-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(9): 2864-2868
doi:10.5923/j.ajmms.20251509.05
Received: Aug. 17, 2025; Accepted: Aug. 29, 2025; Published: Sep. 2, 2025

The Early Verticalization as a Method of Rehabilitation in Patients with Ischemic Stroke After Thrombaspiration
M. M. Bakhadirkhanov, N. B. Mirzayeva
Republican Scientific Center of Emergency Medical Care, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study evaluated the safety and effectiveness of early graded verticalization after aspiration thrombaspiration in 140 patients with acute ischemic stroke (2022–2024). The main group (n = 70) underwent thrombaspiration plus verticalization within 12 hours; the control group (n = 70) received standard care. Verticalization was feasible in 92.9% of cases, with only 8.6% experiencing transient orthostatic hypotension and no severe complications. Clinical outcomes were superior in the intervention group: functional independence at 90 days was 60.0% vs 42.9% (p = 0.028), recovery was faster, hospital stay shorter, and complication rates lower.
Keywords: Ischemic stroke, Aspiration thrombaspiration, Early rehabilitation, Verticalization, Outcomes
Cite this paper: M. M. Bakhadirkhanov, N. B. Mirzayeva, The Early Verticalization as a Method of Rehabilitation in Patients with Ischemic Stroke After Thrombaspiration, American Journal of Medicine and Medical Sciences, Vol. 15 No. 9, 2025, pp. 2864-2868. doi: 10.5923/j.ajmms.20251509.05.
1. Introduction
- Ischemic stroke (IS) is one of the leading causes of disability and mortality worldwide: in 2021, the number of stroke survivors approached 70 million, and more than 12 million new cases are registered annually [1]. The greatest burden of the disease falls on Central Asian countries, where the age-standardized mortality rate exceeds 70 per 100,000 population [2]. In Uzbekistan, 68,611 cases of stroke were registered in 2022, corresponding to an incidence of 1.94 ‰, which requires significant healthcare resources [3].The introduction of endovascular technologies, primarily aspiration thrombaspiration (direct aspiration), has expanded the possibilities for early reperfusion and made it possible to reduce the risk of severe disability in cases of large cerebral vessel occlusion [4-6]. However, successful recanalization does not guarantee functional recovery without effective rehabilitation during the first days after stroke — the so-called “neuroplasticity window period.” The large randomized AVERT trial was the first to demonstrate the potential of early mobilization within < 24 hours, but under a “high-dose” protocol it also revealed a risk of deterioration in cases of severe stroke [7]. A subsequent dose–response analysis showed that moderate activity (10–20 minutes × 2–3 times/day) was associated with better functional independence [8]. At the same time, the 2024 national and international guidelines on acute stroke still provide only general recommendations, emphasizing the need to personalize the initiation of verticalization [4].One of the promising approaches to individualization is the consideration of autonomic status: low heart rate variability (HRV) and reduced baroreflex sensitivity are associated with orthostatic intolerance and unfavorable stroke outcomes [9,10]. Meanwhile, data on how early verticalization guided by these parameters affects outcomes in patients after aspiration thrombaspiration remain insufficient.Thus, the development and evaluation of a protocol for early, graded verticalization with monitoring of autonomic parameters in patients with IS after thrombaspiration is a relevant task that could improve the effectiveness of early rehabilitation, reduce hospitalization time, and decrease the incidence of complications.
2. Materials of the Study
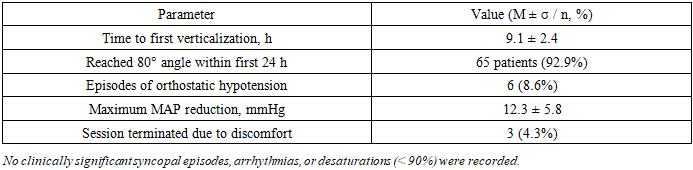
- The study was conducted at the Department of Neurology of the Republican Scientific Center of Emergency Medical Care (RSCEMC) between 2022 and 2024. A total of 140 patients were examined, including 64 (45.7%) males and 76 (54.3%) females, aged 41 to 79 years, all in the hyperacute and acute phases of ischemic stroke (IS) in the carotid and vertebrobasilar territories. Confirmation of the type of cerebrovascular disorder was based on medical history, neurological examination, and neuroimaging data (CT and MRI of the brain). The study population (n = 140) was divided into the following groups. The main group (MG) included 70 (50.0%) patients with ischemic stroke (cardioembolic and atherothrombotic subtypes) who underwent emergency endovascular thrombaspiration.The comparison group (CG) consisted of 70 (50.0%) patients with ischemic stroke who did not undergo emergency endovascular thrombaspiration. Methods: The protocol of early verticalization included initiation within ≤ 12 hours, with a stepwise elevation from 30° to 80° on a robotic tilt table; sessions lasted 10–20 minutes and were performed 2–3 times per day. Control: standard bed rest for ≥ 24 hours. Monitoring: blood pressure (BP), heart rate (HR), oxygen saturation (SpO₂), NIHSS score, and complications. Outcomes: primary outcome — modified Rankin Scale (mRS) 0–2 at 90 days; secondary outcomes — ∆NIHSS at 48 hours, time to independent walking, length of hospital stay, hemodynamics (M ± σ), and incidence of complications.Statistics: Shapiro–Wilk → t/χ²/ANOVA; p < 0.05. It is necessary to present the results according to the following points: Results: Baseline characteristics of the sample; Tolerance of verticalization; Comparison of outcomes (thrombaspiration + early verticalization vs control). Subgroups (age, NIHSS, time to thrombaspiration). Adverse events. Use empirical values.
3. Study Results
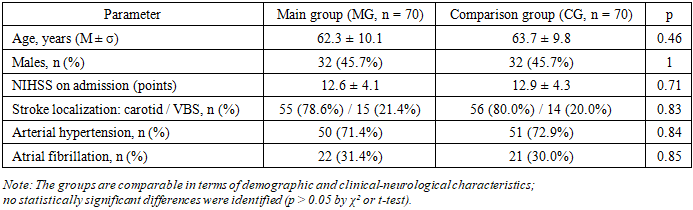
- Table 1 demonstrates that at the time of enrollment, the groups were fully comparable in terms of key demographic and clinical–neurological characteristics. The mean age in the main group (MG) was 62.3 ± 10.1 years, while in the comparison group (CG) it was 63.7 ± 9.8 years (p = 0.46), which excludes age as a potential source of bias. Equality in the proportion of men (45.7% in both groups) and identical baseline stroke severity scores on the NIHSS (12.6 ± 4.1 vs 12.9 ± 4.3; p = 0.71) confirm the validity of the randomization. A similar distribution of risk factors — arterial hypertension, atrial fibrillation, and lesion localization — allows with high confidence to attribute differences in final outcomes specifically to the intervention (thrombaspiration + early verticalization) rather than to confounders.
|
|
|
|
|
4. Discussion
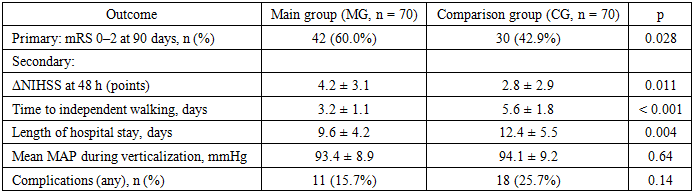
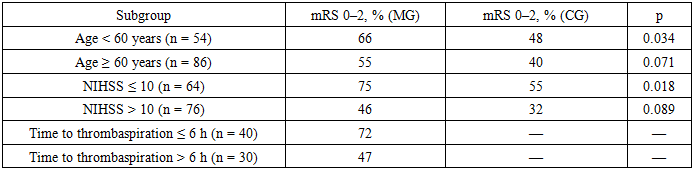
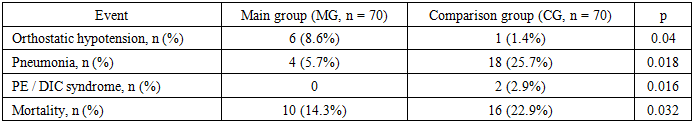
- The findings of this study confirm that early graded verticalization within the first 12 hours after aspiration thrombaspiration in patients with acute ischemic stroke is both feasible and safe, and it contributes to superior functional outcomes. In our cohort, the vast majority of patients successfully tolerated verticalization to an 80° angle with only a small proportion developing transient orthostatic hypotension, which did not lead to severe complications. This aligns with recent reports suggesting that carefully titrated mobilization protocols can minimize hemodynamic risks while harnessing the benefits of early activation of neuroplasticity mechanisms.Our results build on and extend the conclusions of the AVERT trial, which demonstrated that early mobilization could improve outcomes but also highlighted potential harm when applied at excessively high doses. By applying a graded, stepwise approach and integrating continuous monitoring of autonomic parameters, our protocol balanced safety and efficacy. Importantly, the improvement in neurological recovery at 48 hours and the higher rate of functional independence at 90 days indicate that early verticalization is not merely tolerated but may play an active role in enhancing rehabilitation outcomes.The reduction in secondary complications provides further evidence of the value of this intervention. The significantly lower rates of pneumonia and thromboembolic events in the intervention group are consistent with the hypothesis that reducing immobility-associated hypostatic phenomena contributes to improved survival. Mortality at 90 days was also lower in the verticalization group, underscoring the broader systemic benefits of early mobilization.Subgroup analyses reveal that the most pronounced benefits were observed in patients under 60 years of age and in those with lower baseline NIHSS scores, confirming the concept of the "neuroplasticity window." Younger patients and those with less severe strokes likely retain greater reserve capacity for adaptation, which is activated by early mobilization. Nevertheless, even in older patients or those with more severe deficits, trends toward improved outcomes were observed, suggesting potential benefits across the spectrum of ischemic stroke severity.Our study also highlights the importance of minimizing delays before thrombaspiration, as shorter onset-to-recanalization times were associated with better outcomes. This finding reinforces the need for optimizing logistics and stroke pathways in order to maximize the efficacy of both reperfusion therapy and early rehabilitation strategies.While the increase in orthostatic hypotension compared with controls deserves attention, its frequency was modest and manageable under strict monitoring conditions. Considering the substantial reductions in infectious and thromboembolic complications, the net clinical benefit clearly favors early graded verticalization. These results are in line with previous evidence indicating that autonomic dysfunction may predict intolerance to early mobilization; therefore, incorporating autonomic assessments into routine clinical practice may help personalize rehabilitation protocols further.The present study has several limitations. It was conducted in a single center, which may affect generalizability. The sample size, while adequate to demonstrate statistically significant differences in primary outcomes, was insufficient to confirm trends observed in certain subgroups, such as elderly patients or those with high baseline stroke severity. Larger multicenter studies are required to validate these findings and refine patient selection criteria. In addition, long-term outcomes beyond 90 days were not assessed, leaving open the question of whether early verticalization has sustained benefits over time.Despite these limitations, the study provides strong evidence that combining aspiration thrombaspiration with early, stepwise verticalization enhances recovery, reduces complications, and improves survival in patients with acute ischemic stroke. The results support the integration of individualized early mobilization protocols into stroke care pathways and justify further research aimed at optimizing timing, intensity, and patient selection.
5. Conclusions
- 1. Early graded verticalization within ≤ 12 hours after aspiration thrombaspiration is technically feasible and well tolerated. A total of 92.9% of patients reached an 80° angle within the first 24 hours; no clinically significant arrhythmias or desaturations were observed, and episodes of orthostatic hypotension accounted for only 8.6%.2. The combination of thrombaspiration and early verticalization significantly increases functional independence. The proportion of patients with mRS 0–2 at 90 days rose from 42.9% to 60.0% (Δ 17%; p = 0.028), while neurological improvement on the NIHSS over 48 hours was enhanced by 1.4 points (p = 0.011).3. Patients who underwent verticalization regained motor activity faster and were discharged earlier. Time to independent walking decreased from 5.6 ± 1.8 to 3.2 ± 1.1 days (p < 0.001), and length of hospital stay from 12.4 ± 5.5 to 9.6 ± 4.2 days (p = 0.004).4. The greatest effect was observed in patients < 60 years and/or with baseline NIHSS ≤ 10. In these subgroups, the rate of favorable outcomes (mRS 0–2) reached 66–75%, exceeding the control by 18–20 percentage points (p ≤ 0.034).5. The safety profile is favorable: infectious and thromboembolic complications were less frequent, and mortality was lower. Pneumonia decreased from 25.7% to 5.7% (p = 0.018), PE/DIC was not recorded compared with 2.9% in the control (p = 0.016), and 90-day mortality decreased from 22.9% to 14.3% (p = 0.032).6. Despite a slight increase in the frequency of transient orthostatic hypotension (8.6% vs 1.4%; p = 0.04), the overall benefit of the intervention substantially outweighs the potential risks.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML