-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(8): 2656-2659
doi:10.5923/j.ajmms.20251508.51
Received: Jun. 22, 2025; Accepted: Jul. 16, 2025; Published: Aug. 15, 2025

Enzyme Immunoassay of Prostate-Specific Antigen as a Method of Sperm Identification in Forensic Biological Examinations
A. S. Masharipov, D. R. Khudargenova, N. S. Babajanova
Khorezm Branch of the Republican Scientific and Practical Center for Forensic Medical Examination, Urgench, Republic of Uzbekistan
Correspondence to: A. S. Masharipov, Khorezm Branch of the Republican Scientific and Practical Center for Forensic Medical Examination, Urgench, Republic of Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In modern forensic biological practice, the determination of the presence of sperm on physical evidence is one of the most important stages in the investigation of sexual crimes. This is especially true in cases of rape, sexual crimes against minors, as well as in the investigation of cases where there are no obvious signs of violence, but there are suspicions of sexual contact. The possibility of accurate detection and identification of sperm fluid allows not only to confirm or deny the fact of sexual interaction, but also to significantly increase the evidentiary value of the results of forensic biological examinations.
Keywords: Male sperm, Forensic medical examination
Cite this paper: A. S. Masharipov, D. R. Khudargenova, N. S. Babajanova, Enzyme Immunoassay of Prostate-Specific Antigen as a Method of Sperm Identification in Forensic Biological Examinations, American Journal of Medicine and Medical Sciences, Vol. 15 No. 8, 2025, pp. 2656-2659. doi: 10.5923/j.ajmms.20251508.51.
Article Outline
1. Introduction
- Despite the development of molecular biology and the improvement of DNA identification methods, the use of these technologies is possible only if there is a sufficient amount of high-quality biological material. In practice, forensic experts often encounter highly degraded, contaminated, or dried samples, especially if the physical evidence was discovered a long time after the crime was committed [4,5]. In such conditions, it becomes necessary to use highly sensitive and specific methods capable of identifying key biomarkers of sperm even in old or partially destroyed samples [6].One of the most promising approaches in this area is the use of enzyme immunoassay (ELISA) to detect prostate-specific antigen (PSA), a glycoprotein produced by prostate cells [7]. The concentration of PSA in the sperm fluid significantly exceeds its content in other body fluids, which makes it a convenient target for laboratory diagnostics [8]. Under the conditions of a forensic examination, this makes it possible to reliably identify the presence of sperm even in traces of small volumes, as well as in samples exposed to time, temperature, moisture, and other external factors [9].Today, ELISA is widely used in clinical and laboratory diagnostics, in particular, in prostate cancer screening [10]. However, its potential in forensic medicine, especially in the study of dried and long-term stored samples, has not been sufficiently studied [11,12]. While traditional methods such as microscopy, enzymatic acid phosphatase tests, or rapid reactions show limited sensitivity and specificity, ELISA, subject to protocol optimization, can significantly improve the accuracy of detecting traces of semen [13].In addition, the relevance of the study is determined by the need to assess the stability of PSA in semen samples that have been subjected to long-term storage under various conditions. To date, a limited number of studies have been presented in the domestic and foreign literature on the long-term preservation of PSA in biological traces [9,13,14]. Meanwhile, in the practice of forensic experts, situations often arise when biological materials collected during an inspection of the scene arrive at the laboratory months or even years later. This requires understanding how informative PSA analysis can be in such conditions, and up to what shelf life reliable ELISA results can be expected [14].Thus, the need for a systematic assessment of the stability of prostate-specific antigen in dried semen samples stored for up to five years, as well as an analysis of the effectiveness and applicability limits of the ELISA method in a forensic biological laboratory, determines the high scientific and practical significance of this study.The results obtained as part of the work can contribute to optimizing algorithms for expert analysis of biological traces, improving the methodological base of forensic medical laboratories, as well as expanding the arsenal of reliable, sensitive and reproducible methods applicable to complex and non-standard materials, which is especially important in conditions of limited volume or poor preservation of physical evidence [14].
2. The Purpose of the Study
- The purpose of this study is to evaluate the effectiveness and scientific justification of using the method of enzyme immunoassay (ELISA) in forensic biological laboratories to detect the presence of human sperm fluid on physical evidence. In particular, the study aims to determine the diagnostic value of quantifying total and free prostate-specific antigen (PSA) in semen samples dried and stored for a long time. An additional task is to assess the stability of PSA at various storage periods and to identify the sensitivity thresholds of the method in retrospective studies of biological traces.
3. Materials and Methods
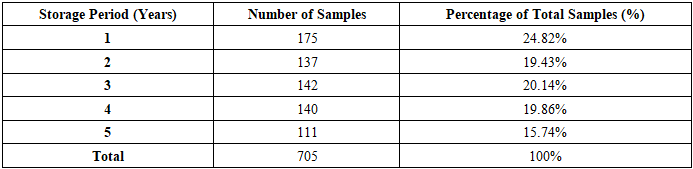
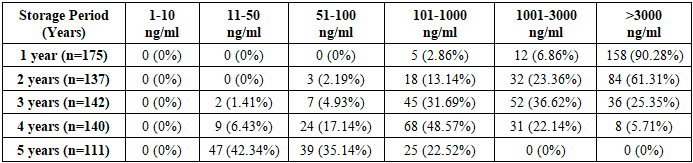
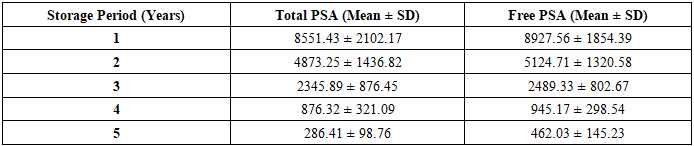
- To evaluate the possibility of using enzyme immunoassay (ELISA) in forensic biological studies, laboratory measurements of the concentration of total and free prostate-specific antigen (PSA) in pre-identified sperm fluid samples dried and stored in laboratory conditions at stable room temperature for one, two, three, four and five years were carried out.The total number of samples examined was 705. The distribution by shelf life was as follows:• 175 samples — with a storage period of 1 year,• 137 — 2 years,• 142 — 3 years,• 140 — 4 years,• 111 — 5 years old.For the analysis, a solid-phase enzyme immunoassay was used using certified commercial diagnostic kits designed for the quantitative determination of total and free PSA. All studies were conducted in accordance with the manufacturer's instructions, with mandatory registration of the results in ng/ml using a photometer. The measurements were carried out in double repetitions to increase the reliability of the data obtained.For the purpose of systematization and subsequent analysis, the quantitative values of PSA were distributed over concentration ranges:• from 1 to 10 ng/ml,• from 11 to 50 ng/ml,• from 51 to 100 ng/ml,• then in increments of 1000 ng/ml — up to ≥50,000 ng/ml.The results are presented in the form of summary tables reflecting both the absolute number of samples in each concentration range and their percentage to the total number of samples examined during the corresponding storage period.Comparative diagrams were constructed to assess the dynamics of changes in PSA concentrations in dried semen samples depending on the storage time. They demonstrate the average levels of total and free PSA for each time interval, which made it possible to visualize the tendency of decreasing antigenic activity as the shelf life increases.Statistical data processing included:• calculation of arithmetic averages, • determination of sample fractions in each interval, • plotting distribution schedules, • assessment of visual trends in antigen degradation.If necessary, statistical analysis methods can be supplemented by checking the significance of differences between groups (for example, using Student's t-test or analysis of variance), which will allow quantifying the identified trends.
4. Results and Discussion
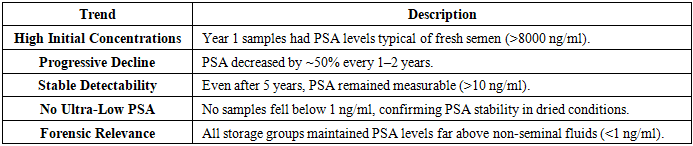
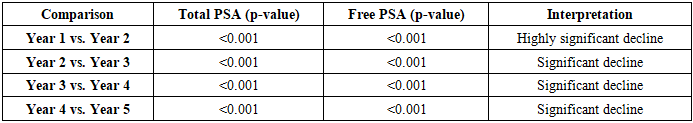
- The results of quantitative determination of total and free prostate-specific antigen (PSA) in dried semen samples stored for one to five years revealed a distinct tendency to decrease the concentration of the marker as the shelf life increased. However, even with five years of storage, PSA concentrations remained at a level significantly higher than those typical for other human biological fluids, such as urine, sweat, or saliva [9,13]. This confirms the high specificity of PSA as a biomarker of sperm fluid.This table summarizes the total number of semen samples analyzed (n=705) and their distribution across different storage periods (1–5 years). It provides the absolute count and percentage of samples per storage group, ensuring a clear understanding of the dataset's composition (Table 1).
|
|
|
|
|
5. Conclusions
- 1. The study showed that the method of enzyme immunoassay (ELISA) has a high sensitivity and specificity in detecting prostate-specific antigen (PSA) in dried samples of sperm fluid. Even with prolonged storage of samples for up to five years, concentrations of total and free PSA remain at levels significantly higher than those in other body fluids such as urine, saliva, or sweat.2. The results obtained confirm that PSA is a reliable and persistent biomarker that retains diagnostic significance even under conditions of degradation and long-term storage. The absence of reported cases with PSA concentrations below 10 ng/ml indicates the stability of the antigen and the validity of its use in forensic biological research.3. The ELISA method makes it possible to reliably identify the presence of semen on physical evidence even long after the alleged incident, which is especially important in conditions of limited access to fresh biological materials or when working with archival files.4. The introduction of ELISA into the routine practice of forensic biological laboratories is advisable: the method provides high reproducibility, is easy to use, is compatible with existing laboratory diagnostic protocols and can be used as a reliable screening tool in investigations of crimes against sexual integrity.5. Thus, the results of this work substantiate the scientific and practical significance of using ELISA with the definition of PSA as a promising approach to the identification of sperm fluid in complex forensic situations, including cases with a long shelf life and degradation of samples.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML