-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(9): 2971-2975
doi:10.5923/j.ajmms.20251509.27
Received: Aug. 22, 2025; Accepted: Sep. 17, 2025; Published: Sep. 20, 2025

Advanced Diagnostic Strategies for Cervical Intraepithelial Neoplasia: Role of Genetic Polymorphisms
Akhmedova M. O.
Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan
Correspondence to: Akhmedova M. O., Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study was conducted on 86 patients aged 30–59 years with cervical intraepithelial neoplasia and 14 patients with cervical cancer. Background: The control group consisted of 92 healthy women without cervical pathology. Methods: The characteristics of the MKI67 (rs10764749) polymorphic gene were analyzed using allele-specific PCR. In healthy women, genotype distribution was assessed according to the Hardy–Weinberg equilibrium, and comparative control analysis confirmed RHV compliance (p>0.05). Results: Functional analysis of MKI67 (rs10764749) in patients with CIN 2 and healthy women of the main group revealed a statistically significant association between this genetic marker and the risk of CIN 2 development. Conclusions: Thus, the results of the analysis of the structural and functional features of the MKI67 gene (rs10764749), conducted in patient groups and in the control group, indicate the presence of a statistically significant role of this genetic marker in increasing the risk of cervical intraepithelial neoplasia.
Keywords: Cervical intraepithelial neoplasia, Human papillomavirus, MKI67 (rs10764749)
Cite this paper: Akhmedova M. O., Advanced Diagnostic Strategies for Cervical Intraepithelial Neoplasia: Role of Genetic Polymorphisms, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 2971-2975. doi: 10.5923/j.ajmms.20251509.27.
1. Introduction
- The primary causal factor in the development of cervical intraepithelial neoplasia (CIN) in women is considered to be infection with high-risk human papillomavirus (HPV) [1]. HPV infection and the integration of its genome into the chromosomal apparatus of cervical epithelial cells serve as an early key mechanism in the progression of cervical tumor lesions [6,7]. It is reported that the pathogenic effect of HPV is mediated by the viral oncoproteins E6 and E7, which are responsible for the initial changes in epithelial cells. These oncoproteins contribute to the alteration of the activity of numerous genes involved in DNA repair processes, cell proliferation, growth factor activation, and angiogenesis [3].MKI67 (rs10764749) is a genetic marker of cell proliferation, whose prognostic value has been demonstrated in the development of various neoplastic processes (including prostate carcinoma, brain tumors, and breast cancer) [4,8]. Furthermore, recent studies indicate that the MKI67 gene may serve as a potential marker for the progression of cervical intraepithelial lesions [2,5].
2. Material and Methods
- A total of 100 Uzbek women aged 30 to 59 years were examined as the main study group, which was divided into two subgroups. The first subgroup included 46 (46%) patients who tested positive for high-risk HPV types, while the remaining 40 (40%) patients tested negative for HPV and 14 (14%) cervical cancer. The control group consisted of data from 92 practically healthy women with a negative HPV PCR test result and NILM findings from liquid-based cytology. Inclusion criteria for the study were based on the results of general clinical and gynecological examinations, including cytological analysis. Each patient underwent a comprehensive examination according to the protocol, which included the collection of clinical and anamnestic data, extended colposcopy, liquid-based cytology, quantitative polymerase chain reaction with real-time detection (PCR-RT), pelvic ultrasound, histological examination of biopsy samples from pathological areas of the cervix, and analysis of the genotypic variant of the MKI67 (rs10764749) gene. Collection of Biological Material for Molecular-Genetic Research. For molecular-genetic studies, blood samples were collected from the cubital vein in dry plastic tubes with a volume of 4 ml, containing 0.5 ml of 0.5 M EDTA (pH=7.8) from patients with CIN 2 HPV (-) (n=40), CIN 2 HPV (+) (n=46), and the control group (n=92). Polymerase Chain Reaction (PCR) for DNA Synthesis in Molecular-Genetic Analysis.A sample of genomic DNA (50–200 ng) was added to a 25.0 µl reaction mixture containing 0.67 mM Tris-HCl (pH 8.8 at 25°C), 16.6 mM (NH4)2SO4, 1–6.7 mM MgCl2, 6.7 µM EDTA, 10 mM 2-mercaptoethanol, 170.0 µg BSA, a mixture of four main deoxynucleotide triphosphates (0.8 mM each), 0.2 U/µl of thermostable DNA polymerase ("SibEnzyme," Novosibirsk), and oligonucleotide primers at the final concentration. The specificity of amplification after PCR completion, as well as the quantity of the obtained amplicon, was verified using electrophoresis. If necessary, hydrolysis of the amplified DNA fragments was performed following the recommendations of the manufacturer ("SibEnzyme," Novosibirsk). The frequency of allele and genotype variants (f) was calculated using the formulas: f=n/2N and f=n/N. The prognostic efficiency (AUC classifier) of the genetic markers studied was determined using the standard formula: AUC=(Se + Sp) /2. The correspondence of genotype frequencies to Hardy-Weinberg equilibrium was evaluated using the χ² test. Differences in allele and genotype frequencies were assessed using the χ² test and Fisher’s exact test. The odds ratio and 95% confidence interval were calculated using the OpenEpi software package (ver. 9.3).
3. Results and Discussion
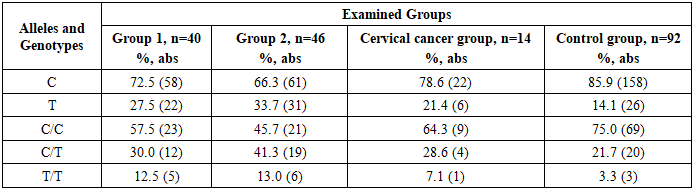
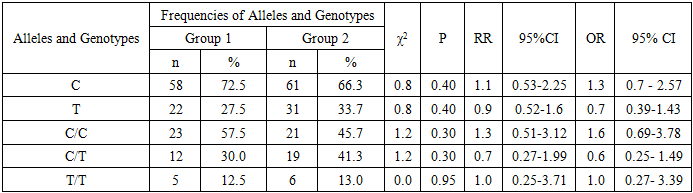
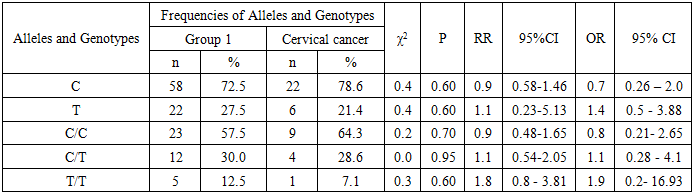
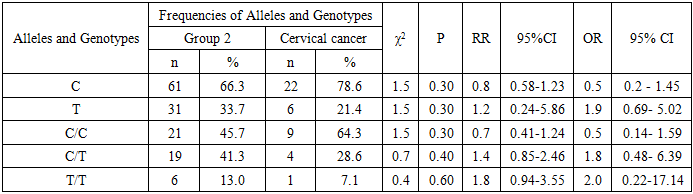
- The structure of the MKI67 gene (rs10764749) in groups of patients with CIN 2, depending on negative or positive HPV test results, was characterized by the observed frequencies of the dominant C and minor T alleles at 72.5% and 66.3%, and 27.5% and 33.7%, respectively. The dominant genotype C/C was identified in 57.5% and 45.0% of patients, while the heterozygous C/T and the rare homozygous T/T genotypes were found in 30.0% and 41.3%, and 12.5% and 13.0% of cases, respectively, in the two studied groups of CIN 2 women.Of particular interest was the study of this gene among women with cervical cancer, which revealed allele frequencies of C (78.6%) and T (21.4%), while the genotypes C/C, C/T, and T/T were distributed as 64.3%, 28.6%, and 7.1%, respectively.In a comparative structural analysis of the MKI67 (rs10764749) gene in the control group, consistently higher frequencies of the main variants were observed: the C allele (85.9%) and the homozygous genotype C/C (75.0%), which were accompanied by lower proportions of unfavorable variants — the T allele (14.1%), as well as the C/T (21.7%) and T/T (3.3%) genotypes compared with patients with CIN 2 (Table 1).
|
|
|
|
|
|
|
4. Conclusions
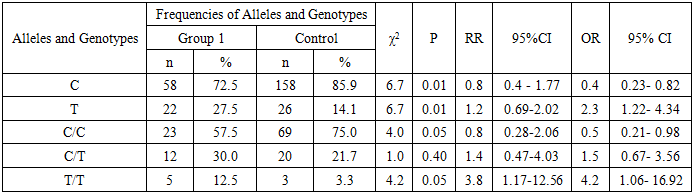
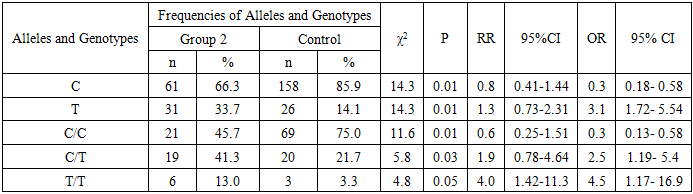
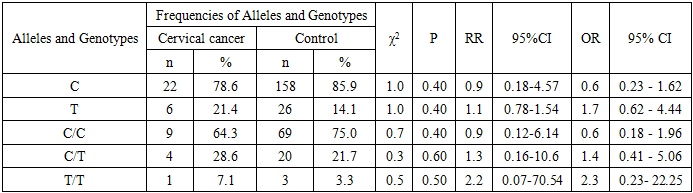
- Thus, the results of the analysis of the structural and functional features of the MKI67 gene (rs10764749), conducted in patient groups and in the control group, indicate the presence of a statistically significant role of this genetic marker in increasing the risk of cervical intraepithelial neoplasia.Thus, the study of the structural and functional characteristics of the genetic markers MKI67 (rs10764749) in comparison with healthy individuals yielded the following results: § The role of unfavorable loci of the biomarkers MKI67 (rs10764749) (T – χ²=6.7; P=0.01; OR=2.3 and T/T – χ²=4.2; P=0.05; OR=4.2) has been proven in the development of moderate cervical intraepithelial neoplasia (CIN) of the stratified squamous epithelium of the cervix in HPV-negative patients.§ The role of unfavorable loci of the genetic markers MKI67 (rs10764749) (T – χ²=14.3; P=0.01; OR=3.1; C/T – χ²=5.8; P=0.03; OR=2.5 has been proven in the development of moderate cervical intraepithelial neoplasia (CIN) of the stratified squamous epithelium of the cervix in HPV-positive patients.§ Reliable data were obtained showing an independent association between the development of cervical cancer (CC) and unfavorable loci of the genetic markers, while no independent contribution of the MKI67 (rs10764749) gene was found (χ²<3.84; P>0.05).§ Differences in the distribution of polymorphic loci of the genes MKI67 (rs10764749) between patients of the 1st and 2nd groups (χ²<3.84; P>0.05), the 1st group and the cervical cancer group (χ²<3.84; P>0.05), as well as between the 2nd group and the cervical cancer group (χ²<3.84; P>0.05), did not reach a statistically significant level.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML