-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(9): 3031-3037
doi:10.5923/j.ajmms.20251509.40
Received: Aug. 19, 2025; Accepted: Sep. 5, 2025; Published: Sep. 25, 2025

Integration of Artificial Intelligence and Digital Radiological Processing in the Diagnostics of Paranasal Sinus Pathology Using Computed Tomography
A. A. Ikramov
Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: A. A. Ikramov, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to analyze the potential of machine-learning algorithms and digital radiological processing technologies in the diagnostics of paranasal sinus diseases and to evaluate the efficiency and prospects of their implementation into clinical practice. Background. Pathology of the paranasal sinuses occupies a significant place in the structure of ENT diseases. According to epidemiological studies, chronic sinusitis occurs in 12–15% of the adult population, and an accurate evaluation of the prevalence and nature of the process requires the use of highly informative imaging methods such as computed tomography and magnetic resonance imaging. Material and methods. The study included 160 people. All patients were divided into two groups. The main group (n=120) consisted of patients with confirmed paranasal sinus pathology. The control group (n=40) consisted of healthy volunteers with no signs of paranasal sinus disease according to clinical and radiological examination data. Results. Computed tomography data of all patients were used not only for clinical diagnostics, but also for forming a sample of images used in training and testing artificial intelligence algorithms. When integrating the deep learning algorithm into the process of analyzing CT images of patients in the main group, it was found that the system efficiently identified key diagnostic features for each form of pathology, which allowed to increase accuracy and standardize interpretation. Discussion. The developed model for classifying paranasal sinus pathologies based on deep learning algorithms demonstrated high diagnostic efficiency, ensuring 85.8% recognition accuracy, which significantly exceeds the indicators of specialists with low (71.7%), medium (78.4%) and even high (73.4%) qualifications. Such result confirms the potential of artificial intelligence algorithms as a tool of clinical decision support in the analysis of computed tomography data. Conclusion. The integration of artificial intelligence and radiological processing into the diagnosis of paranasal sinus diseases contributes to an increase of diagnostic accuracy and efficiency of the physician's work, creating prerequisites for a personalized approach to patient treatment.
Keywords: Artificial intelligence, Digital radiological processing, Computed tomography, Paranasal sinus pathology, Automatic diagnostics, Medical imaging
Cite this paper: A. A. Ikramov, Integration of Artificial Intelligence and Digital Radiological Processing in the Diagnostics of Paranasal Sinus Pathology Using Computed Tomography, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 3031-3037. doi: 10.5923/j.ajmms.20251509.40.
Article Outline
1. Introduction
- Pathology of the paranasal sinuses (sinusitis, frontal sinusitis, ethmoiditis, sphenoiditis, polypous changes, tumor processes) occupies a significant place in the structure of ENT diseases. In recent years, the clinical picture of these diseases has undergone changes, which is manifested by an increase of the number of erased and latent forms. A significant proportion of patients with rhinosinusitis do not experience pain, and the disappearance of local pain after the start of therapy is not always a sign of complete recovery. If until the end of the 20th century, clinicians widely believed that local headache during acute inflammatory processes of the paranasal sinuses and exacerbations of chronic forms was the leading diagnostic sign (Piskunov S.Z., 1991), in recent years this approach has been revised and its diagnostic value has been seriously questioned (Stagnieva I.V., 2008).In spite of the improvement and extension of the range of diagnostic and therapeutic technologies, the prevalence of inflammatory diseases of the paranasal sinuses remains high and shows no tendency to decrease (Piskunov S.G., 2013). According to a number of studies, the incidence of chronic rhinosinusitis has increased more than threefold over the past two decades (Kozlov V.S., 2003; Kleshchin D.A., 2005). At the same time, the clinical manifestation of sinusitis becomes less typical: there is more and more often no pronounced local pain or it is of low intensity, which complicates early diagnostics. According to epidemiological studies, chronic sinusitis occurs in 12–15% of the adult population, and an accurate evaluation of the prevalence and nature of the process requires the use of highly informative imaging methods such as computed tomography (CT) and magnetic resonance imaging (MRI) [1].The traditional interpretation of images largely depends on the physician's experience and the quality of the source material, which creates conditions for subjective errors. The integration of artificial intelligence and digital radiological processing technologies opens up new opportunities for objectifying analysis, automating pathology recognition, and standardizing descriptions, thereby improving the accuracy and reproducibility of diagnostic conclusions [2].Taking the above into account, there is growing interest in the introduction of objective technologies in diagnostics. The paranasal sinus area is especially important, where deep learning algorithms are already showing their practical value.In a study on paranasal sinus segmentation, the multi-class 3D U-Net achieved an F1 score of 84.3% for healthy sinuses and 79.3% for pathological sinuses, which highlights the clinical potential of automation in navigation and preoperative planning [3,4].In a separate study, a deep neural network-based algorithm demonstrated 85.8% accuracy in classifying sinusitis from CT scans, significantly outperforming physicians' results, ranging from 71.7% to 78.4% depending on skill level [5-7].The integration of AI and digital radiological processing into daily work can dramatically improve the detection and management of paranasal sinus pathology, especially in the context of the growth of hidden and atypical forms of diseases [8,9].The aim of the study was to analyze the potential of machine-learning algorithms and digital radiological processing technologies in the diagnostics of paranasal sinus diseases and to evaluate the efficiency and prospects of their implementation into clinical practice.
2. Material and Methods
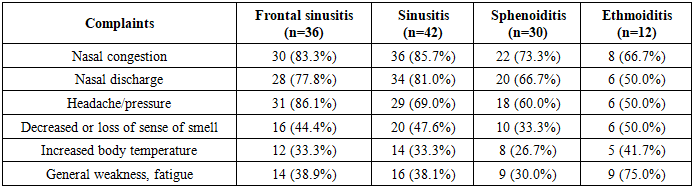
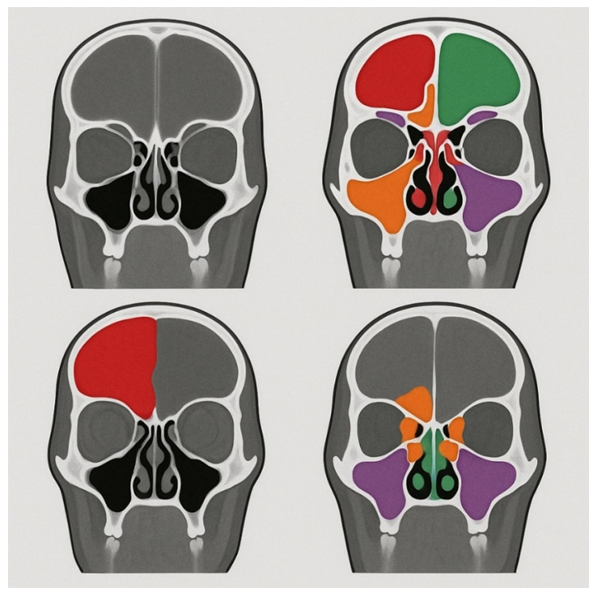
- This study used a retrospective approach, focusing on patients with paranasal sinus pathology and healthy patients who underwent examination at the Republican Research Center of Emergency Medicine from January 2024 to January 2025. The study included 160 people. All patients were divided into two groups. The main group (n=120) consisted of patients with confirmed paranasal sinus pathology. The control group (n=40) consisted of healthy volunteers with no signs of paranasal sinus disease according to clinical and radiological examination data.Patients with paranasal sinus pathology were divided into subgroups depending on the location of the pathological process and the number of images obtained: with frontal sinusitis — 36 patients; sinusitis was detected in 42 patients; sphenoiditis — in 30 patients; 12 patients were diagnosed with ethmoiditis (Fig. 1).
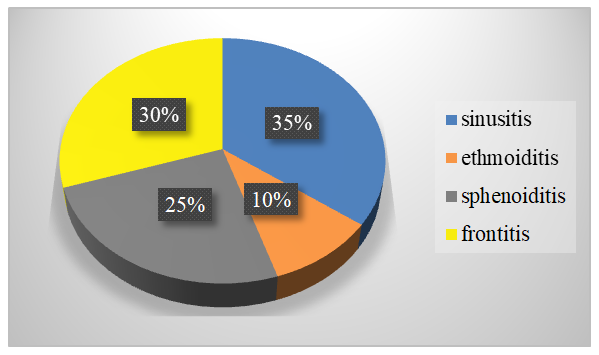 | Figure 1. Clinical distribution of patients in the main group |
|
3. Results
- When analyzing CT images of patients in the main group, typical radiological signs were identified for each subgroup of the disease.Tomograms showed diffuse or partial reduction in pneumatization of the frontal sinuses with the presence of homogeneous or cellular opacification corresponding to the accumulation of mucopurulent contents in patients with frontal sinusitis (n = 36), (Fig. 2).
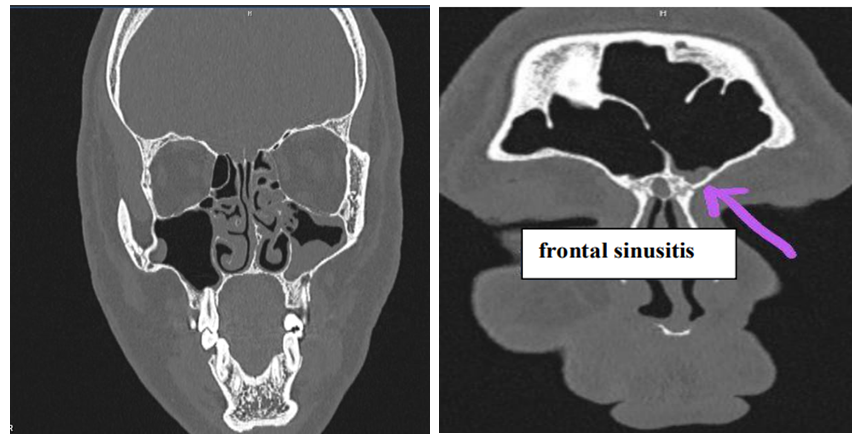 | Figure 2. Non-contrast multispiral computed tomography examination of the paranasal sinuses, performed with the patient in the supine position using scanning with a slice thickness of 1 mm |
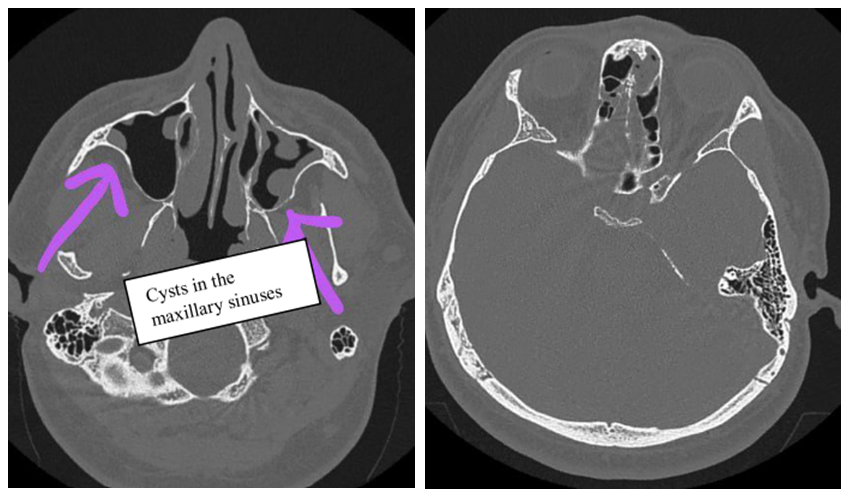 | Figure 3. Maxillary sinuses - in both maxillary sinuses there are cysts measuring up to 1.0x0.8x1.8 cm on the right, up to 1.5x1.0 cm on the left, with a density of +28+30 H units |
4. Discussion
- The developed model for classifying paranasal sinus pathologies based on deep learning algorithms demonstrated high diagnostic efficiency, providing a recognition accuracy of 85.8%, which significantly exceeds the indicators of specialists with low (71.7%), medium (78.4%) and even high (73.4%) qualifications. Such a result confirms the potential of artificial intelligence (AI) algorithms as a tool to support clinical decision-making in the analysis of computed tomography (CT) data.An important achievement of the presented model is its ability to accurately extract informative features and efficiently perform spatial analysis of images. It allows detecting pathological changes that may not be obvious during standard visual evaluation. It is especially relevant in cases of blurred or atypical clinical picture, when radiological diagnostics becomes crucial.A detailed analysis of the algorithm's performance in each clinical subgroup revealed characteristic features of its functioning and advantages over traditional CT image interpretation.When analyzing images of patients with frontal sinusitis (n = 36), the AI system demonstrated high sensitivity in detecting thickening of the frontal sinus mucosa and the presence of hypodense contents, which was particularly important in cases of partial sinus involvement, where the changes occupied less than half of the volume. The algorithm clearly defined the obliteration of the frontal nasal canal, which allowed predicting the risk of disease recurrence after treatment. When compared with the results obtained by physicians, it was found that the AI more often detected minimal inflammatory changes in the upper sinuses, which could remain unnoticed during a routine examination. In the group of patients with sinusitis (n=42), the algorithm reliably segmented areas of total and subtotal sinus darkening, determined fluid levels and mucosal hyperplasia. The use of radiological processing with noise suppression and contour enhancement contributed to a clearer visualization of the boundaries of polypous masses in the chronic process. The AI showed an advantage in assessing the involvement of adjacent structures, including the anterior ethmoidal cells, which increased the accuracy of determining the extent of the inflammatory process and influenced the choice of treatment tactics. When analyzing the sphenoid sinus, the algorithm demonstrated stable operation even in conditions of complex anatomy and small sizes of the studied area. The AI correctly identified mucosal thickening and the presence of pathological contents and also segmented the sphenoid-ethmoidal recess with high accuracy. It is particularly important that the system successfully detected minimal changes in the posterior ethmoid cells, which often remain unnoticed during routine examination due to their deep location. In the ethmoiditis group, the algorithm reliably segmented the affected cells of the ethmoid labyrinth, determined the degree of mucosal thickening and determined the presence of polypoid formations. In cases of combined forms of inflammation, the AI correctly displayed the involvement of adjacent sinuses, which facilitated a comprehensive evaluation of the disease. The algorithm's ability to differentiate hyperplastic changes from polyposis structures proved to be particularly valuable, which was important for planning surgical intervention.Comparative analysis between subgroups: regardless of the process localization, the algorithm demonstrated high reproducibility of results and stable segmentation of pathological areas. However, the greatest increase in accuracy compared to traditional analysis was observed in frontal and sphenoid pathologies, which may be underestimated in conventional interpretation due to difficult access for visualization or an unclear clinical picture.Thus, the integration of AI into CT analysis of the paranasal sinuses not only automates the process of pathology recognition, but also provides additional value in complex anatomical conditions, minimal changes and multisinusitis.An analysis of the use of the AI system in diagnosing paranasal sinus diseases revealed the following key advantages:1. Increased diagnostic accuracy — sensitivity in detecting inflammatory changes reached 95–97%, which is higher than with traditional analysis (88–90%). It is especially important in early diagnostics and treatment strategy choice.2. Reduction of description time - automatic preliminary segmentation and protocol generation allowed to reduce the physician's time costs by 30-40%, which increases the throughput of the radiology room and reduces the patient's waiting time for the conclusion.3. Standardization of conclusions - the formation of descriptions according to standardized templates reduced interobserver variability and ensured comparability of data between different specialists and medical institutions.4. Detection of minimal changes — the use of radiological processing with noise suppression and contrast optimization allowed to detect early stages of inflammatory and neoplastic processes, minimal polyposis formations and thickening of the mucous membrane.5. Educational value — the algorithm can be used as a training tool for young professionals, allowing them to compare their conclusions with a benchmark analysis performed by the AI, which accelerates the process of professional growth.The results obtained are consistent with data from foreign studies, which note that modern deep learning algorithms demonstrate accuracy in recognizing paranasal sinus pathologies in the range of 83–90%, and in some cases surpass experienced specialists in a number of indicators related to the quantitative evaluation of inflammatory changes.At the same time, despite the obvious advantages, the introduction of the AI into clinical practice requires solving a number of problems. Standardization of CT examination protocols is necessary to ensure data reproducibility, training of physicians in the use of digital diagnostic systems, as well as multicenter clinical trials to validate algorithms on local patient samples. An important area of development is the integration of the AI models into comprehensive diagnostic platforms, including high-resolution CT/MRI and digital radiological processing modules, which will allow to achieve maximum efficiency in image analysis.Thus, the results of this study demonstrate that artificial intelligence algorithms can efficiently complement the work of radiologists, expanding their diagnostic capabilities, increasing the accuracy and speed of analysis and contributing to the standardization and objectification of descriptions.
5. Conclusions
- The study demonstrated that the integration of artificial intelligence and digital radiological processing technologies into the diagnostics of paranasal sinus diseases is a promising direction for the development of modern radiological diagnostics. The use of deep learning algorithms in the analysis of computed tomography data:• improves the accuracy and reproducibility of diagnostic results;• reduces image interpretation time, increasing physician efficiency;• allows to detect minimal pathological changes that may not be obvious during traditional visual analysis;• provides standardization of descriptions and conclusions, reducing interobserver variability.The results obtained confirm that artificial intelligence systems can serve as a reliable tool for supporting clinical decision-making, complementing the physician's experience but not replacing him. The greatest effect is achieved through the combined use of highly informative imaging methods (CT/MRI), digital radiological processing modules, and automatic segmentation and classification algorithms.Further development of this technology involves adapting algorithms to national medical image databases, validating them in multicenter studies, as well as their integration into everyday clinical practice. It will allow to improve the quality of diagnostics, optimize patient routing and bring the healthcare system closer to the principles of personalized medicine.The results of the study open up broad opportunities for further improvement of artificial intelligence technologies in the diagnostics of paranasal sinus diseases. Promising areas include the development of specialized algorithms for detecting rare and complex forms of pathology, the integration of multicenter databases to increase the versatility of models, and the creation of a unified software platform combining visualization and automatic segmentation modules and the formation of standardized protocols. The implementation of these tasks will not only allow to improve clinical diagnostic indicators, but also to reduce the workload on specialists, optimizing the use of healthcare resources and expanding the availability of high-tech medical care.
Conflict of Interests
- The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGEMENTS
- The authors express their gratitude to the management of the multidisciplinary clinic of Republican Research Center of Emergency Medicine for the material provided for our study.
Ethical Approval and Consent to Participate
- Our institution's research ethics committee does not require review or approval of case reports.Our investigation is conducted in accordance with the World Medical Association's Code of Ethics (Declaration of Helsinki).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML