Mamajonov Ikboljon Maribjonovich1, Makhkamov Nosirjon Jurayevich2
1Independent Researcher, Andijan State Medical Institute, Andijan, Uzbekistan
2Associate Professor, Doctor of Medical Sciences, Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Mamajonov Ikboljon Maribjonovich, Independent Researcher, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This scientific article presents a comparative clinical and pathomorphological analysis of tuberculous spondylitis in cases associated with COVID-19 infection and those without it. Clinical observations revealed that tuberculous spondylitis complicated by COVID-19 was characterized by more pronounced general intoxication symptoms, more severe pain syndrome, and a more rapid progression of motor function limitations. Pathomorphological analysis demonstrated that cases of tuberculous spondylitis associated with COVID-19 showed more extensive neutrophilic infiltration, foci of caseous necrosis, signs of vasculitis, and the proliferation of fibrous tissue. Furthermore, on the microscopic level, increased vascular damage and immune complex alterations were noted under the influence of COVID-19. These findings play a significant role in better understanding the course of tuberculous spondylitis, improving differential diagnostic criteria, and developing more effective treatment strategies.
Keywords:
Tuberculous spondylitis, COVID-19, Clinical features, Pathomorphology, Caseous necrosis, Vasculitis, Immune complexes, Spinal tuberculosis, Differential diagnosis
Cite this paper: Mamajonov Ikboljon Maribjonovich, Makhkamov Nosirjon Jurayevich, Comparative Clinical and Pathomorphological Analysis of Tuberculous Spondylitis with and without the Influence of COVID-19, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 2888-2892. doi: 10.5923/j.ajmms.20251509.09.
1. Introduction
In recent years, the systemic impact of COVID-19 on the human body particularly its effect on the immune system, pro-inflammatory cytokine activity, and microcirculatory disturbances — has significantly altered the course of many chronic diseases [1,2]. This is especially relevant in the case of tuberculosis (TB), where coinfection with COVID-19 appears to exacerbate disease progression. In patients with tuberculous spondylitis, the presence of COVID-19 is associated with more severe clinical symptoms, such as intensified pain, systemic intoxication, and decreased spinal mobility [3,4].Pathomorphologically, COVID-19-positive TB spondylitis cases demonstrate more aggressive features, including pronounced neutrophilic infiltration, vasculitis, caseous necrosis, and widespread fibrosis within spinal tissues [5,6]. Furthermore, SARS-CoV-2 infection leads to endothelial dysfunction, hypercoagulation, and immune-complex-mediated damage, which significantly worsens the course of tuberculous lesions [7–9].In Uzbekistan, an increasing number of TB cases among both younger and older populations, particularly in the post-COVID period, has emphasized the need for comprehensive investigation of this comorbidity [10,11]. Comparative clinical and pathomorphological analysis of tuberculous spondylitis with and without the influence of COVID-19 is essential for understanding the immune-mediated mechanisms and for optimizing diagnostic and treatment strategies [12,13].
2. Purpose of Research
The main purpose of this study is to conduct a comparative analysis of the clinical and pathomorphological characteristics of tuberculous spondylitis with and without the influence of COVID-19 infection, to identify the differences between these two conditions, and to improve differential diagnostic and therapeutic approaches that are essential for clinical practice.
3. Materials and Methods
This research was conducted on histological specimens obtained from 150 patients diagnosed with tuberculous spondylitis at the Andijan Regional Center for Phthisiology and Pulmonology during the period from 2019 to 2023. Tissue samples were fixed in 10% neutral buffered formalin following standard histoprocessing protocols, embedded in paraffin blocks, and sectioned into 4–5 µm thick slices using a microtome.Several classical histological staining techniques were applied to enable a comprehensive assessment of tissue architecture and pathological changes. Hematoxylin and eosin (H&E) staining was used to assess general tissue architecture and cellular morphology. The Van Gieson method was applied to highlight areas of caseous necrosis and granulomatous inflammation, while Masson’s trichrome staining was utilized to visualize collagen fibers and assess the extent of fibrosis.A detailed morphometric and comparative pathomorphological analysis was carried out. All cases were categorized into two groups: those with confirmed concurrent COVID-19 infection and those without. Morphometric parameters such as the extent of fibrotic tissue proliferation, area of necrosis, degree of neutrophilic infiltration, and presence of vasculitic changes were quantitatively assessed using digital image analysis software calibrated for histological evaluation. The collected data were statistically analyzed to identify significant differences between the two groups and to better understand the modifying influence of COVID-19 on the pathological course of tuberculous spondylitis.
4. Results and Discussion
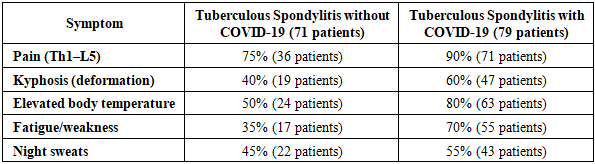
The results of this study clearly demonstrated the clinical, pathomorphological, and morphometric differences between cases of tuberculous spondylitis associated with COVID-19 and those without. In particular, the analysis of clinical symptomatology revealed that the disease progresses more severely and rapidly under the influence of COVID-19 infection. The primary symptoms related to lesions in the thoracic (Th1–Th12) and lumbar (L1–L5) segments of the spine—namely, pain, kyphosis, elevated body temperature, general fatigue, and night sweats—were thoroughly analyzed.A total of 150 patients were included in the study. Among them, 71 patients had tuberculous spondylitis associated with COVID-19 infection, while the remaining 79 patients had tuberculous spondylitis without COVID-19 involvement. The table below presents the differences in the clinical frequency of these symptoms between the two groups (see Table 1).Table 1. Impact of COVID-19 Infection on Clinical Symptoms of Tuberculous Spondylitis
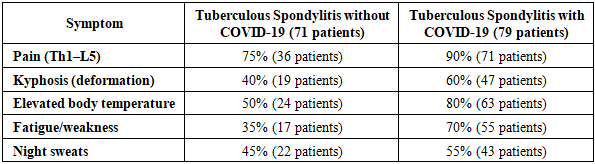 |
| |
|
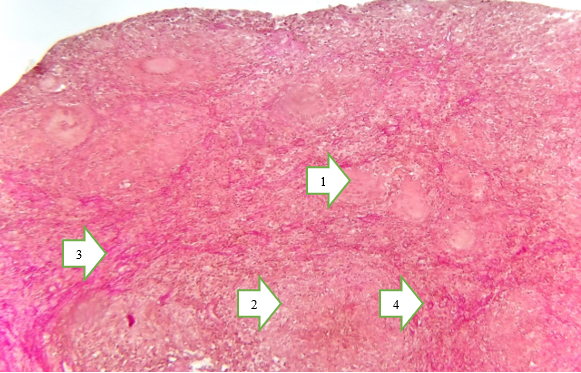
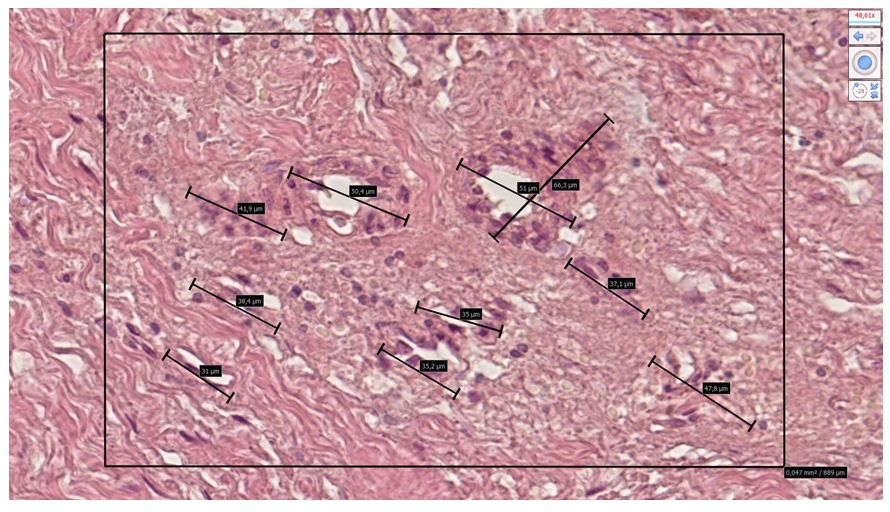
Analysis of the clinical data indicates that tuberculous spondylitis presents with significantly more severe manifestations under the influence of COVID-19 infection. Notably, pain was observed in 90% of patients with concurrent COVID-19, which can be attributed to the heightened activity of inflammatory mediators and an intensified immune response. The 15% increase in pain incidence reflects the enhanced progression of necrotic, fibrotic, and vasculitic changes within the affected tissues. Furthermore, general fatigue and weakness were reported in 70% of patients in the COVID-19 group, representing a 35% increase compared to patients without COVID-19. This highlights the detrimental effect of SARS-CoV-2 infection on overall metabolic function and immune system stability, and suggests the presence of a pronounced systemic intoxication syndrome. An elevated body temperature was recorded in 80% of COVID-19-associated cases, showing a 30% difference from the non-COVID group. This hyperthermia indicates that the tuberculous process was occurring in an active inflammatory phase. Kyphotic spinal deformity was observed in 60% of patients with COVID-19, which is 20% higher than in those without the infection. This finding suggests that the granulomatous and fibrotic processes associated with tuberculosis progress more rapidly and severely in the presence of COVID-19, leading to accelerated damage of vertebral structures. Night sweats were reported in 55% of COVID-19-infected patients—10% more than in the comparison group—likely due to neuroimmune alterations, hypersensitivity of the hypothalamic centers, and overactivation of the autonomic nervous system. The increased degree of fibrosis played a key role in the earlier manifestation of both kyphosis and fatigue. Additionally, endothelial damage resulting from vasculitis and immune complex deposition may explain the more frequent occurrence of fever and night sweats. In summary, COVID-19 infection not only intensifies the clinical course of tuberculous spondylitis but also deepens tissue damage, as confirmed by both clinical and pathomorphological evidence.Comparative Pathomorphological Analysis of Tuberculous Spondylitis with and without COVID-19.The pathomorphological study of tuberculous spondylitis revealed significant differences influenced by the presence of COVID-19 infection. In cases without COVID-19, the morphological pattern was characterized by classical chronic granulomatous inflammation. Well-formed granulomas were observed in vertebral tissues, featuring central caseous necrosis surrounded by epithelioid cells and multinucleated giant cells of the Pirogov–Langhans type. The inflammatory process was localized, with clearly demarcated zones of perifocal fibrosis and sclerosis.In contrast, COVID-19-associated cases exhibited diffuse, rapidly progressing morphological changes. The structure of granulomas appeared disorganized, with a reduced number of epithelioid cells and poorly developed giant cells. Caseous necrosis occurred early and extensively, leading to widespread tissue destruction without clear boundaries. The inflammatory process was dominated by diffuse lymphohistiocytic infiltration, and extensive development of paraspinal abscesses was frequently observed.Moreover, COVID-19-associated cases demonstrated early-onset vasculitic changes and microangiopathic features such as thrombosis, ischemia, and vascular hyalinization. These findings are likely related to either immune hyperactivity or immunosuppression caused by SARS-CoV-2, resulting in a highly active inflammatory response.Overall, the comparative pathomorphological analysis indicates that COVID-19 significantly alters the morphogenesis of tuberculous spondylitis. It leads to disrupted granulomatous formation, expansion of necrotic zones, and accelerated fibrotic and vascular alterations. These morphological differences directly influence the clinical course of the disease and necessitate tailored therapeutic strategies (Figure 1-2).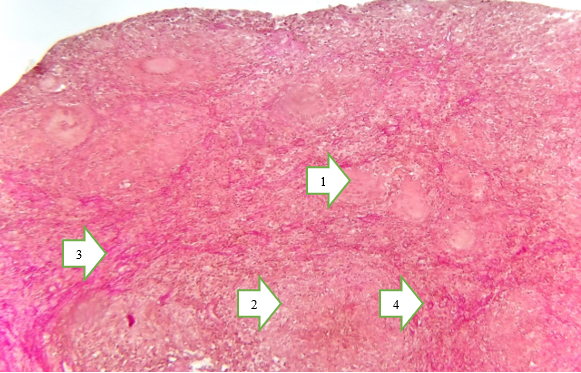 | Figure 1. Under the influence of COVID-19. Pirogov–Langhans giant cells (1). Caseous necrosis (2). Fibrous connective tissue structures surrounding the necrotic area (3). Vascular wall sclerosis (4). Size: 4×10. Stain: Van Gieson |
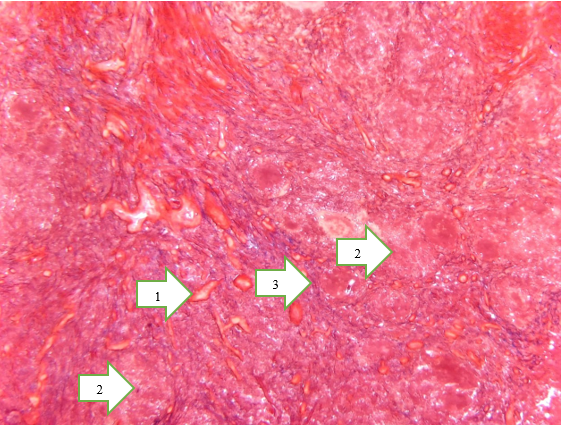
 | Figure 2. Without the influence of COVID-19. Sclerosis of the vascular wall and collagen fibers (1). Foci of necrosis (2). Collagen fibers surrounding the necrotic area (3). Magnification: 4×10. Size: 4×10. Stain: Van Gieson |
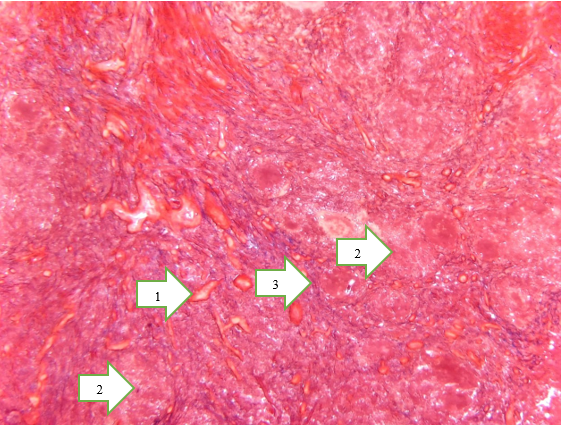
Changes Observed in Bone Tissue During the Post-COVID-19 Period:In post-COVID-19 tuberculous spondylitis, productive arteriolosclerosis was observed in small-caliber arteries of the bone tissue, along with the accumulation of caseous necrosis and sparse fibrous connective tissue components around the vascular walls due to the influence of Mycobacterium tuberculosis. This condition typically manifests as systemic vasculitis in small-caliber arteries, characterized morphometrically by thickening of the vessel walls, perivascular accumulation of numerous epithelioid cells, a high number of immature Pirogov–Langhans giant cells, and extensive foci of lymphocytic infiltration (Figure 3).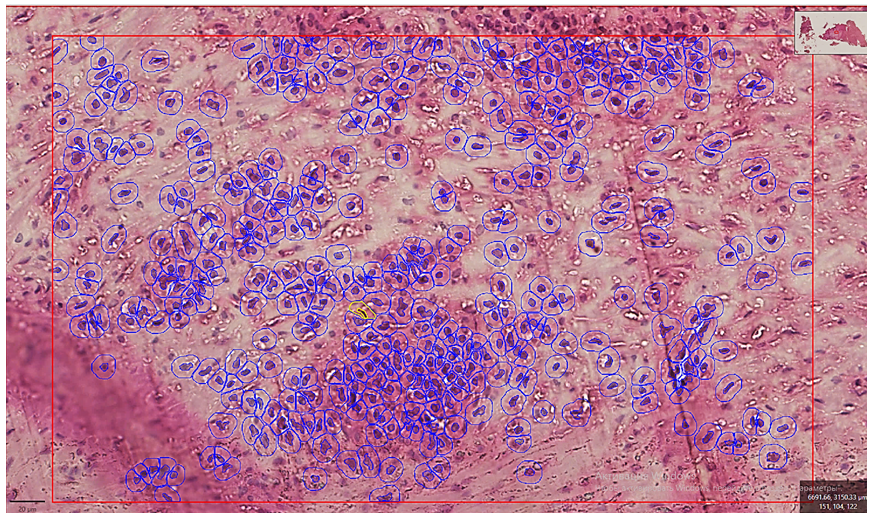 | Figure 3. In tuberculous spondylitis developed under the influence of COVID-19, the number and area occupied by leukocytes within the productive inflammatory focus of bone tissue are presented. The microscopic specimen was scanned using the NanoZoomer (REF C13140-21, S/N000198, HAMAMATSU PHOTONICS, 431-3196 JAPAN). Staining: G.E. Dimensions: 10x20 |
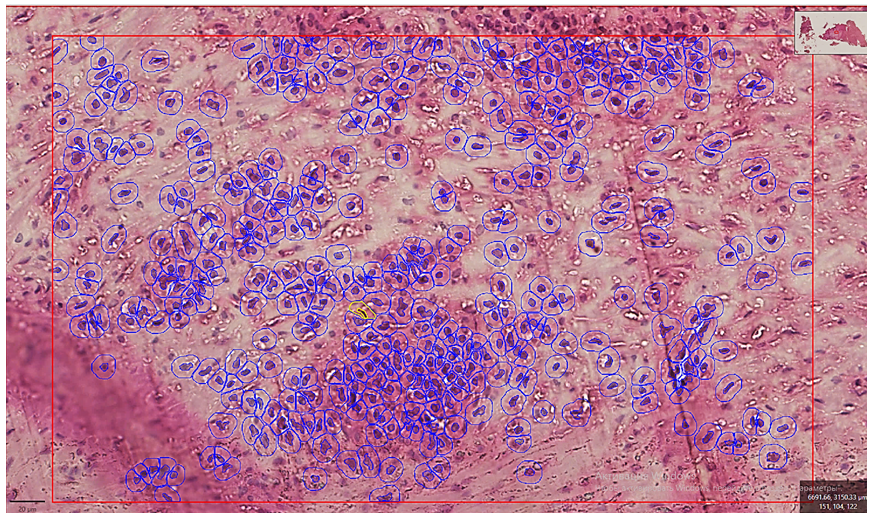
In post-COVID-19 tuberculous spondylitis, simultaneous damage to both bone and soft tissues was noted. This includes foci of aseptic necrosis, proliferative activity of fibroblasts indicative of productive inflammation, increased sparse fibrous connective tissue, interstitial plasma cell infiltration, lymphocytic infiltration surrounding caseous necrosis, and the presence of immature Pirogov–Langhans cells. Additionally, pericyte proliferation around vessels contributes to the expansion of necrotic areas. These findings demonstrate the presence of various mixed reactive tissue changes.Tuberculous Spondylitis in Patients Without COVID-19 Infection: In patients not affected by COVID-19, tuberculous spondylitis typically presents with classical features: caseous necrosis, lymphocytic infiltration, and well-formed Pirogov–Langhans giant cells. Morphometric indicators confirm that the area of tissue damage in these cases is 2.25 times larger compared to post-COVID-19 cases (Figure 4).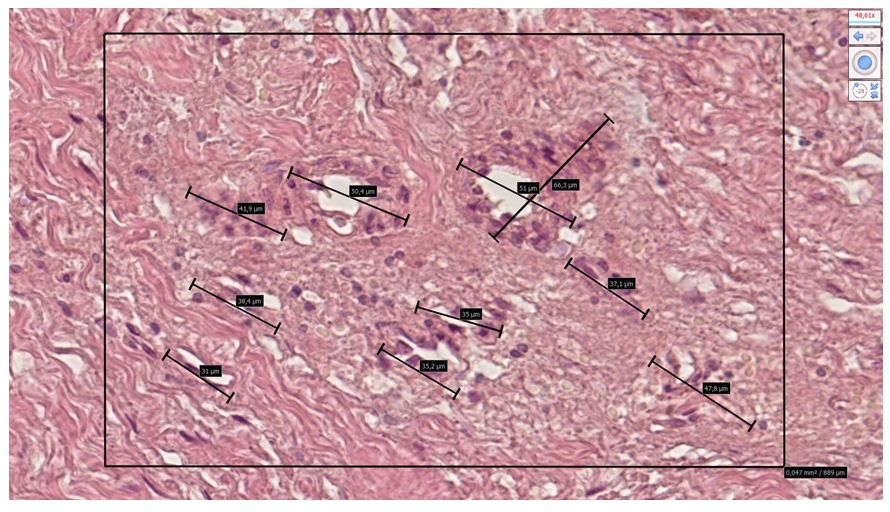 | Figure 4. In the area of chronic productive inflammation of bone tissue, pericyte cell proliferation was observed around the vascular perimeter, and the vessel diameter was measured. The microscopic specimen was scanned using the NanoZoomer (REF C13140-21, S/N000198, HAMAMATSU PHOTONICS, 431-3196 JAPAN). The boundaries of cellular and fibrous structures in the arterial walls were presented with precise dimensions. Staining: G.E. Dimensions: 10x20 |
Degree of Bone Column Preservation: In post-COVID-19 tuberculosis cases, the average preserved area of bone columns in a 0.758 mm² section was 0.0128 mm² (1.68%). In the comparative group (with COVID-19), this value was 0.0526 mm² (6.94%), whereas in classical tuberculous spondylitis it measured 0.0334 mm² (4.41%). These findings demonstrate statistically significant differences, confirming the results of morphological and morphometric analyses.Quantity and Size of Pirogov–Langhans Giant Cells: In post-COVID-19 tuberculosis, the average diameter of Pirogov–Langhans cells was 454.22±2.24 µm, while in classical tuberculosis, it was 176.4±1.75 µm. Additionally, in a 64,000 µm² area, an average of 8.4±1.06 Pirogov–Langhans cells were found in post-COVID-19 granulomas, compared to 4.26±1.21 in classical tuberculosis cases. This indicates a more active formation and greater abundance of Pirogov–Langhans cells in granulomas developed in the context of COVID-19 infection.
5. Conclusions
The conducted comparative morphological and morphometric analysis has convincingly demonstrated that tuberculous spondylitis associated with COVID-19 infection possesses distinct pathogenetic features and histological hallmarks compared to classical tuberculous lesions. A defining characteristic in these cases is the presence of systemic vasculitis involving small-caliber blood vessels, surrounded by zones of extensive caseous necrosis and intense cellular infiltration composed of epithelioid cells and Pirogov–Langhans type multinucleated giant cells.Moreover, the marked proliferation of pericytic and fibroblastic elements, particularly in the post-viral phase, underscores the heightened reparative response and fibrotic transformation associated with COVID-19-mediated immune dysregulation. Morphometric findings further substantiate these observations, with a pronounced reduction in preserved trabecular bone area (1.68% vs. 4.41% in classical cases), and a statistically significant increase in both the number and diameter of giant cells, suggesting intensified immunopathological activity.Of particular note is the presence of mixed-type inflammatory responses, including aseptic necrosis and lymphoplasmacytic infiltration, indicative of overlapping infectious and post-infectious immune mechanisms.Taken together, these findings suggest that COVID-19 significantly exacerbates the pathomorphological progression of tuberculous spondylitis, resulting in more aggressive tissue destruction, complex healing responses, and potentially poorer clinical outcomes. Accordingly, such cases necessitate meticulous histopathological monitoring and the development of tailored, multidisciplinary treatment strategies.
References
| [1] | World Health Organization. Global Tuberculosis Report 2023. Geneva: WHO; 2023. |
| [2] | Siawaya JF, Ruhwald M, Kristensen VS, et al. Host biomarkers for diagnosis of tuberculosis disease. Lancet Infect Dis. 2022; 22(4): e123–e133. |
| [3] | Tadolini M, et al. Active tuberculosis, sequelae and COVID-19 co-infection: First cohort of 49 cases. Eur Respir J. 2020; 56(1): 2001398. |
| [4] | Mousquer GT, Peres A, Fiegenbaum M. Pathology of TB/COVID-19 co-infection: the role of cytokines and immune responses. Int J Infect Dis. 2021; 113: 103–109. |
| [5] | Visca D, Ong CWM, Tiberi S, et al. Tuberculosis and COVID-19 interaction: A review. Pulmonology. 2021; 27(2): 151–165. |
| [6] | Sy KTL, Haw NJL, Uy J. Previous and active tuberculosis increases risk of death and prolongs recovery in COVID-19 patients. Trop Med Infect Dis. 2020; 5(3): 74. |
| [7] | Gao Y, Liu M, Chen Y, Shi S. COVID-19 and TB interaction mechanisms: a comprehensive review. Front Immunol. 2022; 13: 831179. |
| [8] | Luciani F, Sweeney S. Co-infection of SARS-CoV-2 and Mycobacterium tuberculosis: current insights. Infect Dis Rep. 2021; 13(2): 328–336. |
| [9] | Ong CWM, Migliori GB, Raviglione M, MacGregor-Skinner G, Sotgiu G. Combating TB and COVID-19: a joint approach. Eur Respir J. 2022; 59(3): 2102674. |
| [10] | Akhmedov Sh.A., Yunusova Z.Sh. Epidemiology and prevention of tuberculosis in Uzbekistan. Tashkent: Ilm Ziyo; 2021. |
| [11] | Rakhimova M.A. COVID-19 and tuberculosis: analysis of complex epidemiological trends in Uzbekistan. J. “Innovations in Medicine”, 2022; 4(2): 45–50. |
| [12] | Kumar NP, Moideen K, Nancy A, et al. Impact of COVID-19 on immunological profile in tuberculosis. Clin Infect Dis. 2021; 73(12): e4663–e4670. |
| [13] | Gebremariam TH, Desta K, Alemayehu M, et al. Clinical manifestations of TB/COVID-19 co-infection: a meta-analysis. Int J Tuberc Lung Dis. 2023; 27(1): 12–20. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML