Gulrukh Karimova Komilovna, Tolibova Komila Obid kizi
The Department of Obstetrics and Gynecology in Bukhara State Medical Institute Bukhara, Uzbekistan
Correspondence to: Gulrukh Karimova Komilovna, The Department of Obstetrics and Gynecology in Bukhara State Medical Institute Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Introduction: When asked by the history taking method, whether close relatives of pregnant women with GDM had inherited diabetes mellitus, where cases of DM were diagnosed (58.2% of pregnant women with a history of GDM, 57.4% of patients with GDM). Methods. The study included general clinical, biochemical (C-reactive protein, ferritin, D-dimer, APTT, ketone, homocysteine, glucose, creatinine, LDH, LII, PGTT, glycated hemoglobin), hormonal (leptin, C-peptide, 25 (ON)D, HOMA-IRCP, HOMA-Islet, methods of correlation and statistical research. Conclusion: In our studies, the risk factors for the development of gestational diabetes were: obesity of the 1st degree (43%), 2nd degree (21.5%) and overweight (12%), women with hereditary diabetes mellitus (57.4%), the presence of a large fetus history (80.9%), preeclampsia (66.2%), polyhydramnios (35.3%), with a condition after COVID-19, complicated by transient diabetes (14.7%).
Keywords:
Leptin, C-peptide, Pregnant with diabetes, Blood glucose, 25 (ON)D
Cite this paper: Gulrukh Karimova Komilovna, Tolibova Komila Obid kizi, Gestational Diabetes: Causes and Diagnosis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 8, 2025, pp. 2590-2593. doi: 10.5923/j.ajmms.20251508.36.
1. Introduction
When studying the state of somatic diseases of pregnant women in the study groups in pregnant women with GDM and GDM in history, chronic pyelonephritis occurred in 32.8% and 30.9%, thyroid disease 32.8%, 35.3%, obesity -75% and 64 .2% in the two groups, respectively.According to the analysis of blood in the case histories of patients in groups, anemia was observed in an average of 61.45% of patients.Based on the above data, using the Microsoft Excel 2010 program, a series of variations was built to find M±m indicators of the degree of dependence of these features, their correlation levels were studied by the Spearman method. Diabetes mellitus has become a global problem among pregnant women around the world, especially during the pandemic, and is one of the pathologies that contribute to a sharp increase in obstetric and perinatal complications and the spread of the disease at a young age. Gestational diabetes mellitus (GDM) is inextricably linked with metabolic disorders and monitoring of obstetric and perinatal complications [3,18]. The International Diabetes Federation estimates that the global prevalence of GDM is up to 14%, with one in seven babies affected, including 18 million births with adverse complications such as maternal and fetal death, and will depend on the methods used and environmental factors [6,11].The lack of treatment for GDM can pose a serious threat to the life of both the mother and the child [16,17], for example, the risk of preeclampsia or eclampsia for the mother increases by 8 times. The frequency of risk factors such as hypertension associated with pregnancy is also increasing due to adaptive anomalies, macrosomia of infants, which forces specialists to use surgical interventions: caesarean section, etc. The majority of women with GDM, almost 50%, develop type 2 diabetes at an older age, and the ancestors of mothers with GDM had an increase in blood glucose levels and changes in the lipid profile of amino acids that stimulate insulin secretion and growth factors [9,15]. As a result of these disorders, the development of type 2 diabetes in children and adolescents increases by 6 times [8,14].In most cases, in pregnant women, the disease is accompanied by mild hyperglycemia and the absence of obvious clinical symptoms, so the peculiarity of GDM is that it is difficult to diagnose with a late manifestation. In some cases, the diagnosis of GDM in infants is detected retrospectively or is not determined at all by the phenotypic symptoms of diabetic fetopathy [1,12]. For this reason, in many countries (especially among the population where type 2 diabetes is common), mass active screening is carried out to detect this pregnancy complication [7,13].In our country, today there are no standards for early screening for GDM that could fully justify itself, and current issues such as early detection and prognosis have not been fully resolved. Currently, the mechanisms of the origin of GDM are not well understood, and therefore, scientific research is underway to identify early screening biomarkers associated with GDM [2,4]. However, the interaction of identified markers with overt and latent clinical signs of GDM has not been clearly demonstrated. For this reason, the search for predictors of GDM and complications is relevant [5,10].It is also necessary to develop models for effective detection of women with gestational diabetes, timely screening and prevention methods, which are of particular importance in the management of gestational diabetes and help improve health outcomes. GDM is not a cure, but prevention is a priority both in terms of health and economics. In a non-diabetic woman at risk of GDM, even a small decrease in glucose levels can be an important factor for pregnancy and the health of future generations.
2. Methodology
The study included general clinical, biochemical (C-reactive protein, ferritin, D-dimer, APTT, ketone, homocysteine, glucose, creatinine, LDH, LII, PGTT, glycated hemoglobin), hormonal (leptin, C-peptide, 25 (ON)D, HOMA-IRCP, HOMA-Islet, methods of correlation and statistical research.
3. Results
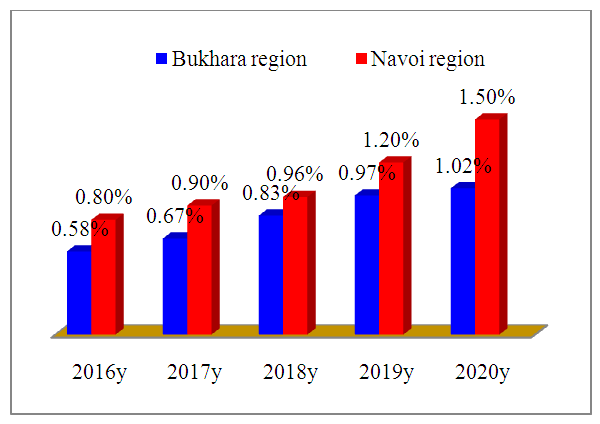
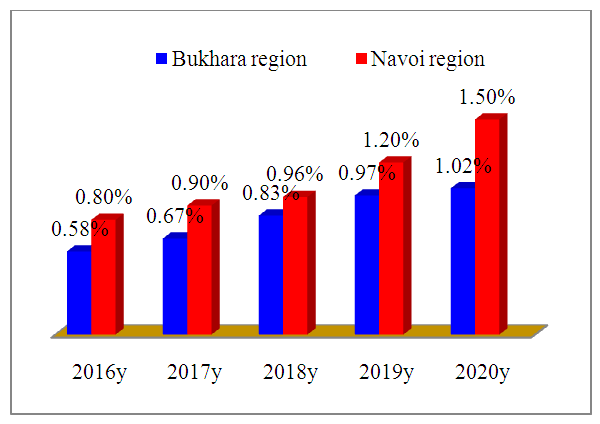 | Picture 1. Incidence rate of GDM in Bukhara and Navoi regions (%) |
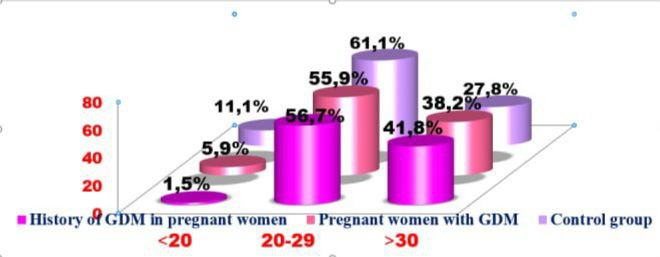
The selection criterion for patients was pregnant women with a high risk of GDM with a gestational age of 22–38 weeks, with various obstetric and somatic complicated anamnesis.When collecting anamnesis, the place of residence of patients was taken into account, since the annual increase in metabolic diseases directly correlates with a decrease in physical activity. It was revealed that 20 (30.2%) pregnant women with GDM live in the village, and in the control group 28 (77.8%). Pregnant women with GDM living in the city amounted to 48 (69.8%), in the control group -8 (22.2%).It can be seen that GDM is relatively high in areas with stress factors such as metabolic diseases and conditions associated with low mobility and modern development.We also paid special attention to the age status of the patients. As can be seen from Picture 3, the incidence of GDM was higher in pregnant women aged 20–29 years due to gestational age and a higher proportion of pregnant women with a history of GDM (56.7% and 55.9%, respectively).Pregnant women aged 30 years and older accounted for 38.2% of pregnant women with GDM and 41.8% of pregnant women with a history of GDM. For comparison, healthy pregnant women in the control group were 11.1% at the age of 20 years, 61.1% at the age of 20-29 years and 27.8% at the age of 30 years (Pic. 2).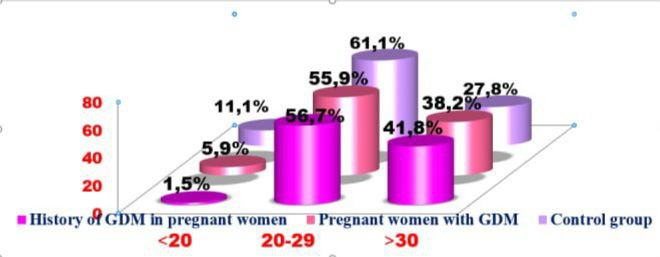 | Picture 2. Age indicators of pregnant women (%) |
Analyzed clinical and anamnestic data and indicators of reproductive health of women with hyperglycemia in the blood. It became known that out of the analyzed data of 68 pregnant women with GDM complications, all of them were diagnosed on the basis of clinical and anamnestic (obesity, large fetus, antenatal fetal death, polyhydramnios, fetal malformation), instrumental and diagnostic data (ultrasound). In pregnant women in Bukhara and Navoi regions in 2016, it was observed in 0.58/0.8% of cases of GDM, in 2017 - in 0.67/0.9% of cases of GDM, in 2018 - in 0.83 /0.96% of GSD cases, in 2019 - in 0.97/1.2% of GDM cases and in 2020 - in 1.02/1.5% of GDM cases (Pic. 1). As can be seen from the figure, the frequency of detection of GDM is more often diagnosed and occurs in the Navoi region in comparison with the Bukhara region. In the control group there were 13 firstborns and 23 second children, respectively 36.1% and 63.9%.Also, by taking an anamnesis, it was determined whether the pregnant woman had a hereditary DM disease or not. The results of the survey showed that close relatives of pregnant women with a history of GDM accounted for 58.2%, and pregnant women with DM had hereditary GDM disease in 57.4%. In the control group, 16.7% had DM in close relatives.However, in pregnant women with a history of GDM and in women with GDM in this pregnancy in the control group without DM, the rates were 41.8%, 42.6 and 83.3%, respectively (Pic. 3). | Picture 3. Patients with hereditary diabetes |
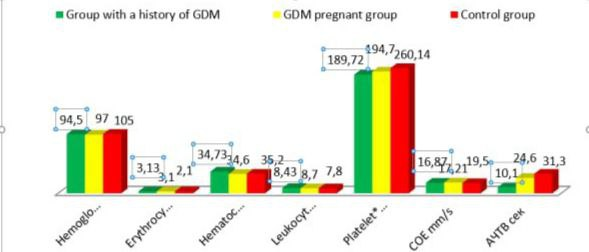
Thus, based on the data obtained, the role of the above risk factors (obesity BMI ≥30, overweight index BMI 25-30, heredity, polyhydramnios, complicated obstetric anamnesis, large fetus) in early development in pregnant women with GDM should be noted.We performed basic routine laboratory tests for pregnant women with GDM and then analyzed them: blood, urinalysis, fasting and loading oral glucose tolerance test (OGTT), glycated hemoglobin index, PTI and coagulogram containing thrombotest, urinalysis for glucose, urea, creatinine.Particular attention was paid to the study of biochemical analysis of glycated hemoglobin and blood sugar in women who had a history of GDM in previous years (67 pregnant women), 68 pregnant women with GDM (identified during our study) and 36 pregnant women in our control groups.The purpose of conducting biochemical studies of all fractions of bilirubin, ALT and AST enzymes, total protein, urea and creatinine was to determine the degree of liver and kidney dysfunction, was to determine the characteristic features for GDM in pregnant women.To identify placental and fetal circulatory disorders associated with the development of complications, we also studied specific analyzes in dynamics, such as homocysteine, leptin, C-peptide, D-dimer and 25 (OH)D. When septic complications occurred, the following indicators were included in the studies as C-reactive protein and procalcitonin.Of the 68 pregnant women, only 26 received 6 to 10 units of insulin per day on the recommendation of an endocrinologist.Pregnancy is accompanied by an increase in hematopoiesis, an increase in plasma volume by 2.5-3 times, respectively, with a change in the composition of formed elements and hemoglobin.The obtained results show that the peripheral blood parameters of pregnant women with a physiological shift (n=36) significantly differ from those of pregnant women with GDM (n=68).In both groups, both healthy and pregnant women with GDM showed a decrease in the levels of erythrocytes and hemoglobin compared to the reference values.Compared to the generally accepted norms, erythrocytes decreased by 0.7 and 0.4 (2.8 and 3.1), and hemoglobin in both groups decreased by 15.2 and 7.2 (98 and 113.2 g/l), respectively.The color index, which reflects the average concentration of hemoglobin (Hb) protein in one erythrocyte, ranged from 0.8 to 1.0 without anemia. A decrease in this indicator was observed in different conditions: with various forms of anemia, for example, iron deficiency, anemia after hemorrhoids, often with chronic diseases of internal organs (Pic. 4).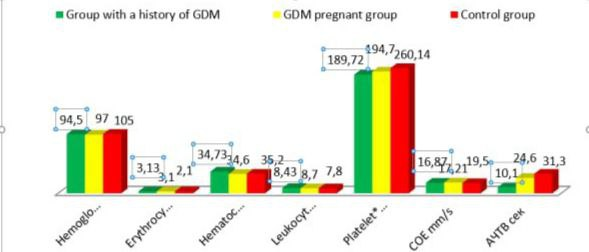 | Picture 4. Results of laboratory blood tests |
In the study of the white part of the blood (leukocytes) in the group of pregnant women with GDM, this indicator was slightly higher than in healthy people (8.7±0.3; 7.8±0.24×1012). In our studies, the risk factors for the development of gestational diabetes were: obesity of the 1st degree (43%), 2nd degree (21.5%) and the growth of overweight (12%), women with hereditary diabetes mellitus (57.4%), the presence a large fetus in history (80.9%), preeclampsia (66.2%), polyhydramnios (35.3%), with a condition after COVID-19, complicated by transient diabetes (14.7%).The negative impact of gestational diabetes on both the mother's body and the fetus, with the subsequent development of DF and insulin resistance of the fetus.
4. Conclusions
1. In our studies, the risk factors for the development of gestational diabetes were: obesity of the 1st degree (43%), 2nd degree (21.5%) and overweight (12%), women with hereditary diabetes mellitus (57.4%), the presence of a large fetus history (80.9%), preeclampsia (66.2%), polyhydramnios (35.3%), with a condition after COVID-19, complicated by transient diabetes (14.7%).2. The negative impact of gestational diabetes on both the mother's body and the fetus, with the subsequent development of DF and insulin resistance of the fetus. They were reflected in the following indicators: an increase in the level of glycated hemoglobin (HbA1c) by 2–2.3 times, insulin resistance of hormonal indicators to C-peptide by 92.4%, homocysteine (a marker of folate status) by 12% and an increase in the predictor of metabolic leptins on average 65% (р<0.001) of the LDH level, LII by 10% relative to the reference values.3. To prevent complications in the mother and fetus, based on clinical and laboratory data and predictors of the development of gestational diabetes mellitus (C-peptide, leptin, an increase in BMI up to 450 mg up to 20 weeks, 1.5 times more than normal pregnancy) indicates a complicated course of GDM and Insulin dose adjustment should be immediately introduced together with an endocrinologist; in order to prevent maternal and perinatal complications, an algorithm based on a computer program has been optimized.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interests
All the authors declare no conflict of interest.
CRediT Authorship Contribution
The authors would like to thank the Bukhara State Medical Institute for supporting this study and providing the data through the Bukhara State Medical Institute Central Library.
Ethics Approval and Consent to Participate
Not applicable.
ACKNOWLEDGEMENTS
The authors are grateful for the support and helpful comments provided by the department of Obstetrics and gynekology in Bukhara State Medical Institute, as well as other experts consulted as part of the process. We would also like to thank Bukhara city maternity complex for her assistance in creating the figure for our literature search.
References
| [1] | Azizova, D. M., Mavlyanov, I. R., Sabirova, R. A., Kulmanova, M. U., Soliev, A. B., & Zharylkasynova, G. Z. (2020). Developing new approaches to hyperlipidemia correction taking into account changes in fatty acids structure of blood serum. Health Risk Analysis, 2020(2), 152-163. doi:10.21668/health.risk/2020.2.17.eng. |
| [2] | Badritdinova, M. N., Razhabova, G. K., Akhmedova, S. M., & Akhmedova, G. I. (2020). Peculiarities of a pain in patients with ischemic heart disease in the presence of individual combines of the metabolic syndrome. International Journal of Current Research and Review, 12(24), 146-150. doi:10.31782/IJCRR.2020.122426. |
| [3] | Davlatov S. S., Khamdamov B. Z., & Teshaev Sh. J. (2021) Neuropathic form of diabetic foot syndrome: etiology, pathogenesis, classifications and treatment (literature review). Journal of Natural Remedies. Vol. 22, No. 1(2), – P. 147-156. |
| [4] | Gulrukh K. Karimova. Early biochemical markers and screening diagnosis of Gestional diabetes mellitus and its prevention during pandemic period / Gulrukh K. Karimova., Gulchekhra A.Ikhtiyarova., Nigora Kh. Muminova. // Journal of Natural Remedies -2021. - №1(1). -Volume 22, - ISSN: 2320-3358, ISSN: 0972-5547–P. 17-26. |
| [5] | Gulrux K. Karimova. An individual approach to the management of gestational diabetes / Gulrux K. Karimova., Nilufar O. Navruzova., Shahodat N. Nurilloyeva. // European Journal of Molecular & Clinical Medicine -2020. -№02. -Volume 07, - ISSN 2515-8260–P. 6284-6291. |
| [6] | Ikhtiyarova, G. A., Dustova, N. K., Kudratova, R. R., Bakhramova, S. U., & Khafizova, D. B. (2021). Pre-course training of women with reproductive loss of fetus in anamnesis. Annals of the Romanian Society for Cell Biology, 25(1), 6219-6226. Retrieved from www.scopus.com. |
| [7] | Ikhtiyarova, G.A. Causes of fetal loss syndrome at different gestation times / Ikhtiyarova G.A., Iroda Tosheva, Nargiza Nasrullayeva // Asian Journal of Research. - 2017. - № 3 (3). - Р. 32-41. |
| [8] | Komilovna, K.G. (2022) Diagnostics of pregnant women with gestational DIABETES. Journal of Pharmaceutical Negative Results, 13, DOI: 10.47750/pnr.2022.13.S08.408. www.scopus.com. |
| [9] | Navruzova, N. O., Karshiyeva, E. E., Ikhtiyarova, G. A., Hikmatova, N. I., Olimova, N. I., & Muminova, N. K. (2021). Clinical and laboratory markers forecasting of cervical diseases and its prevention. Annals of the Romanian Society for Cell Biology, 25(4), 13098-13110. Retrieved from www.scopus.com. |
| [10] | Rakhmatillaevna, K. F. (2020). Diagnostic value of salivator cytokines in dental diseases in children with diabetes mellitus type 1. European Journal of Molecular and Clinical Medicine, 7(3), 1518-1523. Retrieved from www.scopus.com. |
| [11] | Rakhmatillaevna, K. F. (2020). Diagnostic value of salivator cytokines in dental diseases in children with diabetes mellitus type 1. European Journal of Molecular and Clinical Medicine, 7(3), 1518-1523. Retrieved from www.scopus.com. |
| [12] | Iktiyarova G.A. Differential methods of pregnancy termination in women with antenatal fetal death at various gestational ages/Iktiyarova G.A. Dis.doc.med.nauk. - 2019. S- 209. |
| [13] | Ikhtiyarova G.A., Karimova G.K., Navruzova N.O. Screening diagnosis of gestational diabetes // Tibbietda yangi kun – 2020. No. 1 (29) pp. 220-223. |
| [14] | Karapetyan T.E. Genital mycoplasmas and pregnancy outcomes / T.E. Karapetyan, V.V. Muravyeva, A.C. Ankirskaya // Problems of reproduction. - 2012. No. 3. - Pp. 88-93. |
| [15] | Karimova, G.K. Screening and Diagnosis of Gestational Diabetes / G.K. Karimova, G.A. Iktiyarova, and N.O. Navruzova // Tibbiyotda yangi kun. - 2020. - No. 1 (29). - Pp. 220-222. |
| [16] | Muminova N.X. Prevention of pyoin-septic complications in the postpartum period/ Muminova N.X. // Experiment in Surgery and Oncology. - 2019. - C. 56-59. |
| [17] | Navruzova, N.O. Modern diagnostic methods for early detection of diseases of the cervix / N.O. Navruzova, G.A. Ihtiyarova, G.K. Karimova, U.O. Navruzova, I.B. Shukurov, Kh.I. Amanova // Vestnik vracha. - 2019. - No. 4. - P. 77-82. |
| [18] | Navruzova, N.O. Modern Approaches to the Diagnosis of Cervical Pathology / N.O. Navruzova, G.K. Karimova, and G.A. Iktiyarova // Sport and Medicine. - 2020. - No. 1. - Pp. 74-77. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML