-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(8): 2594-2597
doi:10.5923/j.ajmms.20251508.37
Received: Jun. 22, 2025; Accepted: Jul. 19, 2025; Published: Aug. 6, 2025

Оptimization of Surgical Tactics in Acute Destructive Cholecystitis: A Comparative Analysis of Access Methods and the Use of Modified Drainage
Shomurodov K. A., Daminov F. A., Rakhmanov K. E.
Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents a study on optimizing surgical tactics in acute destructive cholecystitis. A comparative analysis was conducted between traditional and minimally invasive approaches using a newly developed modified drainage device featuring an air chamber for sealing the gallbladder stump. The use of a differentiated approach and innovative drainage significantly reduced the incidence of postoperative complications, shortened the duration of surgery, and improved long-term treatment outcomes. The results confirm the effectiveness of the proposed diagnostic and treatment algorithm and technical innovations in enhancing the safety and quality of surgical care.
Keywords: Acute destructive cholecystitis, Laparoscopic cholecystectomy, Mini-laparotomy approach, Modified drainage, Postoperative complications
Cite this paper: Shomurodov K. A., Daminov F. A., Rakhmanov K. E., Оptimization of Surgical Tactics in Acute Destructive Cholecystitis: A Comparative Analysis of Access Methods and the Use of Modified Drainage, American Journal of Medicine and Medical Sciences, Vol. 15 No. 8, 2025, pp. 2594-2597. doi: 10.5923/j.ajmms.20251508.37.
1. Introduction
- Relevance of the Study. According to the World Health Organization, biliary tract diseases, including acute destructive cholecystitis, rank among the leading causes of acute surgical abdominal pathologies and are a common reason for emergency hospital admissions and surgical interventions [1]. In modern medicine, it is particularly important not only to ensure timely diagnosis and treatment of this condition but also to select the optimal surgical approach that minimizes invasiveness, shortens hospital stays and recovery periods, and reduces the incidence of postoperative complications. Minimally invasive surgical techniques—primarily laparoscopic cholecystectomy—have proven to be an effective alternative to traditional open surgery [2]. However, under conditions of acute destructive inflammation, performing minimally invasive procedures can be technically challenging and associated with an increased risk of complications.The literature review indicates that despite significant progress in the development of minimally invasive surgical techniques for the treatment of acute destructive cholecystitis, several unresolved issues remain. These include the optimal choice of surgical tactics, timing of intervention, and criteria for evaluating the effectiveness of different methods [3]. A number of studies emphasize the need to standardize approaches to diagnosis and treatment in order to reduce variability in clinical decision-making and improve the quality of medical care. The literature highlights the importance of a multidisciplinary approach to patient management, involving not only surgeons but also gastroenterologists, anesthesiologists, and intensive care specialists [4]. This ensures comprehensive evaluation, appropriate preoperative preparation, and effective postoperative monitoring [5]. Thus, accumulated scientific evidence confirms the relevance of further comparative studies and the development of adapted diagnostic and treatment algorithms aimed at optimizing the surgical management of acute destructive cholecystitis under modern clinical conditions [6].Objective of the Study. The aim of the study is to improve treatment outcomes in patients with acute destructive cholecystitis by refining surgical tactics.
2. Materials and Methods
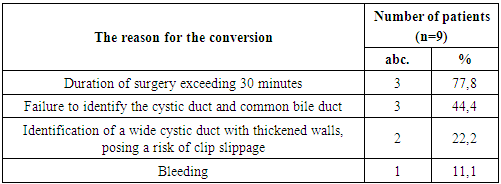
- The study is based on an assessment of surgical treatment outcomes in 201 patients with acute destructive cholecystitis who received treatment in the surgical departments of the Samarkand branch of the Republican Specialized Scientific and Practical Emergency Medical Center (SB RSSPEMC) during the period from 2020 to 2024.The most common comorbidities in both patient groups were grade 2–3 hypertension, coronary heart disease, and grade 2–3 obesity (statistically significant differences compared to the control group, p<0.05). More than one-third of the patients had two or more comorbid conditions [7]. The proportion of patients without any comorbidities ranged from 19.3% to 20.7%.Preoperative instrumental examination followed a standard protocol and included, in addition to general tests (complete blood count, urinalysis, blood biochemistry, ECG, chest X-ray, etc.), abdominal and pelvic ultrasound, as well as endoscopic evaluation of the upper gastrointestinal tract.Depending on the treatment strategy, the patients were divided into groups. From 2020 to 2021, 82 patients (40.8% of the 201) with acute destructive forms of cholecystitis underwent cholecystectomy using only the traditional wide-open approach. These patients formed the comparison group.From 2022 to 2024, 119 patients (59.2% of the 201) with acute destructive cholecystitis underwent cholecystectomy using either the laparoscopic or mini-laparotomy approach. These patients formed the main group.In the comparison group, 17 patients (20.7% of 82) were initially scheduled for laparoscopic cholecystectomy. However, all 17 required conversion, meaning the surgery was completed using the traditional wide-open approach. For the remaining 65 patients (79.3% of 82), the traditional open approach was planned from the outset.The treatment strategy in the main group differed from that in the comparison group by employing a more differentiated approach to selecting the optimal surgical access for cholecystectomy, with a preference for less invasive techniques.According to a developed scoring system, patients who scored 0 to 5 points were recommended for laparoscopic cholecystectomy, while those scoring more than 5 points were advised to undergo cholecystectomy via mini-laparotomy access [8].In the main group, 47 patients (39.5% of 119) were initially scheduled for laparoscopic cholecystectomy. However, due to technical challenges during the procedure and based on diagnostic laparoscopy findings, 9 patients (19.1% of 47) scored more than 5 points and underwent conversion. The reasons for conversion are presented in table 1.
|
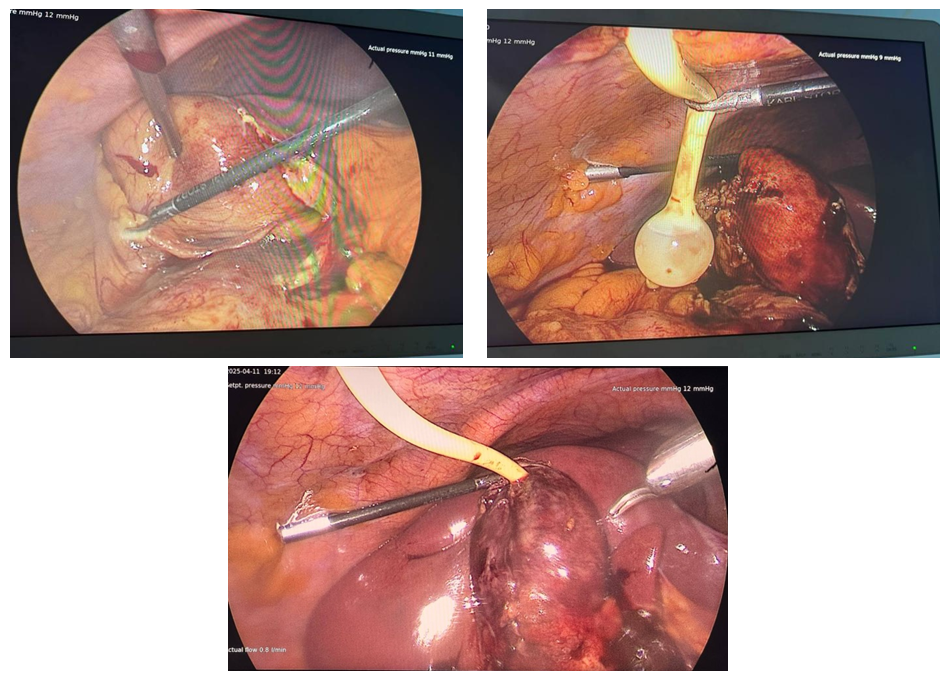 | Picture 1. Stages of Mini-Laparoscopic Cholecystectomy in Destructive Cholecystitis with Drainage of the Gallbladder Stump Using a Special Drainage Catheter with an Air Chamber |
3. Research Results
- The improvement in the choice of surgical tactics for patients with acute destructive cholecystitis, the refinement of surgical technique, reduction of surgical access trauma, and other innovations developed and implemented within this study inevitably impacted the immediate outcomes for this patient group. Compared to 2020–2021, the rate of postoperative complications decreased from 13.4% to 2.5%, i.e., by five times. Complications such as bile leakage occurred twice less frequently, and severe complications like bile peritonitis and bile duct injuries were completely absent.Long-term outcomes were analyzed in 129 (64.2%) of the 201 operated patients with acute destructive cholecystitis.One of the main indicators characterizing the effectiveness of surgical intervention in acute destructive cholecystitis is the presence of postcholecystectomy syndrome (PCS). The study of PCS types was based on the classification by A.A. Shalimov (1988).Patients with the organic form of PCS were more frequent in the comparison group (10%) than in the main group (2.6%). The sharp decrease in the number of PCS cases with and without disruption of bile duct integrity since 2021 is associated with the transition to a differentiated approach to the surgical treatment of patients with acute destructive cholecystitis.The use of our specially designed drainage catheter with an air chamber during laparoscopic cholecystectomy for destructive cholecystitis has improved surgical treatment outcomes in both the early and long-term postoperative periods.
4. Conclusions
- The developed and optimized diagnostic and treatment algorithm for managing patients with acute destructive cholecystitis, which includes a scoring assessment of disease severity based on clinical data, ultrasound findings, and diagnostic laparoscopy, allowed a justified choice of the most rational surgical intervention method. In the main group, this algorithm enabled laparoscopic cholecystectomy in 31.9% of cases and mini-access cholecystectomy in 68.1%, contributing to a significant reduction in operative time from 66.5±4.9 to 42.1±2.9 minutes (t = 4.23; p < 0.001). Thus, the use of the algorithm improved the effectiveness of surgical treatment by individualizing access selection according to disease severity and objective diagnostic criteria.The evaluation of a modified drainage device with an air chamber, ensuring the hermetic sealing of the gallbladder stump during laparoscopic cholecystectomy, demonstrated significant improvement in surgical care quality, reflected by a reduction in early biliary complications from 7.3% to 2.5%. These results indicate that the device increases procedural safety and promotes better postoperative recovery.The developed diagnostic and treatment algorithm combined with the use of a special air-chamber drainage device, applied in cases with a long gallbladder stump, led to a decrease in early postoperative complications from 13.4% (11 patients in the comparison group) to 2.5% (3 patients in the main group) (χ² = 4.954; df = 1; p = 0.027), as well as a reduction in the incidence of postcholecystectomy syndrome (PCS) during the long-term follow-up from 24.0% (12 patients in the comparison group) to 6.3% (5 patients in the main group) (χ² = 4.692; df = 1; p = 0.031).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML