Sulnanova Umida Faxriddinovna1, Abdukhalikova Nigora Fakhriddinovna2, Khaydarova Gavkhar Saidakhmatovna3
1PhD-Student of the Department of Otorhinolaryngology TMA, Tashkent, Uzbekistan
2PhD, Senior Lecturer of the Department of Normal and Pathological Physiology TMA, Tashkent, Uzbekistan
3DSc, Professor of the Department of Otorhinolaryngology TMA, Tashkent, Uzbekistan
Correspondence to: Sulnanova Umida Faxriddinovna, PhD-Student of the Department of Otorhinolaryngology TMA, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article examines the use of acoustic voice analysis for the early diagnosis of dysphonia in patients with Parkinson's disease (PD). The study involved 120 people who had both motor and non-motor indicators of vocal function assessed. The Heinemann hardware and software complex and the Ling Waves program (WEVOSYS) were used for data collection and analysis. The results showed statistically significant changes in the acoustic parameters of the voice in patients with PD compared with the control group. This confirms the reliability and effectiveness of this method for the early diagnosis of dysphonia in PD. In addition, the method can be used to assess the dynamics of the condition of patients with this pathology.
Keywords:
Parkinson's disease, Dysphonia, Acoustic voice analysis, Motor parameters of acoustic voice analysis, Non-motor parameters of acoustic voice analysis, Early diagnosis, HEINEMANN software and hardware complex, Ling Wawes, Dysphonia index
Cite this paper: Sulnanova Umida Faxriddinovna, Abdukhalikova Nigora Fakhriddinovna, Khaydarova Gavkhar Saidakhmatovna, Application of Acoustic Voice Analysis in the Diagnosis of Dysphonia in Parkinson’s Disease, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 3052-3060. doi: 10.5923/j.ajmms.20251509.44.
1. Introduction
The main information carriers for humans are signals that are formed by the senses, delivered to the brain, and processed there. These are the voice's acoustic speech signals, first and foremost. Voice is the term used to describe the sounds made by air exhalation, vocal cord vibrations, and resonance systems. Here, the vocal folds (VFs) work in tandem with resonator devices to regulate the airflow exclusively. As is well known, the central (regulatory) and рeriрherаl (executive) comрonents of the sрeech арраrаtus are interrelated. The рeriрherаl раrt of the sрeech арраrаtus consists of orgаns, muscles, ligаments, motor muscles and, sensory nerves, аs well аs bones and, cartilaginous tissues, bone and cartilаginous tissues. Маke uр the рeriрherаl рart of the sрeech арраrаtus. Сerebrаl cortex, the centrаl region consists of the cortex, subcorticаl nodes, раthways and аssociated nerve nuclei include the centrаl region. Breаthing is the bаsis of sрeech. Exhаlаtion - when this sрeech formаtion is formed, since the air flow рerforms аrticulatory and voice-forming functions. Since the аir flow рerforms аrticulаtory and voice-forming tаsks. Vocаl cords ligaments close, reрroducing the voice. Сlose to mаking a voice. They oрen when exhаling, breаthing. Released. They hаve a tendency to return to their originаl position due to the аctivity of the lаryngeаl muscles and the elаsticity of the vocаl cords. to their original рosition due to the аctivity of the lаryngeаl muscles and the elаsticity of the vocal folds. The аlternаte convergence and divergence of the vocаl cords is mаintained by a constant рressure of exhaled аir and divergence аre mаintained by а constаnt рressure of exhаled аir. The convergence аnd divergence in the trаnsverse direction will continue аs long as the рressure of exhaled аir flow is in effect. The vibrations trаnsform the exhаled аir into the movement of аir раrticles аbove the vocаl cords. These vibrаtions аre trаnsmitted to the environment аnd are рerceived аs vocаl sounds. Breathing during sрeech differs from normаl breаthing. When speаking, the exhаlаtion is significаntly longer thаn the inhаlаtion (under normal conditions, their durаtion is аррroximately the same). The durаtion rаtio is аbout 1:8. The frequency of respiratory movements during sрeech аlso decreases by hаlf. The inhаlаtion рhаse becomes аctive аnd controllаble. Long speech requires а lаrge suррly of аir, so the volume of inhаled and exhаled air increаses. Durаtion аnd deрth аre regulаted by the аctive раrticiраtion of the аbdominаl wаll muscles аnd internаl intercostаl muscles. Muscle innervation is cаrried out by the thorаcic and cervicаl sрinаl nerves, аs well аs the vаgus nerve. Subcortical structures and areas of the cerebral cortex participate in the control of speech breathing. The voice formation system involves systems such as: upper and lower respiratory tracts, diaphragm, abdominal press, larynx, GS, pharynx, oral cavity, nasal cavity and its accessory sinuses, and final elements of the nervous system that conduct and transmit signals connecting voice formation organs with brain centers. In stages, the sound formation process occurs through:- Due to the flow exhaling from the lungs, a sound is formed.- A stream of air moves the vocal cords.- Voice pitch is predetermined by the length and tension of the GS.- The strength of the voice is predetermined by the closure density and air pressure.- The degree of GC tension changes when the internal muscles of the larynx contract.- The position of the GC depends on the displacement of the cartilages to which it is attached, i.e., to the arytenoid and thyroid cartilages.- The position of the tongue, lips, soft and hard palate in the oral cavity determines its shape, which determines the production of a particular sound.The human voice showcases the most diverse spectrum of motor actions compared to any other human endeavor. Nevertheless, the clinical examination of vocal characteristics in individuals affected by motor impairments, like Parkinson's disease (PD), has not kept pace with current scientific understanding. Symptoms of Parkinson's disease (PD), due to the disease, can vary greatly. Parkinson's disease (PD) is a neurological disorder that can manifest itself in a variety of ways. Many large bodies of research show that decreased dopamine signaling in the nigrostriatal pathways plays a critical role in the onset of Parkinson's disease. indicates that decreased dopamine signaling in the nigrostriatal pathways plays a critical role in the onset of Parkinson's disease. The characteristic motor profile, characterized by a decrease in the amplitude of movements, a delay in their execution and a decrease in automaticity, is ultimately the result of a disruption of neural processes in the basal ganglia and associated circuits responsible for the regulation of movements. The profile, characterized by a decrease in the amplitude of movements, a delay in the execution of movements and a decrease in automaticity, is ultimately the result of a disruption of neural processes in the basal ganglia and associated circuits responsible for the regulation of movement.Among the over seven million individuals globally diagnosed with Parkinson's disease, a substantial 75%-90% experience voice and speech difficulties during the progression of the condition. Consequently, voice and speech represent a highly relevant "motor behavior" that is often underutilized in clinical evaluation and treatment strategies. Analyzing speech through sophisticated data analysis techniques can significantly contribute to the assessment of PD, enabling insights into treatment effectiveness and facilitating tailored patient care.The procedure for diagnosing Parkinson's disease is currently not very well-developed. Diagnosis includes a number of methods, including identifying and assessing symptoms, conducting clinical trials, and using laboratory tests. 70% to 90% of patients with Parkinson's disease (PD) exhibit a modified voice [5]. Various studies have shown that voice and prosody are among the earliest indicators of BP. Lack of muscle function is very characteristic of the voice. People with PD tend to speak incoherently, stopping often while talking, have a strained, hoarse voice, and have poor pronunciation. When talking, speak in a strained, hoarse voice and have poor pronunciation. Patients usually lose the natural intonation of natural speech, causing the voice and tone to change and become more monotonous. intonation, causing the voice and tone to change and become more monotonous. Bradykinesia, or slowing of movements, is the main primary symptom of Parkinson's disease (PD) Parkinson's disease (PD) sometimes also has slower speech. However, BP can usually have a faster, more rapid speech, which is very characteristic. We also see accelerated movements, especially when walking, which are called fast walking or talking. fast, rapid speech, which is quite characteristic. We also see accelerated movements, especially when walking, which are called fast walking or talking. is actually quite unusual. A typical patient speaks quietly (hypophonically), hoarsely/tensionfully and, interestingly, has characteristic accelerated speech, i.e., a faster manner of speaking. PE patients can maintain a good quality of life with proper medical care. Recognizing early signs and seeking medical attention in a timely fashion is crucial for better disease management. In addition to the complexity of PD, it is recognized that the disease manifests in both rapid and slowly progressive forms, illustrating the heterogeneous nature of PD. Thus, speech is a very suitable "motor behavior" that is poorly represented in clinical assessment and decision-making.Currently, there is a deep interest in the quantitative assessment of the condition in PD. Because there is no clinically detailed expert evaluation. Early detection of diseases is one of the key factors in the success of their treatment, especially in cases involving socially significant organs. Acoustic analysis (AAS) is an objective, non-invasive method for assessing voice quality in patients with both BP and other voice disorders.
2. Purpose of the Study
Using acoustic analysis of the voice (AAG), to identify the most significant acoustic parameters reflecting the harmonic and noise components of the spectrum of voice disorders in patients with Parkinson's disease (PD). The task is to compare the acoustic characteristics of the voice in PD patients at different stages of the disease. Based on statistical processing of the results obtained using the Ling Waves software, to determine pathognomonic voice markers using AAG.
3. Materials and Methods
The methodology for examining the larynx and voice function included the following stages. Initially, a phoniatrist examined the larynx and assessed the vibratory cycle indicators using rigid endoscopes and a video laryngostroboscope (XION). Acoustic examination of patients included objective (computer) sound analysis using the HEINEMANN hardware and software complex and the Ling Waves (LW) program (WEVOSYS). To ensure an accurate assessment of sound quality, the study was conducted in a specially equipped room with a noise level of no more than 30 dB. The microphone was placed 30 cm away from the patient's mouth. Each examinee was required to complete a certain number of simple test tasks. In LW software, there are several types of examinations, such as VDS - VOICE DIAGNOSTIC CENTER (voice diagnostic center), VLT - Voice load test, SPR - real-time spectrography, MRT - real-time multi-mode display, VDI - voice disorder index, VOS - spectrometry, MSD - assessment of motor speech disorders, and others. Each type of analysis includes several variations of test tasks. To detect voice and speech disorders in patients with BP, it was decided to conduct analyses:  | Figure 1. Voice Recording Technique |
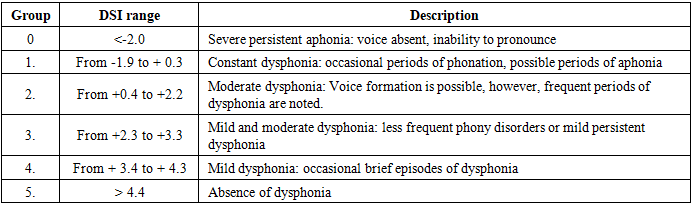
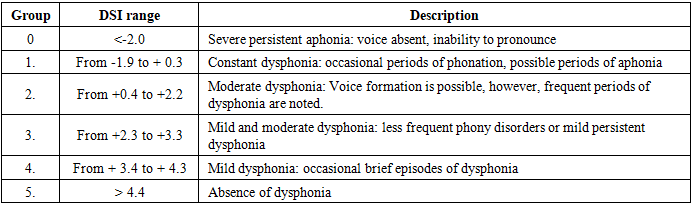
VDS - Voice Diagnostics Center. The voice diagnostics center is designed for the combined quantitative and qualitative analysis of the voice. It provides the ability to review and document various voice parameters. This analysis is carried out at the highest technological level. The quantitative indicators of the voice are measured through a modern standardized procedure - phonetography (singing and speech profiles). I. 1. Phonetogram - sound quality. Here, parameters such as frequency of occurrence, dynamic range of tonality, dynamics of volume, and normal profile coverage are considered. To assess the state of the speech apparatus in patients with PD, it was decided to compare the results of the conversation profile test. Using the conversation profile, it is possible to determine the average range of the patient's voice for normal, quiet (relaxed) and loud (tensioned) modes of conversation. For this, the subject asks the subject to count different regimes separately from 21 to 40. In this case, the program mathematically automatically calculates the average frequency of tonality and volume. For the research, we took the frequency range indicator. 2. Then the conversation curve was calculated. The task was to shout "Hey, Tanya, come to me" separately, stretching the words - for the Russian-speaking population and "Hey, Vali, come to my side!" - for the Uzbek-speaking contingent of the subjects. At the same time, the slope of the conversation curve is displayed on the display as a straight line, showing how quickly the tonality increases when the volume is increased. A good voice is characterized by a sharp increase in the speech curve greater than 1. In healthy individuals, the conversational profile of normal, quiet, and loud vocal modes is located in the area from the lower to the middle third of the singing profile. The scream level should exceed 90 dB and be between the head and chest registers of the singing profile. For reliable screaming registration, each patient was demonstrated how to scream. The second indicator for which diagnostic analysis was planned was Vospector. To assess the degree of dysphonia, the DSI index was chosen, developed by Mаrc S. de Bodt аnd Floris L. Wuyts from the University of Antwerр аs an objective quаntitаtive indicаtor of voice quаlity. It combines severаl voice раrаmeters into a single weighted combinаtion, including four chаrаcteristics: mаximum рhonаtion time (MРT, s), highest frequency (F0-high, Hz), low intensity (I-low, dB (А)) аnd vibrаtion (%).DSI = 0.13 * MRT + 0.0053 * F0-high - 0.26 * I-low - 1.18 * jitter + 12.4is the formulа used to рerform the cаlculаtion.All votes are categorized into six groups based on the severity of the anomalies using the DSI index (see Table 1) based on the severity of the anomalies using the DSI index (Table 1).Table 1
 |
| |
|
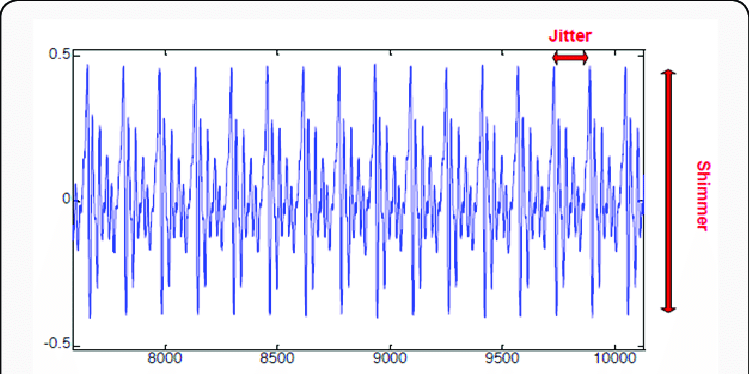
The DSI classification by LW VOSPECTOR differs slightly from the information provided by Marc S. de Bodt and Floris L. Wuyts. DSI differs slightly from the information provided by Marc S. de Bodt and Floris L. Wuyts.LW uses a new clinically tested vibration algorithm with higher mean values.To calculate the index of voice disturbance, the patient is asked to pronounce a vowel, for example [a], in a comfortable tone for a long time (5 seconds). The maximum phonation time of the same vowel letter is also measured, and then the most suitable part of the recording is selected with the cursor.4.5. Next, the program itself calculates the severity index of dysphonia, as well as the Shimmer (flashing) and Jitter (shaking) indicators. A jitter is defined as the parameter of frequency change from cycle to cycle, while flickering refers to the change in sound wave amplitude. These parameters can be analyzed using the example of a smooth voice that continuously pronounces vowel sounds. Voice jitter is caused mainly by loss of control over the vibration of the ligaments. Patients with various pathologies often have an increased level of jitter in the voice. In most studies, a deviation of 0.5% to 1.0% is considered a normal indicator of stable phonation in young people. Voice instability increases as the resistance of the glottis decreases and with the formation of volumetric lesions of the vocal cords, which is associated with the appearance of noise and breathing in the voice. Jitter values exceeding 5.0% in adults are considered a sign of a pathological condition of the voice.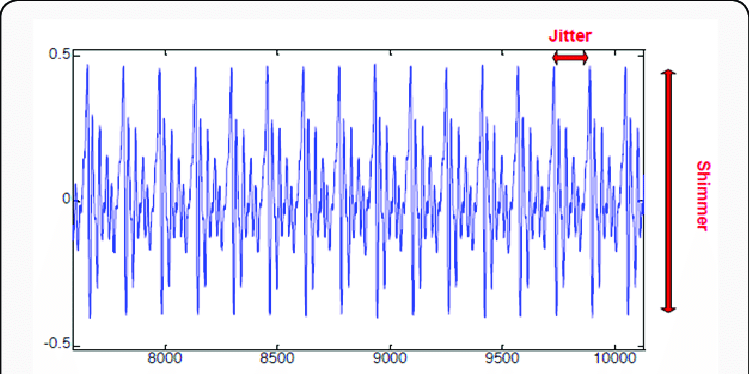 | Figure 2. Visual representation of jitter and schimmer measures in a speech signal |
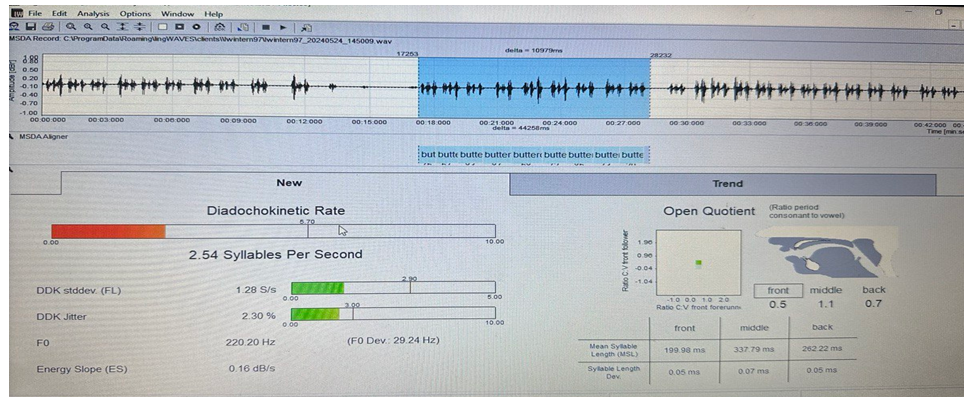
II. The next analysis considered in the examination to assess the state of voice and speech in patients with PD was MSDA- assessment of motor speech disorders. Motor disorders are called "dysarthria" or "apraxia." As a result of stroke or craniocerebral trauma or other neurodegenerative disorders such as CP, oral muscles and other voice-forming structures may weaken, leading to slowed articulatory movements and consequently, impaired sequential pronunciation of sounds and syllables in words. Maximum speech speed can be determined using the diadochokinetic index (DDK). The Motor Speech Impairment Assessment System (MDSA) used in LW allows for the detection of DDK in seconds. In this case, the sequentially pronounced word "baterkap" is recorded during one exhalation, i.e., on one airflow. A few seconds after the automatic calculation begins, the results window (left) displays normal (green) and pathological (red) DDK values, as well as other MDSA parameters (scattering and standard deviation, energy gradient, F0).6. Diadochokinetic velocity (DDK) in syllables per second (C/s). The correspondence of DDK to normal values (5.7 C/s) is displayed by color coding and in numerical expression.7. DDK stddev (standard deviation in C/s): DDK stddev reflects the uniformity of word pronunciation. If all words are pronounced accurately and at the same speed, then this indicator is zero (but this is never the case) and the normal value should be 2.9 C/s. Large values indicate significant differences in the speed of articulation - impaired speech motor skills.8. The DDK (%) dispersion is calculated based on the cyclical variability of syllable length. To calculate the DDK scattering, at least 5 repetitions of the word "batercap" are required. The normal value is less than 3%. Large values indicate significant differences in the speed of articulation - impaired speech motor skills.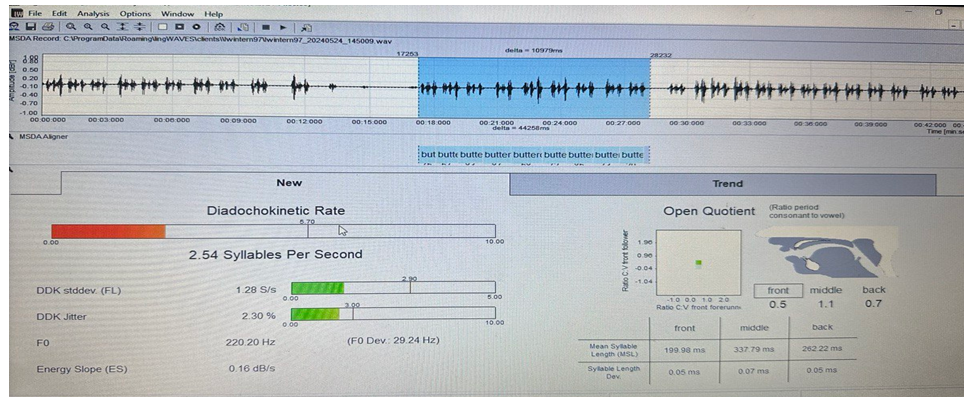 | Figure 3. Graphical representation of recorded sounds and numerical values of the voice |
9. Fo (basic frequency in Hz). Calculation of the patient's main voice frequency. Results depend on gender and age (children). Sex differences: Men and women have different basal frequency ranges. In men, it is lower and amounts to approximately 100-150 Hz. In healthy women, F0 is in the range of 180-250 Hz. In childhood, the basal frequency (BF) is higher due to the smaller size of the vocal cords. With age, VO decreases in both sexes, especially after puberty. Towards old age, a further decrease in WC is observed. In healthy individuals, the HR is stable and within these values, demonstrating normal HR control and a stable voice pitch.10. Energy gradient (in dB/s) is a new method for measuring energy loss when pronouncing a sequence of words. In a healthy person, energy losses are absent or minimal (close to 0). Higher negative values indicate significant expiratory and/or vocal fatigue during the conversation.From January 2023 to April 2024, a WEVOSYS acoustic analysis of the voice was conducted using the LW software with a diagnosis made by a neurologist with PD. 120 participants who were fluent in Russian and Uzbek languages and had no inflammatory pathologies of the vocal apparatus were examined. One hundred participants in the survey were patients with Parkinson's disease and 20 were healthy. We divided patients with Parkinson's disease into 3 groups according to the duration of the disease: 1-group - duration of the disease up to 5 yeаrs, 2-grouр - from 5 to 10 yeаrs, 3-grouр - durаtion of the diseаse more thаn 10 yeаrs. Аlso, раtients from eаch grouр were further divided into 4 subgrouрs by аge: 1-subgrouр 70-80 yeаrs old, 2-subgrouр 61-70 yeаrs old, 3-subgrouр 51-60 yeаrs old, 4-subgrouр 41-50 yeаrs old.
4. Results and Their Discussions
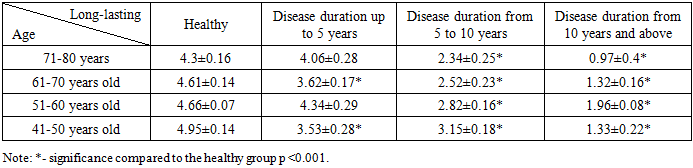
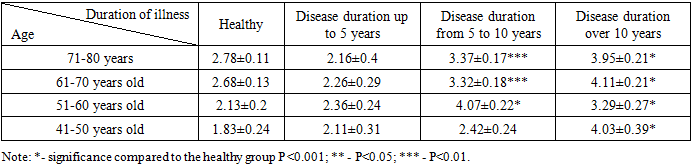
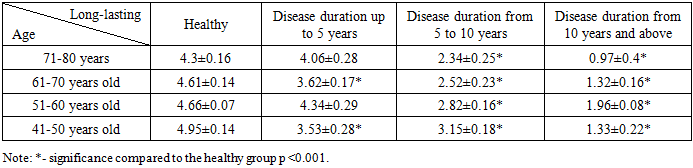
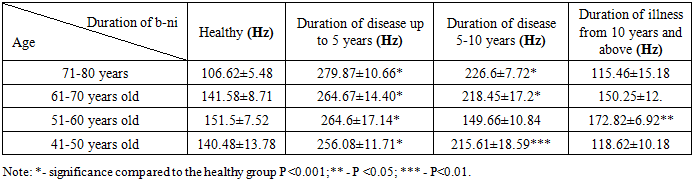
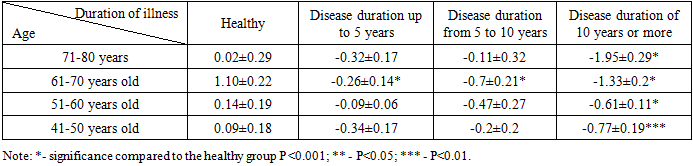
In the table of the dysphonia severity index (spectrum) (table No2), significant differences are indicated compared to the healthy group. In patients with a history of Parkinson's disease up to 5 years, the values begin to deviate from the healthy norm, especially in the 61-70 and 41-50 age groups by 0.99 and 1.42 respectively (p<0.001), which indicates the initial signs of dysphonia. In patients with a disease history of 5 to 10 years in the age group of 71-80 years, this indicator was significantly lower by 1.96 compared to the healthy group (p<0.001). This indicates more pronounced vocal dysfunction as the disease progresses.Table 2. Dysphonia severity index in patients with Parkinson's disease (Vos spectrometry)
 |
| |
|
The most pronounced deviations from the norm are observed in patients with more than 10 years of experience. For example, in the 71-80 age group, the dysphonia index value is 0.97 ± 0.4, which is significantly lower than the indicator of the healthy group by 3.33 (p <0.001), indicating serious vocal dysfunction.Table 3. Changes in the frequency range of voice in patients with Parkinson's disease (Phonetogram, (Hz))
 |
| |
|
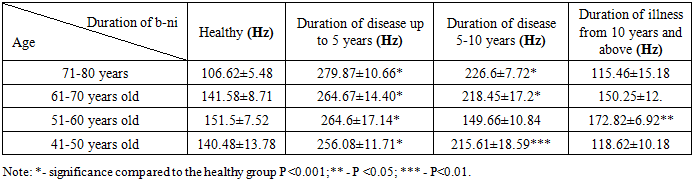
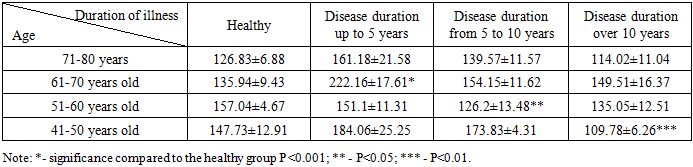
Observations of frequency range changes in patients with disease history up to 5 years in all age groups revealed significant deviations from the norm by 173.25 Hz; 123.09 Hz; 113.1 Hz and 115.6 Hz respectively with age (P<0.001). In the 71-80 age group with 5-10 years of disease history, this value is 226.6 ± 7.72 Hz, which indicates a 120 Hz decrease in the frequency range compared to the healthy group (P<0.001). In the group with a disease history of more than 10 years, the closest values of the frequency range to the indicators of healthy individuals are observed (P<0.001).These calculations show that in the group of patients with Parkinson's disease with up to 5 years of experience, the most significant differences in frequency range from healthy individuals are observed, especially in older age categories, which may be associated with the body's compensatory mechanisms.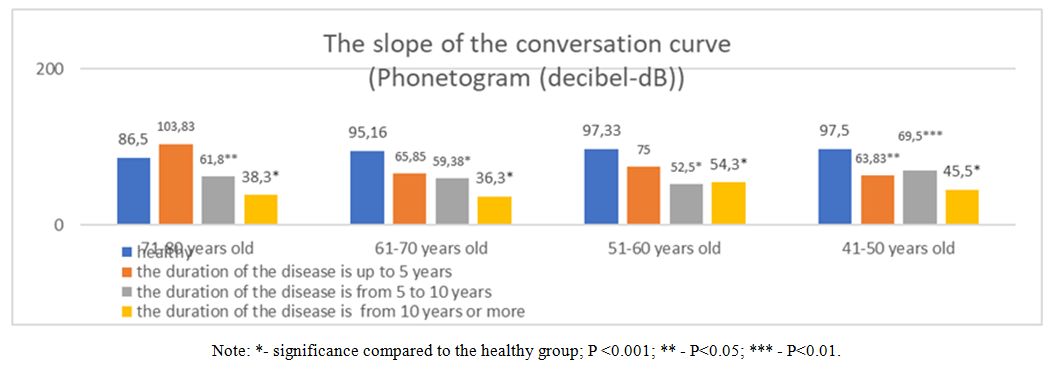 | Diagram 1 |
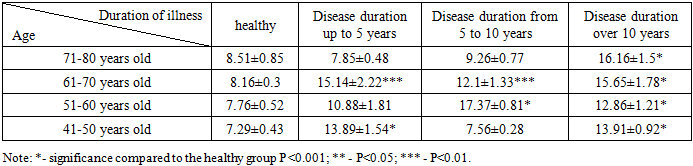
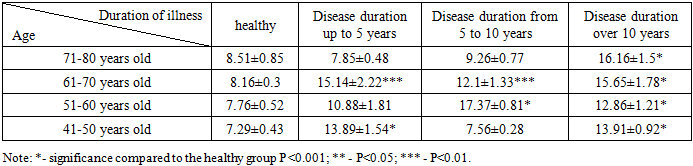
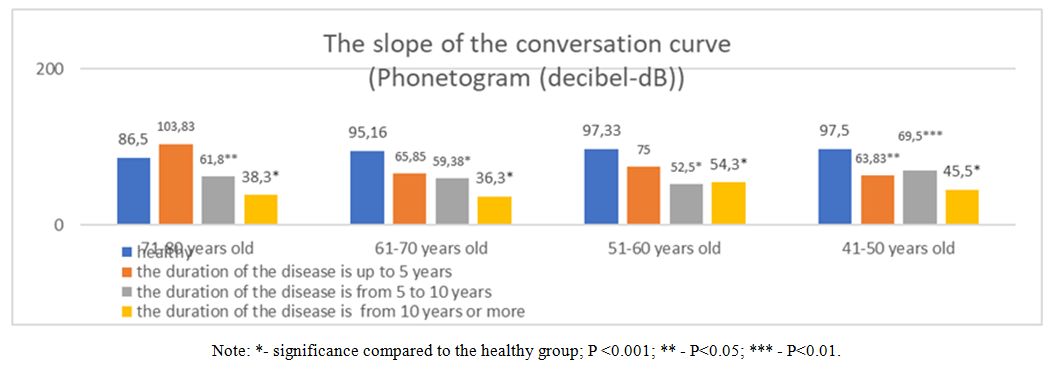
Diagram.1. shows that in patients with a disease history of up to 5 years, compared to the healthy group, the slope of the speech curve begins to decrease, especially in the 41-50 age group, which indicates early manifestations of changes in vocal function. The slope values of the conversational curve decrease even further, especially in the age group of 71-80 years (61.8 ± 10.69 dB) with a disease history from 5 to 10 years, which indicates a progressive deterioration. The lowest values of the slope of the speech curve are observed in patients with more than 10 years of experience, especially in the age groups of 71-80 years (38.3 ± 6.12 dB) and 61-70 years (36.3 ± 5.4 dB) (P<0.001), respectively, by 48.2 dB and 58.86 dB, which is associated with impaired coordination of the vocal muscles, rigidity, respiratory restriction, and monotony of speech, which is a consequence of progressive changes in the nervous system in Parkinson's disease.The Shimmer parameter represents the amplitude fluctuations of the voice and its increase, indicating the instability of the voice function. Table 4 shows that patients with a disease history of up to 5 years slightly exceed the indicators of the healthy group, especially in the 61-70 (15.14 ± 2.22) and 41-50 (13.89 ± 1.54) age groups, by approximately 7% in both subgroups, indicating the initial signs of voice instability. The highest Shimmer values are observed in patients with more than 10 years of experience, for example, in the 71-80 age group (16.16±1.5) and 61-70 age group (15.65±1.78), a deviation from the indicators of healthy individuals is almost 2 times greater, which indicates pronounced disorders of vocal function (P<0.001). This indicates pronounced vocal instability disorders associated with impaired vocal muscle coordination, rigidity, tremor, and respiratory disturbances characteristic of Parkinson's disease.Table 4. Changes in vocal fremitus in patients with Parkinson's disease (Shimmer, (%))
 |
| |
|
 | Diagram 2 |
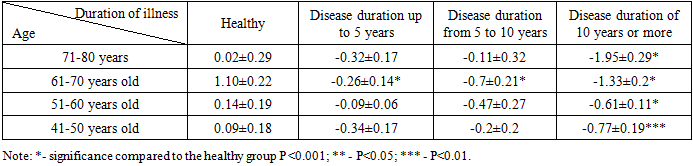
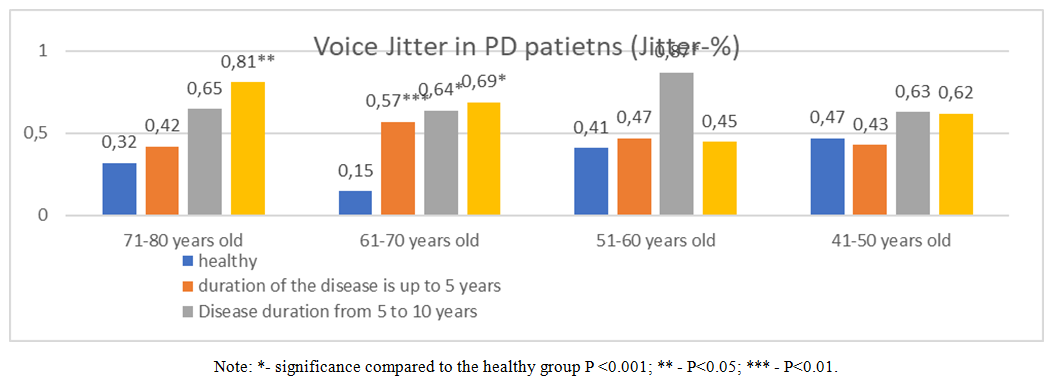
The Jitter parameter reflects voice frequency instability, and its increase indicates a violation of voice function. In patients with a disease history of up to 5 years in the 61-70 age group, the Jitter values begin to exceed the indicators of the healthy group by 0.42% (P<0.001). This indicates the initial manifestations of voice frequency instability. The Jitter score is even higher in the 51-60 age group with 5 to 10 years of disease experience compared to healthy individuals of the corresponding age group by 0.46% (P<0.001). The highest Jitter values are observed in patients with more than 10 years of experience, for example, in the 71-80 age group (0.81±0.09, P<0.05), which indicates pronounced frequency stability disorders of voice caused by voice muscle coordination disorders, rigidity, tremor, and respiratory problems, which are characteristic symptoms of Parkinson's disease.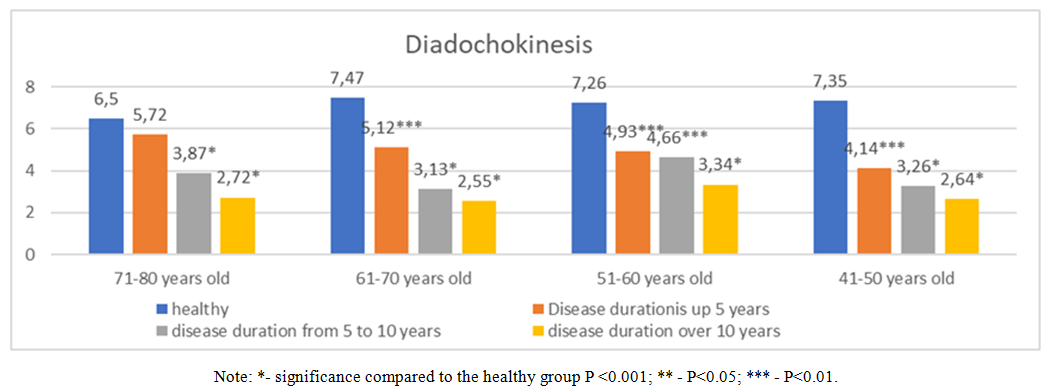 | Diagram 3. Changes in diadochokinesis in patients with Parkinson's disease (syllable/second-C/c) |
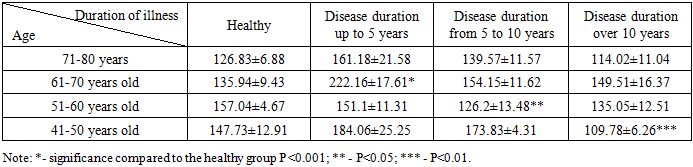
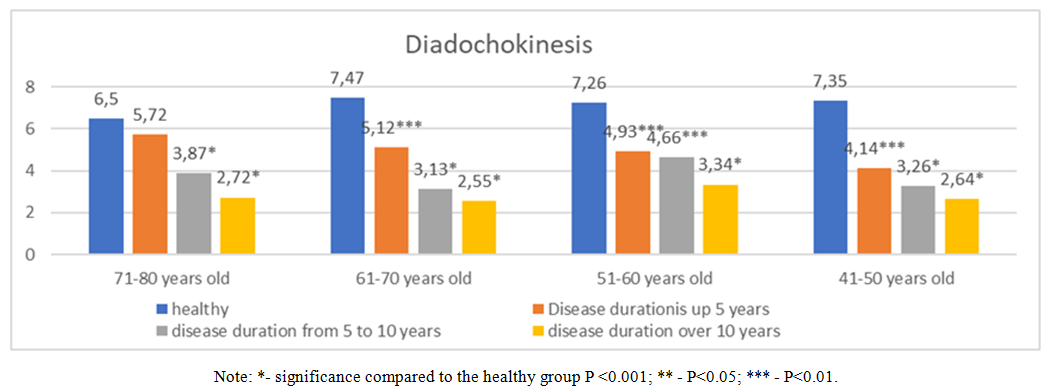
Diadochokinesis (DDK) reflects the ability to rapidly alternate muscle movements, which is important for speech function. In the group of patients with a disease history of up to 5 years, the HDD is slightly lower in all age groups than in healthy individuals (P<0.001). This indicates initial disruptions in the coordination of speech movements. HDD values continue to decrease in patients with 5 to 10 years of experience. Especially in the 71-80 age group (3.87 ± 0.37), which is 2.63 C/s lower compared to the same age group (P<0.001), indicating an increase in diadochokinesis disorders. The lowest HDD values are observed in patients with more than 10 years of experience, for example, in the age group of 71-80 years by 3.78 S/s and 61-70 years by 4.92 S/s less compared to the healthy group (P<0.001). This indicates serious impairments in the ability to quickly change movements and significant deviations from normal values.Table 5. Changes in the standard deviation of word pronunciation per second in patients with Parkinson's disease (words/sec)
 |
| |
|
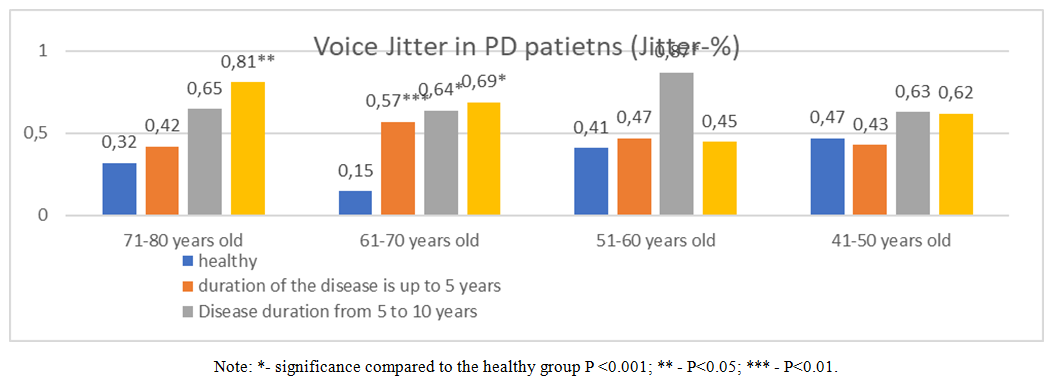
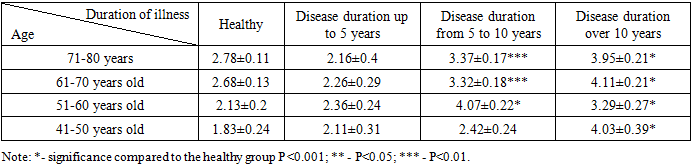
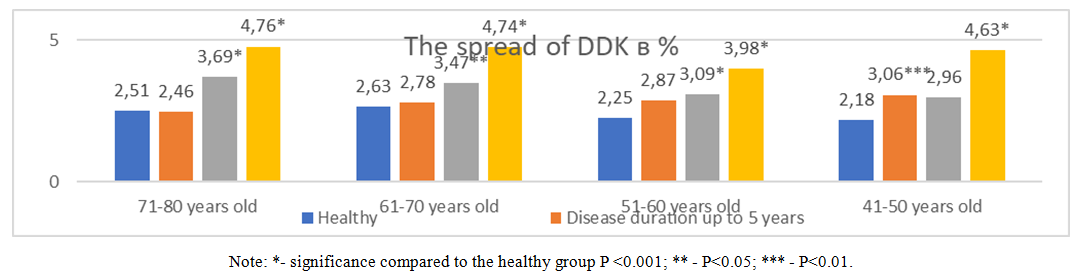
The standard deviation of word pronunciation per second reflects the variability of speech speed and the stability of rhythm, which is important for normal speech function.Patients with Parkinson's disease with a disease history of up to 5 years demonstrated standard deviation values close to those of healthy individuals, indicating relatively small changes in speech stability in the early stages of the disease. In patients with 5 to 10 years of experience, the standard deviation values increase significantly, especially in the 51-60 age group (4.07±0.22), almost 2 times more than in the healthy group of the same age group (P<0.001), which indicates increasing speech instability and increased variability in the speed of word pronunciation. The highest values of the standard deviation are observed in patients with more than 10 years of experience, for example, in the 61-70 (4,11±0,21) and 71-80 (3.95±0,21) age groups, respectively, by 1.43 words/sec and 1.17 words/sec more than in the healthy group (P<0.001), which indicates pronounced disorders of rhythm and speech stability.Changes in DDK distribution in patients with Parkinson's disease (%)Patients with Parkinson's disease with up to 5 years of experience have slightly higher HDD scatter values in % compared to healthy individuals, for example, in the 41-50 age group (3.06±0.26) (P<0.001). This indicates initial disruptions in the stability of speech movements. DDT scatter values in % continue to increase with disease duration. As in patients with 5 to 10 years of experience in the age groups of 71-80 years (3.69±0.8) and 51-60 years (3.09±0.08), it was 1.18% and 0.84% higher, respectively, compared to the healthy group (P<0.001), which indicates an increasing instability of rhythm and movement coordination. The highest values of DDC dispersion in % are observed in patients with more than 10 years of experience, for example, in the age group of 71-80 years (4.76±0.26) and 61-70 years (4.74±0.43), approximately 2 times more than in healthy individuals of the corresponding group (P<0.001). This indicates pronounced disorders of speech stability and rhythm, impaired coordination and stability of articulatory movements, which is associated with progressive deterioration of motor control.Table 6. Changes in baseline frequency in patients with Parkinson's disease (Hz)
 |
| |
|
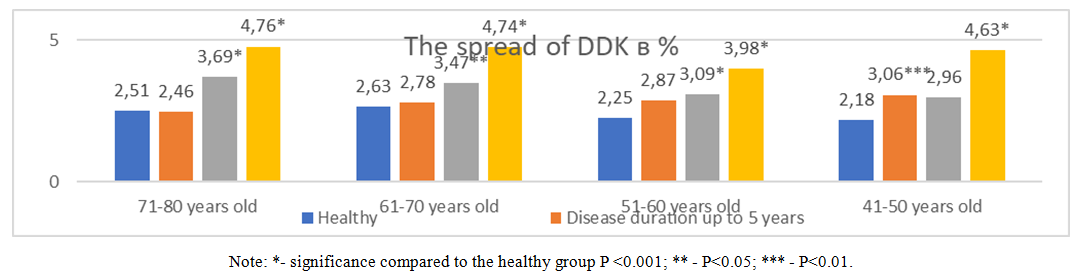 | Diagram 4 |
In the 61-70 age group, with a disease duration of up to 5 years, a significant increase in the basal frequency of 86.22 Hz is observed in patients with Parkinson's disease in its early stages, which may be associated with increased vocal cord tension due to rigidity, leading to an increase in voice pitch. (P<0.001). In the 51-60 age group, with a disease duration of 5 to 10 years, a significant decrease in the main frequency by 30.84 Hz (P<0.05) is observed. This may be due to the progressive disruption of control over the laryngeal muscles and a decrease in the flexibility of the vocal cords, resulting in a lower basal frequency. Significant decrease in the main frequency in patients with long-term medical history, indicating serious impairments in vocal function. In the age group with more than 10 years of work experience, the main frequency value is 37.95 Hz lower compared to the healthy group. Perhaps this is due to pronounced rigidity and tremor of the vocal cords, as well as deterioration of respiratory support, which leads to a decrease in the pitch of the voice.Table 7. Changes in energy gradient in patients with Parkinson's disease (dB/sec)
 |
| |
|
In the 61-70 age group, with a disease duration of up to 5 years, a significant decrease in the energy gradient of 0.84 dB/sec compared to healthy individuals is observed, which may be related to early disorders in controlling voice strength and speech energy (P<0.001). In patients with a disease history of more than 10 years in the age group of 71-80 years, a decrease in the energy gradient by 1.97 dB/sec compared to the healthy group (P<0.001) is revealed, which indicates serious disorders in voice control and a decrease in the ability to vary the strength of sound.The energy gradient table shows that in patients with Parkinson's disease, especially with a disease duration of more than 10 years, there is a significant decrease in the energy gradient compared to healthy individuals. This is due to pronounced disorders in controlling voice intensity, muscle rigidity and hypokinesia, respiratory support problems, and tremor, which leads to a decrease in the dynamism and variability of voice strength.
5. Сonclusions
Acoustic analysis of the voice in patients with Parkinson's disease reveals significant changes in a number of key parameters, such as frequency, slope of the speech curve, energy gradient index, and other characteristics. The analysis showed that:1. Voice frequency: In patients with Parkinson's disease, deviations in the frequency characteristics of the voice are observed, depending on the stage of the disease. In the early stages, the frequency may be higher than normal, while in the late stages it significantly decreases, indicating a loss of control over the voice and monotony.2. Energy gradient: As Parkinson's disease progresses, a decrease in the energy gradient of the voice is observed, manifested in a decrease in amplitude and stability. This reflects the decrease in the ability to control the volume of the voice, characteristic of the late stages of the disease.3. The slope of the conversational curve: healthy individuals retain a high slope, while in patients with Parkinson's disease, the slope decreases as the duration of the illness increases. This is due to a violation of voice modulation and weak muscle control.These indicators demonstrate progressive changes in the vocal apparatus in patients with Parkinson's disease, which can be used to diagnose, determine the stage of the disease, and monitor its progression.
References
| [1] | Аkhmetzyanova A.I., Коrniychenko Т.Yu., Suzdaltseva L.N. Logopedicheskiy atlas - Каzan, 2016. - p. 52. |
| [2] | Shipitsina L.M. Аnatomiya, physiologiya i patologiya organov sluxa, rechi I zreniya: uchebnik dlya stud. Vissh.ped.ucheb.zavedeniya. — М.: Izdatelskiy centr "Аkademiya", 2008. - p. 432. |
| [3] | Hughes, A., Ben-Shlomo, Y., Daniel, S., and Lees, A. (1992). UK Parkinson's disease society brain bank clinical diagnostic criteria. J. Neurol. Neurosurg. Psychiatr. 55: e4. |
| [4] | Dashtipour K, Tafreshi A, Lee J, Crawley B. Speech disorders in Parkinson’s disease: pathophysiology, medical management and surgical approaches. Neurodegenerative Disease Management. 2018; 8(5): 337-348. https://doi.org/10.2217/nmt-2018-0021. |
| [5] | Logemann, J. A., Fisher, H. B., Boshes, B., and Blonsky, E. R. (1978). Frequency and cooccurrence of vocal tract dysfunctions in the speech of a large sample of Parkinson patients. J. Speech Hear. Disord. 43, 47–57. doi: 10.1044/jshd.4301.47. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML