Matyakubova Salomat Aleksandrovna1, Yusupova Dilnoza Azadboevna2
1Urgench Branch of Tashkent Medical Academy, Uzbekistan
2Khorezm Branch of the Republican Specialized Scientific - Practical Medical Center of Oncology and Radiology, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Trophoblastic disease is characteristic only of pregnant women of reproductive age and occurs in 0.1-0.25% of all pregnancies. The purpose of study. To develop an algorithm for the pathogenetic treatment of trophoblastic disease in women with a history of undeveloped pregnancy. Material and methods. At the first stage, a retrospective analysis of 199 medical records of women with trophoblastic disease who were treated at the Khorezm branch of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology for the period 2019-2023 was conducted. Results and discussion. As many researchers point out, with age, women experience impaired fertilization, which can lead to the development of cystic fibrosis. Cystic fibrosis is less common in women aged 18 to 20 (8.5%), and in women aged 21 to 30 above (58.8%) and aged 31 to 40 (30.7), it occurs in one in two. Conclusion. A study of the nature of the discrepancy between the size of the uterus and the period of delay in menstruation showed that invasive forms were more common in patients with cystic fibrosis who had uterus sizes larger than expected in terms of the period of delay in menstruation and symptoms of toxicosis. In this regard, this combination is considered an unfavorable prognostic sign of bubble drift.
Keywords:
Trophoblastic disease, Pathogenetic treatment, Human chorionic gonadotropin, Bubble drift, Signs of invasion of the myometrium
Cite this paper: Matyakubova Salomat Aleksandrovna, Yusupova Dilnoza Azadboevna, Development of an Algorithm for Pathogenetic Treatment of Trophoblastic Disease in Women with a History of Undeveloped Pregnancy, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 2869-2874. doi: 10.5923/j.ajmms.20251509.06.
1. Introduction
Trophoblastic disease (TD) is characteristic only of pregnant women of reproductive age and occurs in 0.1-0.25% of all pregnancies. Cystic fibrosis is most often diagnosed among this pathology. According to WHO (2011), on average, there is one cystic fibrosis per 1,000 births, and approximately 2 out of 100,000 women develop chorioncinoma after childbirth and in the same proportion after abortions [1]. Among oncological diseases, TD ranges from 0.01% to 3,6% [2,3]. According to the international histological classification, TD includes: bubble drift (BD) (complete, partial, invasive), choriocarcinoma, trophoblastic tumor of the placental bed, epithelioid trophoblastic tumor. Invasive BD is considered malignant due to its pronounced penetration into the myometrium, as well as its ability to metastasize [4,5].Despite the fact that TD is a relatively rare pathology, the urgency of its problem is quite high, since women of predominantly young childbearing age, sometimes under the age of 25, are susceptible to this disease. The problems of early diagnosis of TD are caused by the aggressive course of the disease, as well as the gloomy prognosis for patients with metastases to the lungs and brain (mortality exceeds 50% and 90%, respectively) [3,6,7].Despite a significant number of studies devoted to this problem, the causes of TB in women with an undeveloped pregnancy remain unclear.The development of new, more effective ways to prevent and treat women with trophoblastic disease, which has arisen as a complication of an undeveloped pregnancy, may become one of the reserves for reducing the morbidity and mortality of women of reproductive age [6,8], which is the main focus of health protection in the Republic of Uzbekistan.The purpose of study was to develop an algorithm for the pathogenetic treatment of trophoblastic disease in women with a history of undeveloped pregnancy.
2. Materials and Methods
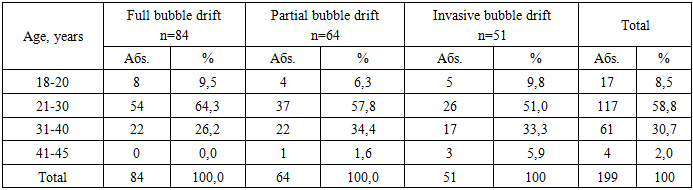
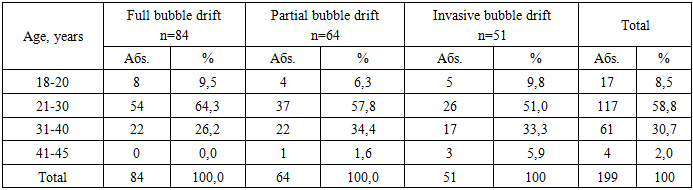
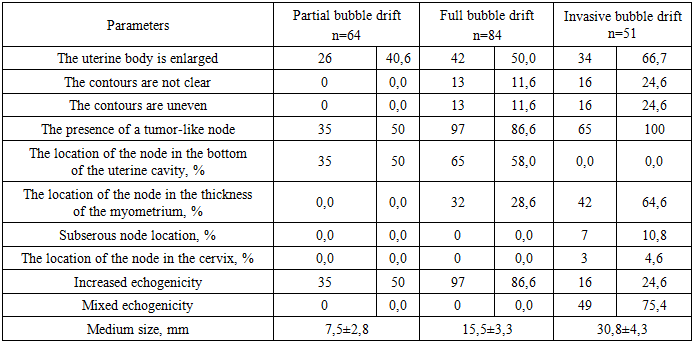
The study was conducted on the basis of the Khorezm branch of the Republican Specialized Scientific - Practical Medical Center of Oncology and Radiology and the Khorezm Perinatal Center.At the first stage, a retrospective analysis of 199 medical records of women with TD treated at the Khorezm branch of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology for the period 2019-2023 was conducted.Selection criteria for the study: diagnosed trophoblastic disease, reproductive age, removal of cystic fibrosis after surgical treatment.Exclusion criteria: diabetes mellitus, autoimmune diseases, diseases of the cardiovascular system, age over 45 years. All women underwent only curettage and the diagnosis of cystic fibrosis was made during histological examination. All the women were examined according to the standards of TD diagnosis and treatment. All patients with TD underwent an assessment of their medical history and clinical symptoms during pregnancy, pelvic ultrasound, and HCG dynamics (1-, 7-, 14 days). Depending on the morphological data, the patients were divided into the following groups: Group I - complete cystic fibrosis - 84 patients (42.2%), group II - partial cystic fibrosis - 64 patients (32.2%), group III - invasive cystic fibrosis - 51 patients (25.6%).The age range of women with TD ranged from 18 to 45 years (the average age was 22.8±0.4 years). The distribution of patients according to age is shown in Table 1.Table 1. Distribution of Trophoblastic disease patients by age
 |
| |
|
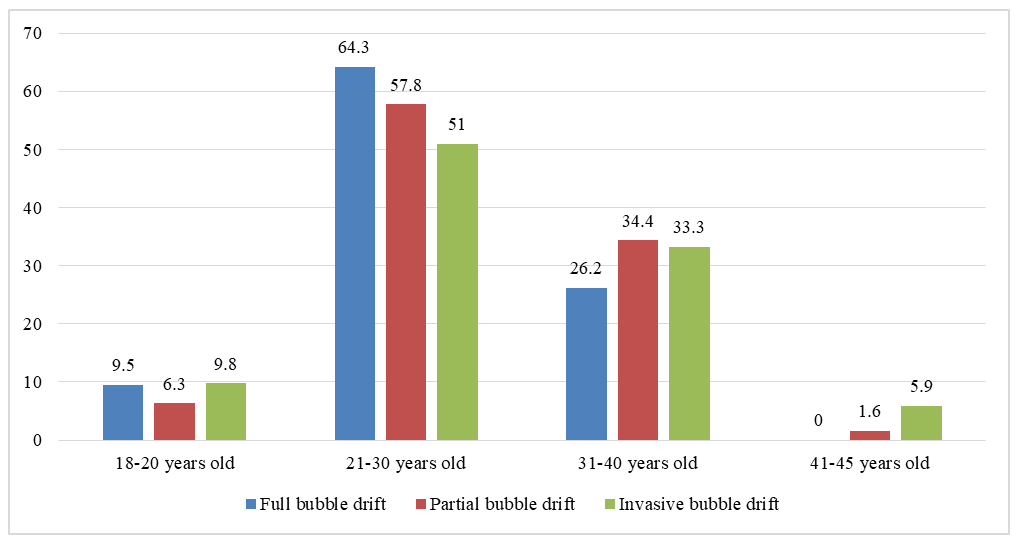
As can be seen from the presented data, TD in most cases occurs in the age range of 21-30 years, while it is 58.8%. It should be noted that in this age period, complete blistering occurs more often than invasive BD and partial BD, but the reliability of the data has not been established (P≥0.005). The lowest incidence of TD is recorded at the age of 41-45 years and 18-20 years (2.0% and 8.5%, respectively). In the age group of 41-45 years, no complete BD was recorded in our studies.All patients underwent ultrasound examination of the small pelvis on an Aloka-1700 device manufactured in Japan using transabdominal and transvaginal sensors of 3.5 and 5.0 Mhz. B-mode and color Doppler mapping mode were used. The localization, size, and structure of the tumor node were clarified, as well as the presence of signs of invasion into the myometrium and features of the uterine vascular bed.An important indicator in the diagnosis is the determination of HCG levels in the peripheral blood during pregnancy. HCG levels were identified by enzyme immunoassay.The content of folic acid in the blood of 68 women with TD after an undeveloped pregnancy in the anamnesis (main group), 41 women with an undeveloped pregnancy (comparison group). They were evaluated in accordance with the attached instructions to ELISA Kite (USA). The reference values ranged from 3.7 to 14.4 ng/ml. Indicators below 3.7 – deficiency, 3.7 – 5.3 ng/ml – borderline indicators, 5.4 – 14.4 ng/ml – normal.In order to achieve this goal, we divided all the surveyed women with TD into 2 groups: the main group consisted of 98 women with a history of TD with an undeveloped pregnancy, which was 49.2%; the comparison group consisted of 101 women with TD without a history of undeveloped pregnancy.In recent years, a specific management system for patients with cystic fibrosis has been developed and is being put into practice, which includes, in addition to comprehensive diagnosis and an individual approach to the choice of therapeutic measures, mandatory systematic monitoring of discharged patients, monitoring of HCG levels, and preventive chemotherapy after successful primary treatment.Pathogenetic treatment was evaluated among 68 women with TD with a history of undeveloped pregnancy, of which 39 patients received folic acid, 1 mg, 3 times a day for 3 months.
3. The Results and Discussion
As many researchers point out, with age, women experience impaired fertilization, which can lead to the development of cystic fibrosis. As can be seen from the diagram, cystic fibrosis is less common in women aged 18 to 20 (8.5%), and in women aged 21 to 30 above (58.8%) and aged 31 to 40 (30.7), it occurs in one in two (Fig. 1).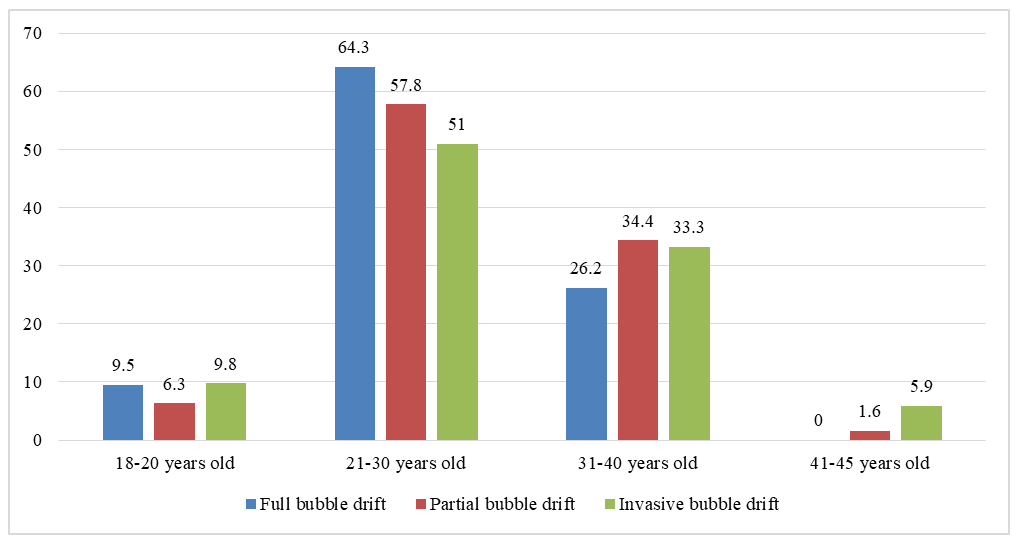 | Figure 1. Age gradation of women depending on the histological type of bubble drift |
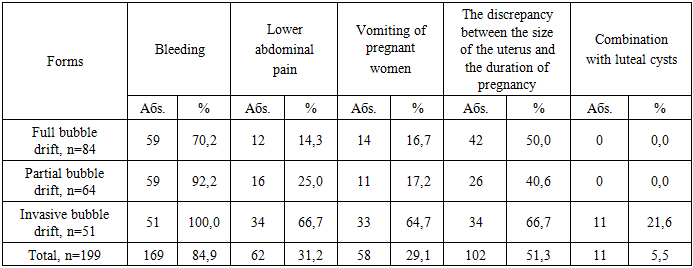
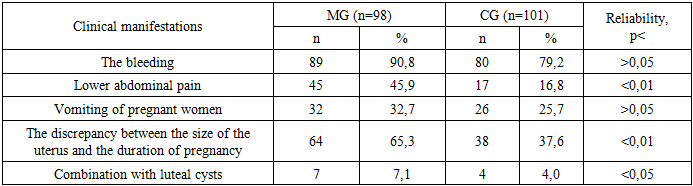
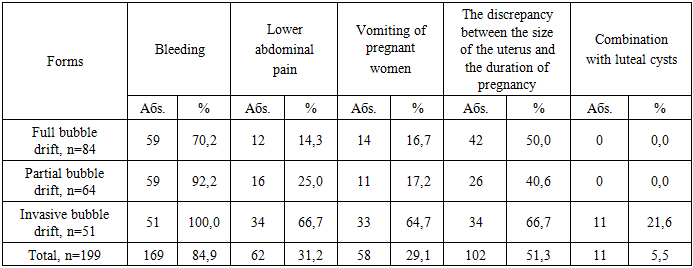
The age range of 18-20 years and 41-45 years is a risk factor for the development of malignant course of cystic fibrosis (χ2=14.52; OR=0.68; p=0.002).The average age of women in the comparison group was 32.01±0.39 years, while women with a history of undeveloped pregnancy were older – 36.6±0.57 years, which is statistically significant (P<0.001). Age over 35 years (RR=0.641; χ2=12.6; P<0.05) is a risk factor for TD in women with a history of undeveloped pregnancy.When calculating the significance of the age of women over 35 years of age as a risk factor for the development of BD, it was found that the prognostic value of this factor for a positive result is +PV=0.69, and for a negative result - -PV=0.72. When calculating the prognostic significance of the age censor in the development of BD in women, it was found that age over 30 is a risk factor, as it has a specificity of 94.2% and sensitivity of 95.1%.When distributing patients with TD according to the form of the disease and the history of undeveloped pregnancy, we found that invasive cystic fibrosis was more common in the main group (28.6% (28 out of 98)) than in the comparison group (22.8%; 23 out of 101;).The presence of complete and partial blistering was less frequently recorded in the main group (34 and 29 out of 98, respectively) compared to the comparison group (40 and 38 out of 101, respectively). Thus, the presence of undeveloped pregnancy in the anamnesis worsens the clinical course of BD and contributes to the development of severe forms of this disease.When analyzing the reproductive history, it was found that pregnancy parity is also a risk factor for the development of BD, while in repeat pregnancies this pathology developed in 75.4% of cases (150 out of 199), while in most cases with invasive BD. We also found that 62.8% (125 out of 199) of abortions preceded the development of BD, while 40.7% (41 out of 199) were spontaneous.When assessing the effect of parity on the risk of developing BD, conducted by analyzing indicators of sensitivity, specificity and odds ratio, it was found that among women with high parity there was a high risk of developing PD, especially the invasive form, which was confirmed by such indicators as Se=74%, Sp=70.8%, P=71.6%, while the ratio The chances or risk of developing BD in women with low parity increased by almost 4.1 times. Depending on the presence of undeveloped pregnancy in the anamnesis in patients with TD, we have not established a dependence on the parity of women.The influence of a history of abortions and spontaneous miscarriages in women with TD was also a risk factor for the development of BD, which was confirmed by statistical analysis of the assessment of specificity, sensitivity and odds ratios: Se=75% and 73%, respectively, Sp=71.2% and 70.9%, respectively, P=71.6% and 72.3%, respectively.When studying the features of menstrual function in patients with cystic fibrosis, it was found that partial and invasive forms of cystic fibrosis occurred more often in patients with late menarche (62.5% and 60.8%, respectively), compared with patients who had it on time and early.In the patients of the main group, the average age of menarche was 14.8±0.12 years, while in the comparison group it was 13.3±0.11 years, which is significantly lower (P<0.05).The development of menarche in women with TD with a history of undeveloped pregnancy over the age of 15 is another risk factor for developing menarche, which is confirmed by such indicators as Se=75.2%, Sp=76.8%, P=78.6%, while the odds ratio or risk of developing menarche in women with menarche aged 15 years and older it increased by almost 7.1 times.The study of the incidence of extragenital diseases among women with BD revealed that the presence of thyroid pathology is a significantly significant risk factor (OR=12.9; 95% CI: 14.5–100.8, p<0.01), as well as overweight and obesity (OR = 19.2; 95% CI: 5.1–72.9; p<0.001), circulatory diseases such as arterial hypertension are among the prognostically significant factors for the development of BD (OR=4.86; 95% CI: 1.61–13.1, p<0.01).In order to identify risk factors and the impact of the presence of extragenital diseases on the development of TD in patients with undeveloped pregnancy in the anamnesis, we analyzed the anamnestic data. The analysis revealed that women in the main group were almost 4 times more likely to suffer from chronic infectious diseases (chronic tonsillitis, chronic sinusitis, etc.).The observed patients did not always have a clearly defined clinical picture. As the results of a prospective study showed, symptoms such as spotting from the genital tract, abdominal pain, toxicosis, and a mismatch in the size of the uterus with the expected duration of pregnancy were the most characteristic. The features of the clinical course of cystic fibrosis, depending on its histological structure, are shown in Table 2.Table 2. Clinical characteristics of the examined women, depending on the form of BD
 |
| |
|
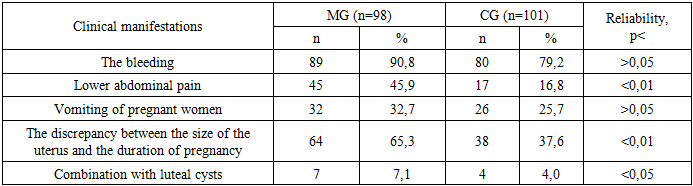
Spotting from the genital tract occurs in 84.9% of patients and was the first sign of the disease. The most characteristic signs were bleeding and a mismatch in the size of the uterus with complete bladder congestion. A combination of bleeding complaints (92.2%) and abdominal pain (25.0%) were presented with a partial form of cystic fibrosis.A certain relationship has been established between the incidence of toxicosis (64.7%) in invasive bladderwort, since cases of toxicosis were significantly more frequent in invasive forms compared with other forms of bladderwort (16.7% and 17.2%, respectively). The presence of all characteristic complaints and the presence of luteal cysts (21.6%) were detected in all cases with invasive cystic fibrosis.An analysis of the clinical characteristics of the women in the main group showed that the presence of undeveloped pregnancy in the anamnesis in women aggravates the clinical symptoms of TD. The data obtained are presented in table 3.Table 3. Clinical characteristics of the examined women, depending on the presence of undeveloped pregnancy in the anamnesis
 |
| |
|
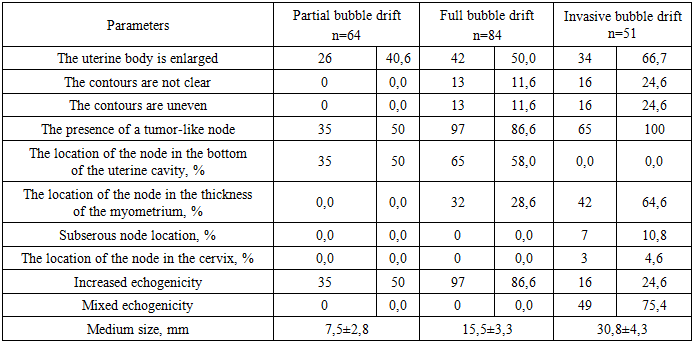
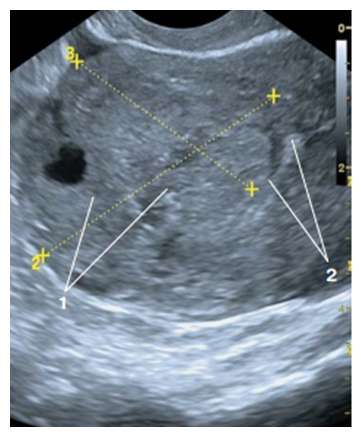
According to ultrasound studies among 64 women with partial BD, in all cases (100%) the uterine body was of normal size, clear and even contours were visualized (Table 4).Table 4. Indicators of ultrasound examination of the uterine body among the examined women, depending on the form of TD
 |
| |
|
In women with complete BD, an increase in the uterine body was noted in 13.4% of cases, and in 11.6% with fuzzy and uneven contours. In 66.7% of cases with invasive BD, the uterine body was enlarged, and deformity of the external contours was found in 24.6% (Fig. 2).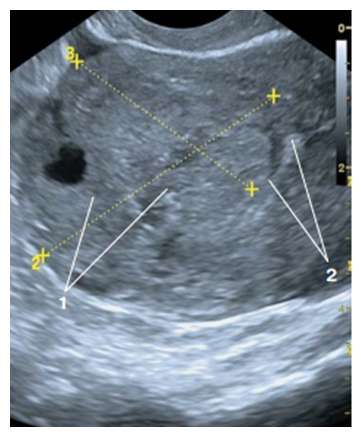 | Figure 2. Patient M., 31 years old. Ultrasound examination – In-mode: nodular formation in the uterine fundus (1) with ingrowth into the uterine region with its deformation |
The presence of a tumor node was recorded in 50% of cases with partial BD, while in 86.6% of cases with complete BD, and in 100% of cases with invasive BD.The localization of the tumor node in the fundus of the uterine cavity was recorded in all cases with partial BD and in 58.0% with complete BD. In invasive BD, tumor-like nodules were localized in the thickness of the myometrium in 64.6% of cases, a subserous location was observed in 10.8% of cases, and in 4.6% in the cervix.It should be noted that in 75.4% of cases, mixed echogenicity is visualized with invasive BD, whereas with partial and complete BD it is not noted. Hyperechogenicity is noted in all cases when a tumor node is found in women with partial and complete BD.In simple BD invasive BD, single tumor-like nodules were noted in 89.2% of cases, in other cases multiple.When patients applied to medical institutions, the majority of women were clinically diagnosed with an abortion in progress (73.4%; 147 out of 199), in every second case of abortion in progress, the morphological picture corresponded to various forms of BD.Thus, a study of the nature of the discrepancy between the size of the uterus and the period of delay in menstruation showed that invasive forms were more common in patients with cystic fibrosis who had uterus sizes larger than expected in terms of the period of delay in menstruation and symptoms of toxicosis. In this regard, this combination is considered an unfavorable prognostic sign of cystic drift (OR = 19.2; 95% CI: 5.1–72.9; p<0.001).
4. Conclusions
1. The incidence of undeveloped pregnancy in the anamnesis in women with TD is 49.2%. Age over 35 years (RR=0.641; χ2=12.6; P<0.05) is a risk factor for TD in women with a history of undeveloped pregnancy. When studying the features of menstrual function in patients with cystic fibrosis, it was found that partial and invasive forms of cystic fibrosis occurred more often in patients with late menarche (62.5% and 60.8%, respectively), compared with patients in whom it occurred timely and early.2. An analysis of the clinical characteristics of the women in the main group showed that the presence of undeveloped pregnancy in the anamnesis in women aggravates the clinical symptoms of TD and contributes to the development of severe forms of this disease. When distributing patients with TD according to the form of the disease and the history of undeveloped pregnancy, we found that invasive cystic fibrosis was more common in the main group (28.6% (28 out of 98)) than in the comparison group (22.8%; 23 out of 101).3. A study of the nature of the discrepancy between the size of the uterus and the period of delay in menstruation showed that invasive forms were more common in patients with cystic fibrosis who had uterus sizes larger than expected in terms of the period of delay in menstruation and symptoms of toxicosis. In this regard, this combination is considered an unfavorable prognostic sign of cystic drift (OR = 19.2; 95% CI: 5.1–72.9; p<0.001).
References
| [1] | Isamuhomedova M.A., Mamadelieva Ja.S., Ataeva S., Koshkina T.A. The Value of Echography in the Diagnostics and Monitoring of Trophoblast Disease Malignant Forms such as Invasive Hydatid Mole and Choriocarcinoma of Uterus // Ul’trazvukovaja i funkcional’naja diagnostika. 2006. № 5. P. 45–49. [in Russian]. |
| [2] | Zakirova, N., Tuguzova, D., Fayzullayeva, N., Inoyatov, S., Karabaeva, M., Yuldasheva, U., Ayubova, H., & Indiaminova, G. (2014). Optimization of bubble drift wives. Doctor’s Herald, 1(1), 89–93. Retrieved from https://inlibrary.uz/index.php/doctors_herald/article/view/4356 [in Russian]. |
| [3] | Mescheryakova L.A. Trophoblastic Tumour. In: Kaprin A.D., Ashrafyan L.A., Stilidi I.S., eds. Gynecological oncology. National manual. M.: GEOTAR-Media; 2019: 273–93. (in Russian). |
| [4] | Chikinev Y.V., Drobyazgin E.A., Dergilev A.P., Sudarkina A.V., Shcherbina K.I., Kachesov I.V., Marchenko A.A. Treatment of chorioncarcinomа with multiple lung metastases (сase report). Journal of Siberian Medical Sciences. 2018; (2): 43-50. (in Russian). |
| [5] | Braga A, Mora P, de Melo AC, Nogueira-Rodrigues A, Amim-Junior J, Rezende-Filho J, Seckl MJ. Challenges in the diagnosis and treatment of gestational trophoblastic neoplasia worldwide. //World J Clin Oncol. 2019 Feb 24; 10(2): 28-37. |
| [6] | Lok C, Frijstein M, van Trommel N. Clinical presentation and diagnosis of Gestational Trophoblastic Disease. // Best Pract Res Clin Obstet Gynaecol. 2021 Jul; 74: 42-52. |
| [7] | Bruce S, Sorosky J. Gestational Trophoblastic Disease. 2022 Jul 18. In: StatPearls [Internet]. // Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29261918. |
| [8] | Pamfamirov Y.K., Demchenko D.V., Korobova P.G. Trophoblastic disease // Tavrichesky medico-biological bulletin. – 2018. – Issue. 21. – Vol 4. – pp. 111-116. (in Russian). |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML