Tendeng JN, Diallo AC, Diao ML, Sow O, Mawuli SD, Kalli M, Harissou A, Choua O, Doumga AD, Togo AP. Adult groin hernia surgery in sub-Saharan Africa: a 20-year systematic review and meta-analysis. Hernia. 2023 Feb; 27(1): 157-72. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML