-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(9): 2948-2951
doi:10.5923/j.ajmms.20251509.22
Received: Aug. 5, 2025; Accepted: Aug. 26, 2025; Published: Sep. 20, 2025

Clinical, Morphological and Morphofunctional Features Oviral Endometriosis
Fayzulloyev Aziz Akhmedovich1, Oripova Feruza Shopulatovna2, Dustova Nigora Khahramonovna2
1PhD Student, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
2Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
Correspondence to: Fayzulloyev Aziz Akhmedovich, PhD Student, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Endometrioid ovarian lesions are the most common form of genital endometriosis [1]. Until now, the mechanisms of development of ovarian endometriosis (OE) are unclear, the features of its morphological and morphofunctional characteristics, the reasons for frequent relapse of the disease, the lack of effectiveness of conservative therapy, including hormonal therapy, have not been sufficiently studied. The aim of the study is to conduct a clinical and morphological analysis of ОE taking into account its various variants and morphofunctional forms. Clinical data and results of morphological examination of surgical material of 139 patients with ovarian endometriosis were analyzed. The average age of patients was 38.6 ± 0.72 years, while 38.85% of patients were under 35 years old; 39.57% - from 36 to 45 years old; 21.58% - over 46 years old. Upon admission to the clinic, the examined patients presented active complaints related to various manifestations of pain syndrome and menstrual cycle disorders. 50.4% of patients reported periodic moderate pain, noticeable discomfort during most of the menstrual cycle, 19.4% of patients reported periodic severe pain during the menstrual cycle, and 4.3% of women reported pain before menstruation. During the surgical intervention, it was found that 64.7% of patients had unilateral ovarian lesions, more often the left one (41.7%), the remaining 35.3% had bilateral lesions. An increase in the size of the ovary due to the formation of a cyst up to 5 cm in diameter was observed in 37.4% of cases, 5–10 cm in diameter in 30.9%, and more than 10 cm in diameter in 28.8%. Small point endometrioid heterotopias on the surface.
Keywords: Ovarian endometriosis, Endometrioid ovarian cyst, Clinical and morphological variants, Morphofunctional forms
Cite this paper: Fayzulloyev Aziz Akhmedovich, Oripova Feruza Shopulatovna, Dustova Nigora Khahramonovna, Clinical, Morphological and Morphofunctional Features Oviral Endometriosis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 2948-2951. doi: 10.5923/j.ajmms.20251509.22.
Article Outline
1. Introduction
- Until now, the mechanisms of development of ovarian endometriosis (OE) are unclear, the features of its morphological and morphofunctional characteristics, the reasons for frequent relapse of the disease, the lack of effectiveness of conservative therapy, including hormonal therapy, have not been sufficiently studied. [1]. There is a lot of contradictory data on the morphogenesis of endometriosis in general and its macrocystic variant in particular; the issue of histo- and morphogenesis of “chocolate” cysts and their belonging to endometriosis is debated; there is no clear classification of possible topographic and histological variants; there are no data on the study and determination of morphofunctional features [2]. A distinction is made between the superficial form of ovarian endometriosis and deep forms - nodular and cystic [3]. The cystic form of ovarian endometriosis is also called ovarian endometriomas [4]. It has been established that large endometrioid cysts often develop in association with functional luteal or follicular cysts. This has led to the assumption that endometriomas are secondary formations that arise from fusion with functional ovarian cysts. From the above positions, “small” forms of endometriosis and endometrioid ovarian cysts with a diameter of up to 30 mm should be classified as “true” (primary) endometriosis, and endometrioid cysts with a diameter of over 40–50 mm are probably preceded by ovarian retention formations [5].
2. The Aim of the Study
- To conduct a clinical and morphological analysis of ОE taking into account its various variants and morphofunctional forms.
3. Materials and Methods
- Clinical data and results of morphological examination of surgical material of 139 patients with ovarian endometriosis were analyzed. The average age of patients was 38.6 ± 0.72 years, while 38.85% of patients were under 35 years old; 39.57% - from 36 to 45 years old; 21.58% - over 46 years old. The endometrioid nature of ovarian lesions at the preoperative stage during clinical examination of patients was diagnosed in only 54 of 139 patients (38.9%). The endometrioid nature of ovarian lesions at the preoperative stage during clinical examination of patients was diagnosed in only 54 of 139 patients (38.9%). Indications for surgical treatment were: ovarian cystoma, uterine myoma, adenomyosis, combination of adenomyosis with uterine myoma. The scope of surgical treatment was determined by the age of the patients, the nature of the pathology of the uterine appendages, and concomitant pathology of the uterus. The majority of patients (66.9%) were operated on laparoscopically in the volume of cystectomy or adnexectomy, 33.1% - laparotomic in the volume of supravaginal amputation or extirpation of the uterus with appendages. The clinical part of the work included the study of anamnestic data, general clinical, gynecological and instrumental methods of research. Morphological examination was performed with subtotal cutting of surgical material, sections were stained with hematoxylin and eosin, picro-fuchsin according to Van Gieson method.Statistical processing of the obtained results was carried out using commonly used methods of parametric and non-parametric statistics on a PC using a standard software package of applied statistical analysis (Statistica for Windows v.6.0).
4. Results and Discussion
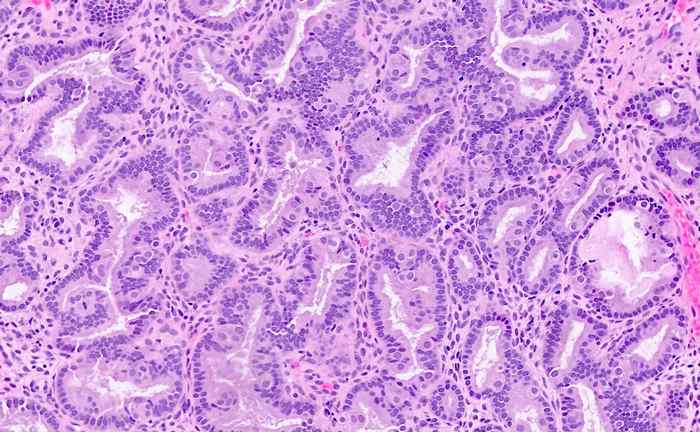
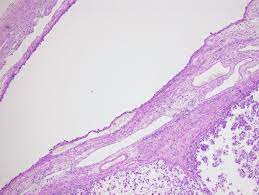
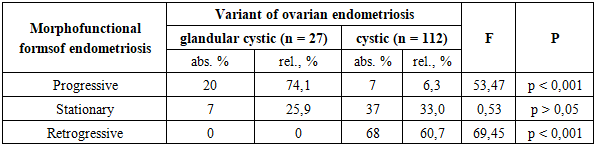
- Upon admission to the clinic, the examined patients presented active complaints related to various manifestations of pain syndrome and menstrual cycle disorders. 50.4% of patients reported periodic moderate pain, noticeable discomfort during most of the menstrual cycle, 19.4% of patients reported periodic severe pain during the menstrual cycle, and 4.3% of women reported pain before menstruation. At the same time, the majority of patients (64.0%) reported increased pain before and during menstruation. Dysmenorrhea was reported by 103 of 139 patients (74.1%): menstrual pain was moderate (43.2%) or severe (28.1%) in most women, and weak only in 2.9%. Some patients noted menstrual cycle-related pain during defecation, tenesmus (10.8%), and pain during urination (4.3%). Dyspareunia was reported by 30.2% of patients, and most of them had moderate (17.3%) or mild (8.6%) pain during intercourse, and rarely severe (4.3%). Pain syndrome in EO was characterized by the presence of pain irradiation in various areas (46.8%): to the lumbar region (36.0%), to the rectum (23.0%), to the sacral (18.0%). In 24.3% of patients with EO, pain syndrome was accompanied by various vegetative disorders: nausea bothered 23.0% of women, vomiting was in 7.9%, loss of consciousness in 2.9%. Menstrual cycle disorders were noted in the anamnesis of 40.3% of women. While the regular menstrual cycle was maintained in most patients (80.6%), the most frequent manifestations of its disorder were heavy menstruation (40.3%), dark brown spotting from the genital tract before and after menstruation (39.5%), and intermenstrual bleeding with a normal cycle (11.5%). When analyzing the gynecological anamnesis data, it was found that patients with EP are characterized by a relatively late age of menarche, on average, it was 13.26 ± 4.5 years. In most patients, the menstrual cycle was established immediately and was regular (96.4%). 52.5% of women assessed the nature of discharge during menstruation as moderate, 47.5% - as heavy. In the anamnesis, 65.5% of patients had an indication of 1-2 births, 9.4% had 3 or more births, 59.0% had 1-2 abortions, 22.3% had 3 or more abortions. In the anamnesis, 8.6% of patients had primary infertility, 7.2% had secondary infertility, and 11.5% of women had spontaneous abortions. Separate diagnostic curettage of the cervical canal and uterine cavity at the preoperative stage were performed in 25.2% of patients.Histological examination of scrapings revealed dyshormonal glandular hyperplasia of the endometrium in 15.8% of cases, and endometrial polyp in 7.9%. Analysis of clinical and anamnestic data allowed us to detect various somatic pathologies in patients with EO: 9.4% had breast diseases, 10.1% had metabolic-endocrine dystonia, 19.4% had varicose veins, 14.4% had kidney and urinary tract diseases, 27.3% had frequent colds, and 18.0% had a tendency to allergic reactions. During a bimanual gynecological examination, formations of a hard-elastic consistency were palpated in the area of the appendages, sensitive to palpation in 60.4% of patients, with limited mobility in 75.5%. During ultrasound examination of the pelvic organs, an endometrioid ovarian cyst was diagnosed in 32.4% of patients, an ovarian cyst without specifying its nature in 31.7%, and a combination of uterine pathology (uterine fibroids and/or adenomyosis) with an ovarian cyst in 22.3%. During the surgical intervention, it was found that 64.7% of patients had unilateral ovarian lesions, more often the left (41.7%), the remaining 35.3% had bilateral lesions. An increase in the size of the ovary due to the formation of a cyst with a diameter of up to 5 cm was observed in 37.4% of cases, with a diameter of 5–10 cm - in 30.9%, and more than 10 cm in diameter - in 28.8%. Small point endometrioid heterotopias on the surface of the ovaries were detected in 2.9% of cases. Most patients with ovarian cysts were characterized by the presence of an adhesive process in the small pelvis: minor adhesive process in the area of the uterine appendages without involvement of the intestine was diagnosed in 48.9% of patients, pronounced adhesive process in the area of the uterine appendages with partial involvement of the intestine - in 19.4%, widespread adhesive process with involvement of all pelvic organs - in 7.9%. The contents of the cysts in most women (94.2%) were assessed as tar-like, thick, "chocolate" color, less often as liquid, dark red (5.7%). Microperforations of the cysts with partial emptying of contents into the abdominal cavity were detected in 21.6% of cases. In addition to ovarian lesions, endometrioid heterotopias during abdominal cavity revision were found on the parietal peritoneum of the small pelvis, on the serous cover of the uterus - 4 observations each (2.9%), on the fallopian tubes, urinary bladder - 3 observations each (2.2%), broad ligament of the uterus - 5 observations (3.4%). At the same time, in 14 patients (10.1%), a combination of endometrioid ovarian cancer with two or more localizations of endometriosis on the pelvic organs and peritoneum was detected. Morphological examination of the removed ovaries revealed macro- and microscopic morphofunctional heterogeneity of the studied observations. Of the 139 patients, 112 (80.6%) had a macrocystic form of the process, 25 (17.98%) had a combination of a cyst with glandular-stromal endometrioid structures in the ovarian tissue outside the endometrioid cyst, and 1.44% had glandular-stromal endometrioid foci without cyst formation.According to this, the morphological characteristics of the EP varied significantly, which was the basis for identifying three variants of the EP in the study - glandular-cystic, glandular and cystic.
|
5. Conclusions
- Thus, the conducted study revealed a significant diversity of clinical manifestations of EP and its morphological features. The clinical course of EP is characterized by various manifestations of pain syndrome: pain during most of the menstrual cycle, increasing on the eve and/or during menstruation, dysmenorrhea, dyspareunia; less often, patients with EP noted a violation of the menstrual cycle by the type of hypermenorrhea. Morphological examination of the surgical material revealed a diversity of the histological structure of EP, which corresponds to three variants - glandular, glandular-cystic and cystic and three morphofunctional forms - growing, stationary, regressing.Morphological features of the glandular cystic variant of EO confirm the opinion about the high frequency of relapses in the "active" form of endometrioid ovarian lesions, which is its analogue. The existence of various forms of EO must be taken into account when choosing a rational tactic for managing patients in the postoperative period to prevent relapses. A comparative analysis of our own surgical material allows us to believe that the macro-microscopic variants and morphofunctional forms of EO represent successive stages of the disease, stages of its evolution, leading to the formation of a "chocolate" cyst due to the chronic wave-like course of the process. Apparently, the following chronology of stages occurs in EO. The onset of the disease is associated with the appearance of a glandular-stromal focus of EO in the ovary, with an active state of the epithelial and stromal components. Being similar to endometrial tissue, it enters the phases of proliferation, secretion with subsequent expansion of the glands with accumulation of secretion, hemorrhages, which entails macrocystic transformation, atrophy of the epithelium, its gradual loss. Good vascularization of the cytogenic stroma, its participation in cyclic processes determine the possibility of hemorrhages not only in the lumen of the glands, but also in the cytogenic stroma, which, in combination, contributes to its fibrosis and cystic transformation of the glands. Thus, the cyclicity of hormonal changes, which have a regular, repetitive nature, forms a vicious circle: circulatory disorder - organization- fibrosis - neoangiogenesis - circulatory disorder. In addition, perifocal sclerosis with the development of a fibrous wall occurs. The tendency towards macrocystic transformation in ovarian cysts is largely determined by the anatomical features of the ovary and the topography of the process in the ovary itself. Glandular-stromal foci of ovarian cysts at the initial stage of the development of pathology in most cases are detected only in the cortex of the ovaries, but then, as the disease progresses and a “chocolate” cyst is formed, the intramural part of the ovary is involved. The progression of ovarian ovarian cancer can proceed in three directions: an increase in the formed cyst with the activation of endometrioid heterotopias existing in the wall, the development of new endometrioid heterotopias outside the cyst in the ovarian tissue, of particular importance is spread through the peritoneum of the small pelvis with possible complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML